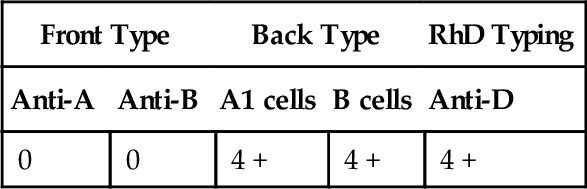
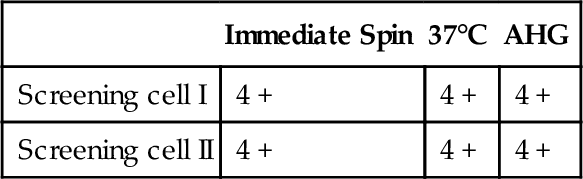
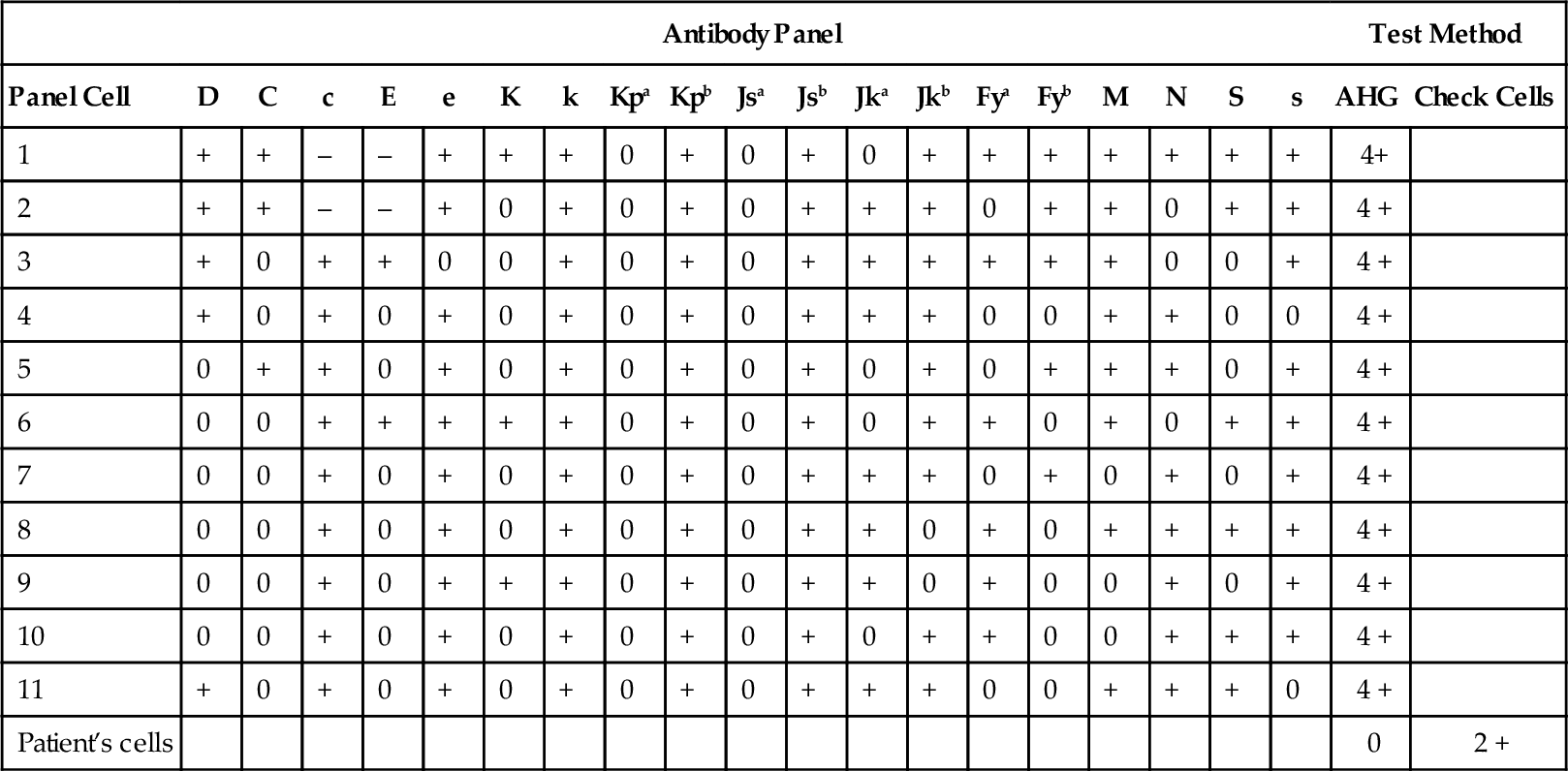
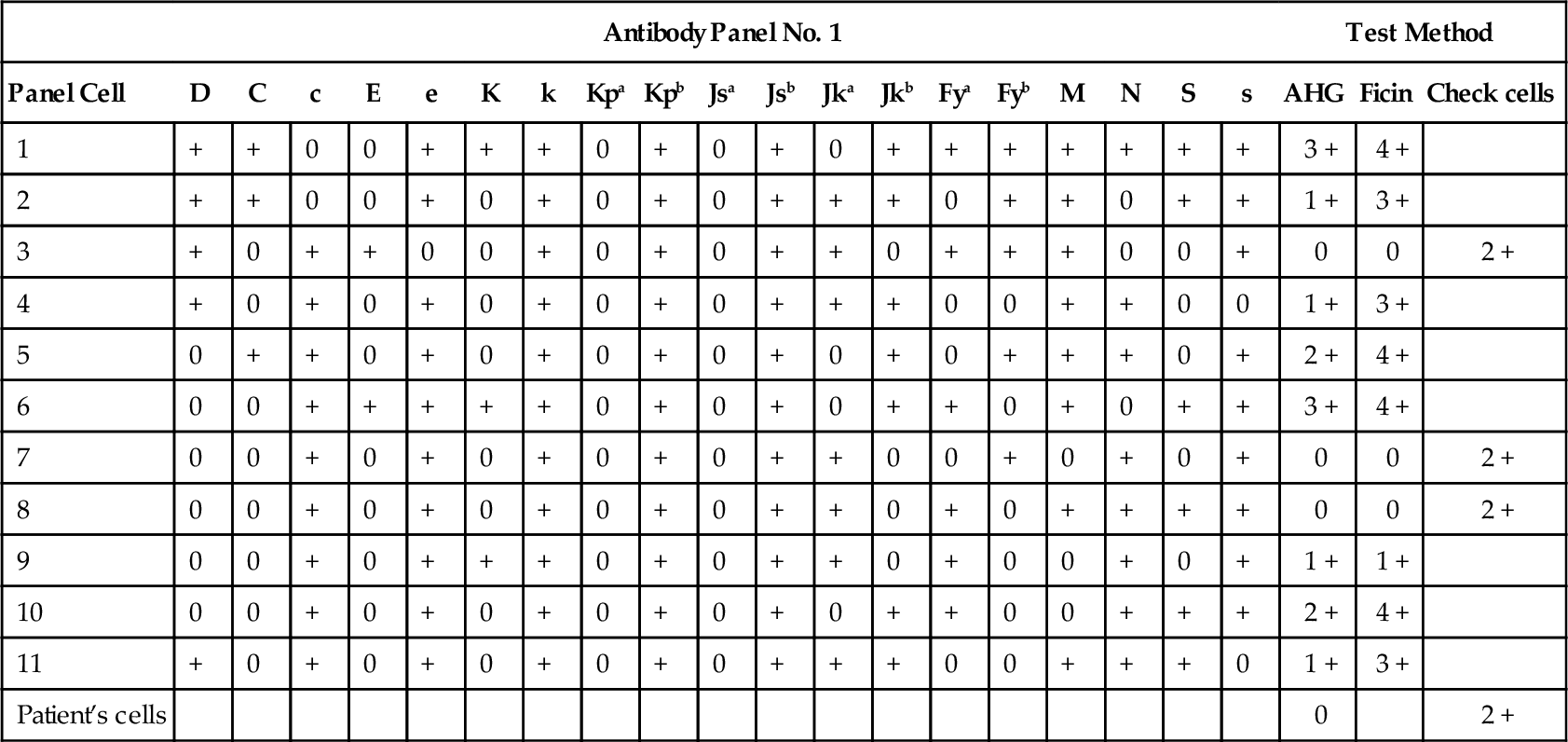
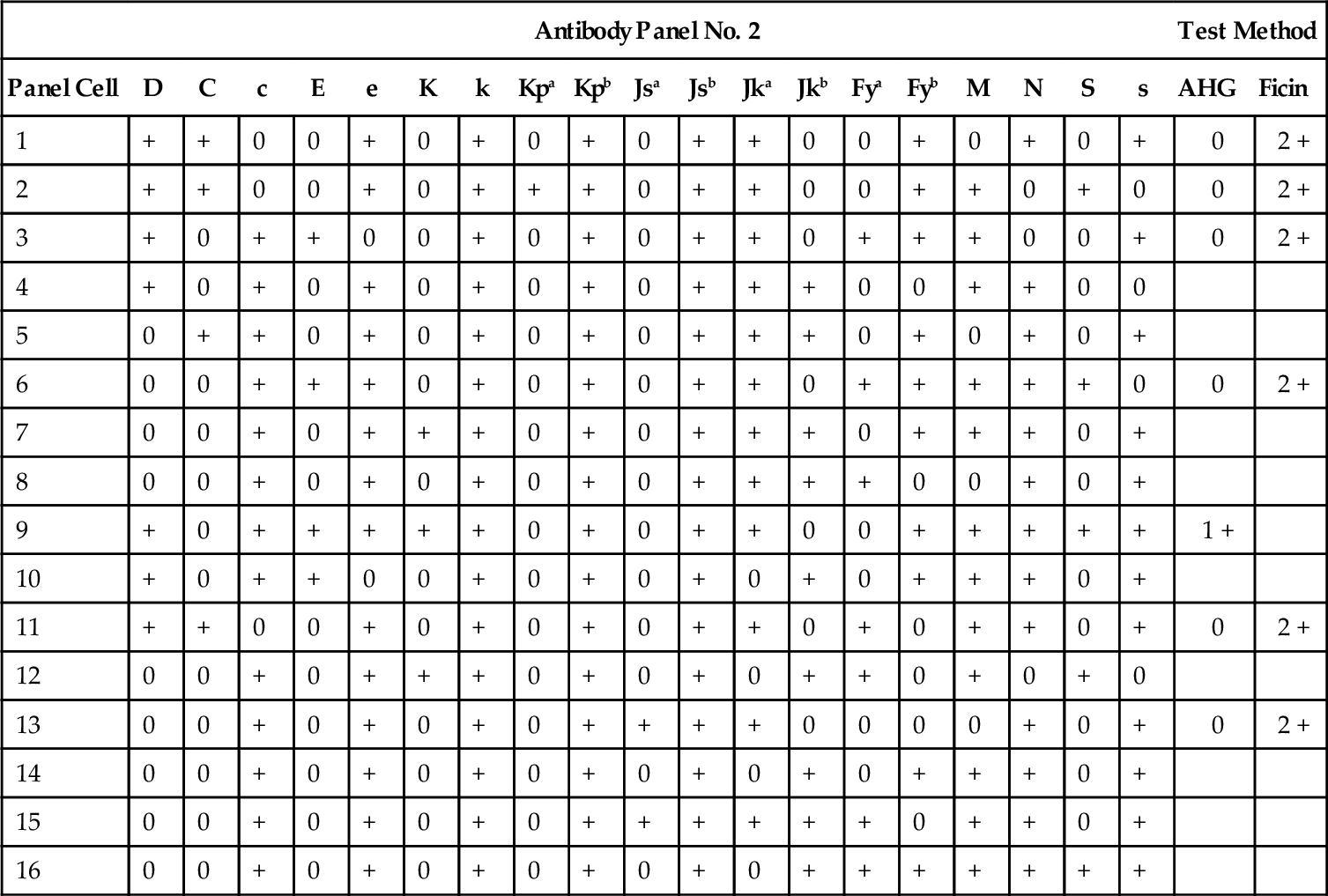
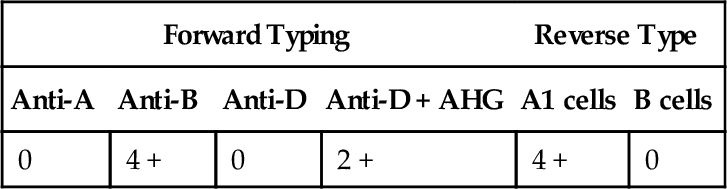
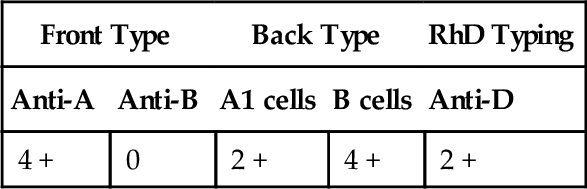
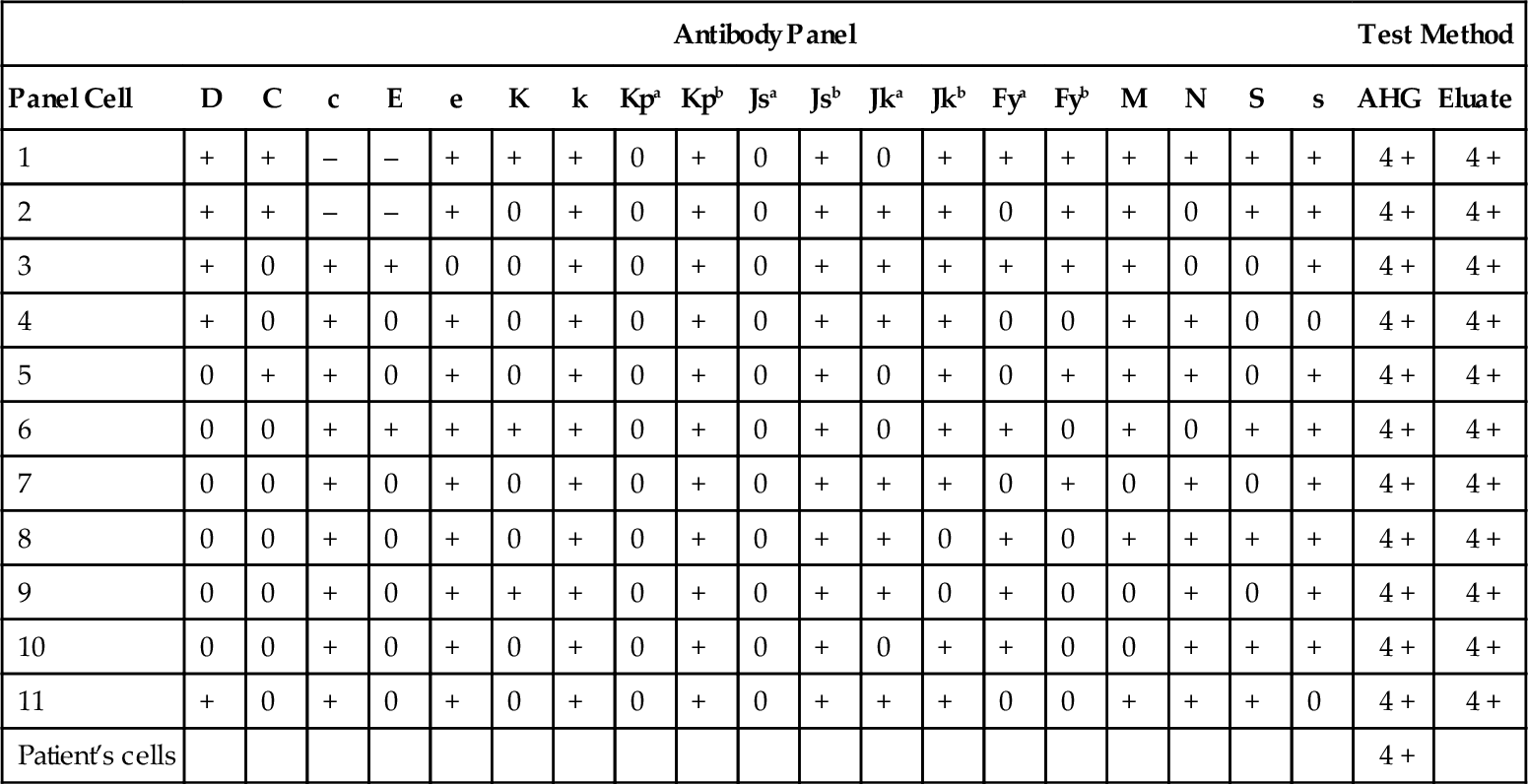
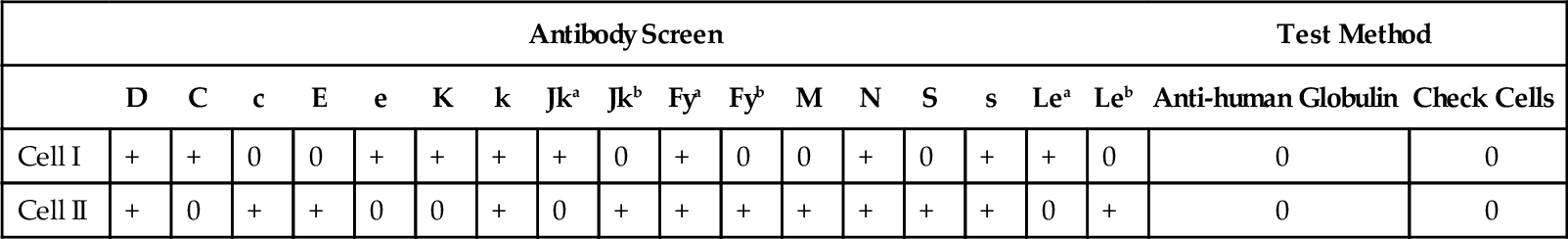
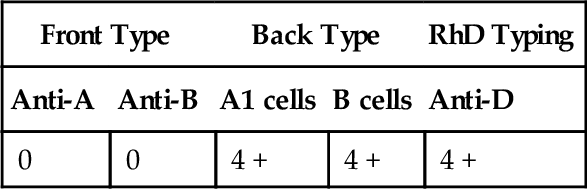
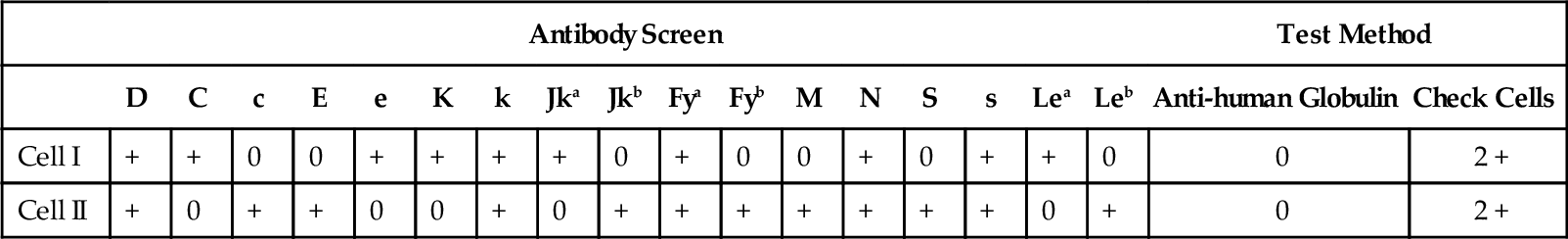
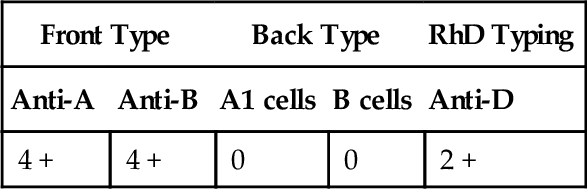
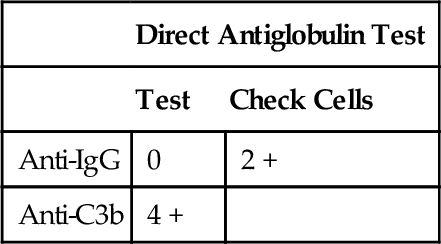
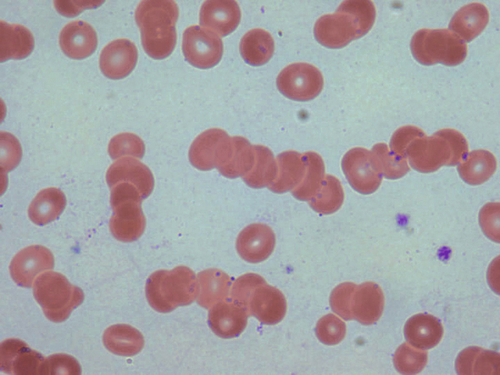
Chapter 19 Eldad A. Hod; Richard O. Francis; Suzanne A. Arinsburg; Jeffrey S. Jhang; Yvette C. Tanhehco; Joseph (Yossi) Schwartz; Steven L. Spitalnik Questions 1. Blood components are currently tested for which one of the following infectious diseases? B. Syphilis. C. Babesia. D. Dengue virus. E. Chikungunya virus. 2. Which one of the following is the approximate current estimated residual risk of hepatitis B virus (HBV) transmission from blood transfusion? B. 1:80,000 to 1:100,000. C. 1:800,000 to 1:1,000,000. D. 1:8,000,000 to 1,000,000,000. E. HBV has not been transmitted by blood transfusion in the past 10 years. 3. Which one of the following is true regarding the manufacturing of cryoprecipitate from fresh frozen plasma (FFP)? B. FFP is thawed and centrifuged at 20°C to 24°C and the precipitate is frozen at –1°C to 6°C within 1 hour of preparation. C. FFP is thawed and centrifuged at 1°C to 6°C and the precipitate is frozen at –18°C within 1 hour of preparation. D. FFP is thawed and centrifuged at 1° to 6°C and the precipitate is frozen at –18°C within 2 hours of preparation. E. FFP is thawed and centrifuged at 20°C to 24°C and the precipitate is frozen at –18°C within 2 hours of preparation. 4. Which one of the following patients should receive irradiated red blood cells (RBCs)? A. A 35-year-old male patient with human immunodeficiency virus (HIV). B. A 22-year-old man with hemophilia and a joint bleed. C. A 50-year-old woman with metastatic breast cancer. D. A 45-year-old female patient after a bone marrow transplant. E. An 8-year-old girl after a motor vehicle accident. 5. Which one of the following is the mechanism by which irradiation of blood components prevents transfusion-associated graft-versus-host disease? A. Inactivation of B-lymphocytes. B. Inactivation of T-lymphocytes. C. Inactivation of plasma cells. D. Inactivation of granulocytes. E. Inactivation of macrophages. 6. Which one of the following is true regarding blood component labeling? A. Labeling can occur at any time during the manufacturing process. B. Labeling should occur before all manufacturing steps. C. Labeling should occur before a product is placed on hold. D. Labeling should occur after all infectious disease testing is completed. E. Labeling should occur after all blood component modifications (i.e., irradiation, leukoreduction) are completed. 7. Which one of the following is the most common cause of filter failure during leukoreduction? B. Sickle cell trait. C. Thalassemia. D. Hereditary spherocytosis. E. Glucose-6-phosphate dehydrogenase deficiency. 8. Which one of the following is the U.S. Food and Drug Administration (FDA)-approved shelf-life of RBCs stored in citrate-phosphate-dextrose-adenine-one (CPDA-1) and additive solution-3 (AS-3)? B. 35 days. C. 42 days. D. 56 days. E. 112 days. 9. Which one of the following is correct regarding the rejuvenation of RBCs? B. RBCs collected in AS-1 may be rejuvenated up to 3 days after expiration and then frozen for up to 3 years. C. RBCs collected in CPD may be rejuvenated up to 42 days after collection and then frozen for up to 3 years. D. RBCs collected in AS-1 may be rejuvenated up to 42 days after collection and then frozen up to 10 years. E. RBCs collected in CPD or AS-1 may be rejuvenated at any time up to their expiration date and then frozen up to 10 years. 10. The nurse calls to inform you that a 22-year-old male patient with acute lymphoblastic leukemia has a hemoglobin of 6 g/dL (reference range, 13.3 to 16.2 g/dL). You decide to order 2 U RBCs. Which one of the following RBC unit modifications should be specified in your order to ensure that the patient receives the appropriate blood? B. Leukoreduced and irradiated. C. Leukoreduced, irradiated, and washed. D. Leukoreduced, irradiated, washed, and hemoglobin S–negative. E. This patient can receive unmodified random donor RBCs. 11. Which one of the following is correct regarding prestorage leukoreduction? A. Leukoreduction increases the risk of human leukocyte antigen (HLA) alloimmunization. B. Leukoreduction increases the incidence of febrile nonhemolytic transfusion reactions. C. Leukoreduction prevents transfusion-associated graft-versus-host disease. D. Leukoreduction reduces the risk of cytomegalovirus (CMV) transmission. E. Leukoreduction prevents transfusion-related acute lung injury. 12. Which one of the following patients is the best candidate for intraoperative blood recovery? A. A 40-year-old man undergoing hip replacement for a hip fracture after a motor vehicle accident. B. A 38-year-old woman undergoing laparotomy for lysis of adhesions secondary to metastatic colon cancer. C. A 65-year-old man undergoing colectomy for bowel rupture. D. A 75-year-old woman undergoing coronary artery bypass grafting. E. A 34-year-old pregnant woman with placenta previa. 13. Which one of the following is true regarding granulocyte transfusions? A. Granulocytes are effective only at yields greater than 5 × 106 cells/kg. B. Granulocyte yields are greatest after donor stimulation with corticosteroids. C. Granulocytes should always be leukoreduced. D. Granulocytes should never be irradiated. E. Granuloctyes should be transfused within 24 hours of collection. 14. During a whole blood donation by a 25-year-old woman, 350 mL of blood is collected. Which one of the following statements about the unit is true? A. The unit must be discarded because of an insufficient volume collected. B. The amount of anticoagulant in the collection bag must be adjusted. C. No additional labeling or processing steps other than standard procedures are required. D. The RBCs from the unit can be used for transfusion, but plasma and platelet components may not. E. The unit may be used only for research purposes. 15. An 18-year-old male arrives at a mobile blood drive reporting that he would like to donate blood but that he received the hepatitis B vaccine yesterday. Which one of the following is the deferral period for this prospective donor given his history of recent vaccination and his report that he feels well today? B. 4 weeks. C. 21 days. D. 12 months. E. None. 16. A 36-year-old man presents to a blood drive at his workplace for a whole blood donation. During the evaluation he reveals that approximately 2 weeks ago he spent approximately 24 hours in jail for public drunkenness. Which one of the following is the deferral period for this prospective donor? B. 4 months. C. 12 months. D. 3 years. E. Permanent. 17. A 58-year-old woman presents for whole blood donation. She reports that she completed a course of warfarin anticoagulation for pulmonary embolism approximately 4 days ago. Which one of the following is the correct deferral period from the time of her last warfarin dose? B. 14 days. C. 1 month. D. 6 months. E. Permanently. 18. A unit of RBCs was issued to the intensive care unit and returned unused to the blood bank. At which one of the following temperature ranges should the component have been maintained for it to be suitable for reissue? B. 1°C to 6°C. C. 20°C to 24°C. D. –18°C or less. E. 30°C to 37°C. 19. A 54-year-old woman presents to her local blood donation site for autologous donation for an upcoming hip replacement surgery. How many days before the anticipated surgery date (date of expected transfusion) must the collections be completed? B. 3 days. C. 28 days. D. 56 days. E. 112 days. A. “No history of transfusion or pregnancy in the past 90 days.” B. “Patient has a history of a negative antibody screen.” C. “No history of transfusion or pregnancy in the past 30 days.” D. “Pregnancy and transfusion history unknown.” E. “Patient is older than 40 years of age.” 21. A type and screen sample was received by your transfusion service and discarded because it was improperly labeled. Which one of the following samples is properly labeled for pretransfusion testing? B. A sample labeled at the patient’s bedside with a label containing the patient’s full name, hospital identification number, date of collection, and the phlebotomist’s initials. C. A sample labeled at the patient’s bedside with a label containing the hospital identification number, patient diagnosis, phlebotomist’s initials, and date of collection. D. A sample labeled at the patient’s bedside with a label containing the patient’s full name, hospital identification number, patient’s location, and the date of collection. E. A sample labeled at the patient’s bedside with a label containing the patient’s full name, hospital identification number, the phlebotomist’s initials, and patient’s date of birth. 22. The pretransfusion testing has been completed for a patient for whom 2 U RBCs have been ordered. In which one of the following situations is it acceptable to use a computer (i.e., electronic) crossmatch for release of these units instead of an immediate-spin (IS) or anti-human globulin (AHG) crossmatch? B. A warm autoantibody of unknown clinical significance is currently detected and underlying alloantibodies have been ruled out. C. The patient has no history of alloantibodies or autoantibodies and the antibody screen is currently negative. D. The patient has a newly positive antibody screen and the antibody has been identified as anti-RhD due to passive transfer from Rh immune globulin. E. The patient has no history of clinically significant antibodies and currently an anti-E antibody has been identified. 23. A shipment of RBC units has arrived at your transfusion service. Which one of the following confirmatory tests must be performed before these units can be made available for transfusion? A. Confirmatory Rh typing of Rh-positive units. B. Confirmatory ABO typing of only group O RBC components. C. Confirmatory testing for weak D. D. Direct antiglobulin testing. E. Confirmatory ABO typing of all RBC components. 24. Which one of the following is a benefit of International Society of Blood Transfusion (ISBT) 128 standard labeling? A. Increased ability to transfer blood components between different facilities. B. Faster processing of different blood components. C. Uniformity of labeling allowing better traceability of blood components. D. Improved use of autologous or directed donations. E. Allows for use of a computerized crossmatch for all transfusions. 25. While on your blood bank rotation, you observe that all blood products are visually inspected before release. Which one of the following types of activities is this considered to be? B. Quality control. C. Quality management. D. Quality indicator. E. Quality improvement. 26. Ten units of cryoprecipitate were thawed but not pooled for a patient who is suspected of having disseminated intravascular coagulation (DIC). Which one of the following are the correct storage temperature and expiration of these thawed units? B. 20°C to 24°C, 4 hours. C. 30°C to 37°C, 30 minutes. D. 1°C to 6°C, 24 hours. E. 1°C to 6°C, 5 days. 27. A type and screen is performed on a sample received from a 45-year-old male patient. The results of the type and screen and initial red cell antibody panel are shown in Tables 19-1 through 19-3. Pretreatment of selected panel red cells with ficin, trypsin, or dithiothreitol (DTT) does not change the reactivity pattern shown in the red cell antibody panel and testing of the patient’s red cells with Ulex europaeus lectin is negative (no agglutination). These findings are consistent with the presence of which one of the following antibodies? B. Warm autoantibody. C. Anti-H. D. Anti-Fy3. E. Anti-Kpb. 28. Which one of the following is the probability that a random donor unit will be compatible with a patient with the results of the red cell antibody panel and selected cell panel shown in Tables 19-4 and 19-5? B. 23%. C. 50%. D. 85%. E. 91%. 29. A 36-year-old woman in the second trimester of pregnancy is admitted to labor and delivery for abdominal pain. The patient has the blood typing results shown in Table 19-6. The red cell antibody screen is positive, and an antibody against the D antigen is identified in the patient’s plasma. Assuming no Rh-immunoglobulins have been administered to this patient, which one of the following is the best explanation for these results? A. Rh positive with an anti-D autoantibody. B. Partial D phenotype with an anti-D autoantibody. C. Rh positive with an anti-D alloantibody. D. Partial D phenotype with an anti-D alloantibody. E. Weak D phenotype with an anti-D alloantibody. 30. A 32-year-old woman is admitted to the intensive care unit with severe burns after a motor vehicle accident. She types as blood group B. She has DIC and has been requiring multiple units of plasma and platelets. The blood bank has an insufficient supply of group B plasma and platelets. Which one of the following will be compatible for this patient? A. Group O plasma and group B platelets. B. Group A plasma and group AB platelets. C. Group AB plasma and group A platelets. D. Group O plasma and group A platelets. E. Group A plasma and group B platelets. 31. A 46-year-old woman has seven biological children, and she reports that there is only one father for all seven children. Two of the offspring are group O, two are group A, two are group B, and one is group AB. Which one of the following choices show the possible phenotypes of the mother and father, respectively? B. AB and B. C. AB and AB. D. A and B. E. None; nonpaternity. 32. A 58-year-old man has a history of pneumonia due to Mycoplasma infection. Following treatment, the patient’s hemoglobin decreases from 15.2 g/dL (reference range, 13.3 to 16.2 g/dL) to 8.1 g/dL. The type and screen shows a cold reacting antibody. This antibody is most likely against which one of the following antigens? B. i. C. P. D. Lea. E. A. 33. Serologic testing of a patient’s red cells showed an Fy(a–b–) Duffy antigen phenotype. Which one of the following is the most likely race/ethnicity of this patient? B. Black. C. Asian/Pacific Islander. D. Native American. E. Inuit. 34. A patient’s antibody screen is positive and an antibody panel is performed. Six of 10 panel cells are reactive when tested using polyethylene glycol (PEG) and the indirect antiglobulin test (IAT). A ficin-treated panel is tested, resulting in no reactivity in all red cells tested. These findings are most consistent with antibodies to which of the following red cell antigens? B. Kell. C. Duffy. D. Lewis. E. Kidd. 35. A 26-year-old pregnant woman in the third trimester carrying a fetus with hemolytic disease of the fetus and newborn is admitted to the hospital for an intrauterine transfusion. Which one of the following antibodies would be the most likely cause of the hemolytic disease? B. i. C. I. D. S. E. Lea. 36. Kell antigens are destroyed by sulfhydryl reagents such as dithiothreitol (DTT; ZZAP) and mercaptoethanol (ME). This suggests that which one of the following elements of the Kell antigen structure is very important for its stability? B. N- and/or O-glycans. C. Zinc binding site. D. Kx antigen. E. Dombrock antigen. 37. Which one of the following Lewis phenotypes can produce anti-Lea antibodies? B. Le(a + b +). C. Le(a–b +). D. Le(a–b–). 38. Antibodies against which one of the following antigens of the MNSs blood group system are generally considered clinically insignificant and ignored for transfusion purposes? B. M. C. S. D. s. E. U. 39. Which one of the following is the highest incidence antigen in the Rh blood group system? B. C. C. c. D. E. E. e. 40. What is the modified Wiener terminology for someone with the Fisher-Race genotype Dce/dce? B. R2/r. C. R1/r′. D. Rz/r′. E. R0/r. 41. What is the risk of giving leukoreduced RhD-positive RBCs to an RhD-negative patient with a negative red cell antibody screen who is not a female of reproductive age? A. Acute intravascular hemolysis. B. Increased risk of a febrile transfusion reaction. C. Inability to receive future RBC transfusions. D. Anaphylactic reaction due to naturally occurring IgE antibodies to the RhD antigen. E. Potential alloimmunization to RhD. 42. Which one of the following antigens is part of a blood group collection rather than a blood group system? B. Cartwright. C. Colton. D. Dombrock. E. Cost. 43. A 44-year-old male patient with thalassemia major and hepatitis C is found to have a positive direct antiglobulin test (DAT) on pretransfusion testing. He receives 2 U RBCs every 3 weeks. His hemoglobin and hematocrit are as expected based on previous pretransfusion labs. No reaction is seen on the red cell antibody screen or the eluate. Which one of the following is the most likely significance of the positive DAT in this patient? A. Delayed serologic transfusion reaction. B. Delayed hemolytic transfusion reaction. C. Drug-induced hemolytic anemia. D. Nonspecific uptake of immunoglobulin. E. Laboratory analytical error. 44. Which one of the following is characteristic of naturally occurring antibodies? A. Usually are antibodies of the IgG subtype. B. React optimally at 37°C. C. Require antihuman globulin for agglutination. D. Do not readily fix complement and are associated with extravascular hemolysis. E. Do not cross the placenta. 45. A 72-year-old man is admitted for a fracture of the right radius. His hemoglobin is found to be 6.2 g/dL (reference range, 13.2 to 16.2 g/dL). A transfusion is ordered and the blood bank type and screen results are as shown in Table 19-7. A peripheral blood smear is provided in Figure 19-1. Which one of the following tests can resolve the ABO discrepancy? A. Saline replacement technique. B. Chloroquine treatment of red cells. C. Addition of rabbit erythrocyte stroma. D. Prewarm all reagents to 37°C. E. Cold autoadsorption. The blood bank received an order for a RBC transfusion for a 72-year-old patient with a hemoglobin of 6.0 g/dL, coronary artery disease, chest pain, shortness of breath, and tachycardia and a positive antibody screen with the red cell antibody panel shown in Table 19-8. Use this scenario to answer the following two questions. 46a. Which one of the following antibodies is present in the plasma of this patient and fully explains the results of the red cell antibody panel testing shown in Table 19-8? B. Anti-D alloantibody. C. Multiple alloantibodies to the following antigens: C, E, K, Fya, S. D. Alloantibody to a high-prevalence antigen. E. Alloantibody to a low-prevalence antigen. 46b. After further testing, the blood bank sends up a unit of packed RBCs and the physician taking care of the patient returns the unit because the unit was incompatible on full crossmatch. Which one of the following is the most appropriate response? B. This is the correct RBC unit, but rituximab should be administered first to prevent a hemolytic transfusion reaction. C. A full crossmatch should not have been performed; the blood bank will release an electronically crossmatch-compatible red cell unit. D. The transfusion should be delayed until crossmatch-compatible antigen-negative units are identified. E. Crossmatch-incompatible RBCs are the only option and the transfusion should not be delayed. 47. A type and screen is performed on a sample received from a currently stable 65-year-old female patient with history of transfusion. The results of the type and screen are shown in Tables 19-9 and 19-10. Which one of the following is the next step in the workup of this patient? B. Antibody panel. C. Eluate. D. Nothing; the antibody screen is negative. E. Repeat the antibody screen. 48. A 72-year-old female patient undergoing hip surgery has the type and screen results shown in Tables 19-11 and 19-12. Previous typing is consistent with these results and she has no history of a positive antibody screen. Two units of RBCs are ordered before the start of surgery in case the surgeon encounters significant bleeding. Assuming all crossmatching methods are technically possible at this hospital, which of the following would be the most appropriate and efficient crossmatch to perform before release of the units? A. No crossmatch is necessary; any two units may be released. B. Electronic crossmatch. C. Immediate spin crossmatch. D. Full AHG crossmatch in tube. E. Full AHG crossmatch in solid phase. 49. What is the significance of a positive DAT? A. The patient is experiencing a delayed hemolytic transfusion reaction. B. The patient is hemolyzing red cells. C. The patient has an autoantibody. D. The patient has antibody or complement bound to circulating red cells. E. The patient has an alloantibody to a red cell antigen. 50. A previously healthy 5-year-old boy manifests hemoglobinuria 4 days after a measles/mumps/rubella (MMR) vaccine. The results of a DAT are shown in Table 19-13. An eluate performed is nonreactive. Further testing is performed, and the patient’s serum causes hemolysis in tubes first incubated in ice and then at 37°C but not in tubes maintained at 37°C or 4°C throughout. These findings are consistent with which one of the following conditions? A. Paroxysmal cold hemoglobinuria. B. Paroxysmal nocturnal hemoglobinuria. C. Delayed hemolytic transfusion reaction. D. Warm autoimmune hemolytic anemia. E. Cold autoimmune hemolytic anemia. 51. Which one of the following factors promotes agglutination in the identification of an anti-D alloantibody? A. Temperature less than 30°C. B. Low pH (pH 2). C. Decreasing incubation time. D. Lowering the salt concentration. E. Decreasing the serum/red cell ratio. 52. A 54-year-old man is going to the operating room for a liver transplant. Per your hospital protocol, the blood bank crossmatches 20 packed red cell units in preparation for the case. The patient has a history of prior alloimmunization with an antibody to the E antigen of the Rh blood group system on current and previous testing. On crossmatching 20 E antigen–negative units, 1 U is found to be incompatible. Repeat testing of this unit confirms that it is E antigen negative and that it is indeed crossmatch incompatible. Which one of the following is the most appropriate explanation for this finding, and what should be done with this unit? B. In addition to the anti-E antibody, the patient has an antibody to a low-prevalence antigen. The incompatible unit can be reissued to another patient, and another unit should be crossmatched for this patient. C. The patient does not have an anti-E antibody and a repeat antibody screen and full red cell phenotype should be performed. Surgery should be delayed until the nature of the patient’s antibody is resolved. D. In addition to the anti-E antibody, the patient has a warm autoantibody. Because this is an autoantibody, the incompatible unit may be transfused in this patient. E. In addition to the anti-E antibody, the patient has an antibody to a high-prevalence antigen. The incompatible unit should be discarded from inventory because it contains a high-prevalence antigen. 53. A 1-day-old infant born at 39 weeks to a 29-year-old woman G2P1is noted to have yellow sclera. Laboratory tests on the cord blood reveal that the infant is type A Rh positive, direct antiglobulin test positive, and has a hemoglobin of 6 g/dL (reference range, 14.7 to 18.6 g/dL). The mother is type O Rh positive and the red cell antibody screen is negative. Hemolytic disease of the fetus and newborn (HDFN) is suspected. Which one of the following maternal antibodies is most likely cause of the anemia and jaundice in this infant? B. Anti-K. C. Anti-c. D. Anti-A. E. Anti-A,B. 54. A 45-year-old female patient presented to the emergency department 6 days ago with upper gastrointestinal bleeding that necessitated the transfusion of 2 U crossmatch-compatible blood. Her pretransfusion red cell alloantibody screen was negative. Her hemoglobin is dropping. A new red cell alloantibody screen is positive and an anti-Fya antibody is identified. The attending physician is not sure if bleeding or hemolysis is causing the drop in hemoglobin. Which one of the following sets of laboratory tests should be ordered for this patient? A. Complete blood cell count, direct and indirect bilirubin, and haptoglobin. B. Complete blood cell count, direct and indirect bilirubin, haptoglobin, and lactate dehydrogenase. C. Complete blood cell, direct and indirect bilirubin, haptoglobin, lactate dehydrogenase, direct antiglobulin test, and urinalysis. D. Complete blood cell count, direct and indirect bilirubin, haptoglobin, lactate dehydrogenase, direct antiglobulin test, urinalysis, and ionized calcium. E. Complete blood cell count, direct and indirect bilirubin, haptoglobin, lactate dehydrogenase, direct antiglobulin test, urinalysis, and potassium. 55. The Kleihauer-Betke test is used to quantitate the extent of fetal maternal hemorrhage. Which one of the following is the basis of this test? A. Fetal hemoglobin is more resistant to hypotonic saline. B. Fetal hemoglobin forms rosettes around Rh-positive cells. C. Fetal hemoglobin is less soluble than hemoglobin A. D. Fetal hemoglobin is resistant to acid treatment. E. Fetal hemoglobin is less dense than hemoglobin A. 56. The patient with blood bank testing results shown in Tables 19-14 through Tables 19-16 has an antibody to which one of the following blood group antigen systems? B. Kell. C. Kidd. D. Duffy. E. MNS.
Transfusion Medicine
Blood Collection, Immunohematology, and Transfusion Services
Blood Collection and Donor Issues
Blood Bank Regulations
Immunohematology
Transfusion Medicine: Blood Collection, Immunohematology, and Transfusion Services
Figure 19-1 Stacked RBCs on a peripheral blood smear from a patient with an ABO discrepancy.