Toxoplasma Lymphadenitis
Carlos E. Bueso-Ramos, MD, PhD
Key Facts
Etiology/Pathogenesis
Toxoplasma gondii is parasitic protozoan
Cat is definitive host for sexual stage of reproduction
Trophozoite-containing oocysts are eliminated in feces
Humans and animals are intermediate hosts
Humans ingest oocysts from contaminated soil or undercooked meat
Clinical Issues
Self-limited clinical course in most patients
Children and young adults (65%) most often affected
Unilateral lymphadenopathy, posterior cervical
Severe congenital toxoplasmosis include, chorioretinitis, cerebral calcifications, hydrocephalus, pneumonia, disseminated disease
Microscopic Pathology
Diagnostic triad
Florid reactive follicular hyperplasia
Monocytoid B-cell hyperplasia in sinuses
Epithelioid histiocytes in paracortical areas that encroach into germinal centers
No multinucleated giant cells; no necrosis
Ancillary Tests
Sabin-Feldman dye test
IgM screening antibody test positive in 1st 3 months
Positive Toxoplasma-specific antibodies are detected by enzyme immunoassays
Anti-Toxoplasma immunohistochemistry detects presence of parasites
Toxoplasma genomes can be detected by PCR
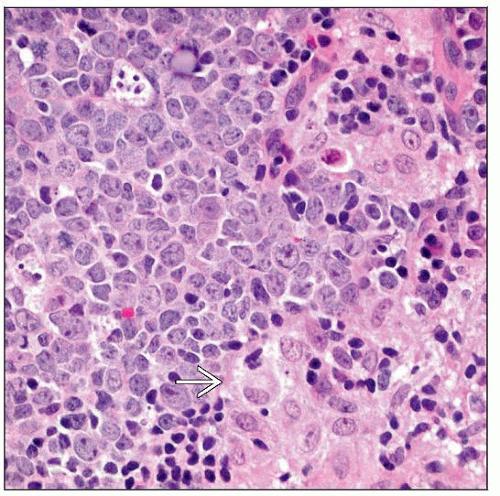
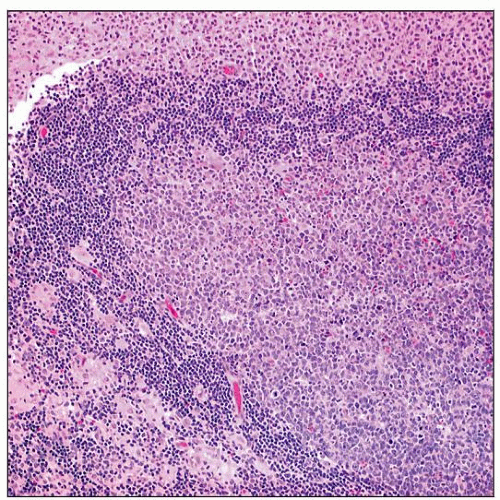 H&E stain shows Toxoplasma lymphadenitis. Note enlarged follicles with reactive germinal centers, clusters of epithelioid cells encroaching on lymphoid follicles, and monocytoid cells. |
TERMINOLOGY
Synonyms
Glandular toxoplasmosis
Piringer-Kuchinka lymphadenopathy
Definitions
Inflammation of lymph node caused by infection by Toxoplasma gondii
ETIOLOGY/PATHOGENESIS
Toxoplasma gondii Infection
T. gondii is a protozoan parasite of the phylum Apicomplexa that can invade many cell types
Cat is definitive host for sexual stage of reproduction
Trophozoites reproduce in intestinal epithelium, producing oocysts
Oocysts are eliminated in feces
Oocysts mature to infective stage in soil in 2-21 days
Humans and animals are intermediate hosts
Ingest oocysts from contaminated soil
Humans can ingest oocysts from undercooked meat
In humans and animals, oocysts are digested by digestive enzymes
Trophozoites are released into intestine
Organisms are carried by macrophages within the lymphatic system and blood vessels to internal organs
Within macrophages, trophozoites can multiply and become crescent-shaped tachyzoites
In immunocompetent patients, tachyzoites usually become segregated into cysts synthesized by host
Within cysts, organisms are slow-growing bradyzoites
Infection typically resolves
In immunodeficient patients, tachyzoites widely disseminate, causing acute infection
CLINICAL ISSUES
Epidemiology
Incidence
Toxoplasmosis is common parasitic disease worldwide
More prevalent in warm and humid climates
In USA, toxoplasmosis is most common parasitic infection
50% of USA population have serum antibodies to T. gondii: Evidence of chronic infection
T. gondii can be spread transplacentally from mother to fetus
1 in every 1,000 live births in USA
˜ 3,000 births are affected annually
Contamination of food &/or water by oocysts commonly causes human infection
Potential damage to fetus is greatest with infection in 1st trimester
Intrauterine death, microcephaly or hydrocephaly with intracranial calcifications may develop
Infections in the 2nd 1/2 of pregnancy are asymptomatic at birth
Fever, hepatosplenomegaly, and jaundice may appear
Chorioretinitis, psychomotor retardation, seizures appear months or years later
Rarely, T. gondii infection can be transmitted via transplanted organ
Active infection may result from reactivation of earlier infection
Common in patients with cancers and diabetes mellitus
Age
Children and young adults most often affected
Gender
Sexes equally affected
Site
Lymph nodes are commonly affected (95%)
Posterior cervical lymph nodes are characteristic site
Often unilateral, firm, 0.5-3.0 cm, tender or nontender
Any group of lymph nodes can be involved
Other cervical, supraclavicular, occipital, parotid, intramammary regions
Generalized lymphadenopathy or hepatosplenomegaly can occur but is unusual
Presentation
Asymptomatic infection is common in immunocompetent individuals
In immunosuppressed patients, CNS involvement is common
Mild malaise, fever, myalgia
Pneumonitis, myocarditis, retinitis, pancreatitis, polymyositis, orchitis
Laboratory Tests
Sabin-Feldman dye test
Highly sensitive and specific
T. gondii organisms do not stain with alkaline methylene blue if they have been exposed to serum anti-T. gondii antibodies
Positive result: Change from negative to positive or rapidly increasing IgG titers
Antibodies to T. gondii can be detected by enzyme immunoassays or indirect immunofluorescence
IgM or IgG antibodies against cell wall antigens
IgM antibodies present within few days after infection
Titers of 1:80 or higher indicate recent infection
IgM and IgA antibodies are 93% sensitive detecting congenital toxoplasmosis
IgG antibody titers of 1:1,000 occur 6-8 weeks after infection
Antibody to 11-kDa sporozoite protein detects infection with oocysts formed in cats
Latex agglutination test is available
Treatment
Pyrimethamine, sulfadiazine, and leucovorin
Prognosis
In immunocompetent patients, infection is self-limiting
In immunodeficient patients, great risk of acute dissemination
Encephalitis, chorioretinitis, pneumonia, and cardiac involvement
Death as result of above conditions
MICROSCOPIC PATHOLOGY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree