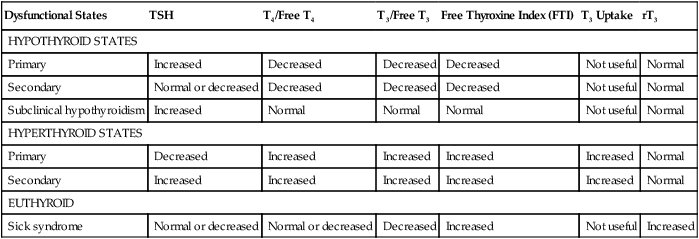
Chapter 52 Regulation of a basal metabolism is achieved through complex coordination of the hypothalamic-pituitary-thyroid feedback control system (Figure 52-1). T4 and T3 are released from the thyroid gland in response to circulating serum levels of thyroid stimulating hormone (TSH) secreted by the pituitary gland. In turn, TSH secretion is influenced by thyroid-releasing hormone (TRH) that is secreted by the hypothalamus. The feedback mechanism creates an inverse relationship between serum levels of T3-T4 and TSH-TRH. When T3 and T4 serum levels rise, TSH and TRH secretions are suppressed. Table 52-1 lists altered laboratory findings in thyroid dysfunction. TSH is the most sensitive and useful test in the diagnosis of hypothyroidism. Free T4 and T3 are also useful. The amount of circulating and unbound hormones is reduced in patients with this disorder. TABLE 52-1 Altered Laboratory Findings in Thyroid Dysfunction • American Association of Clinical Endocrinologists (AACE) Thyroid Task Force: Medical guidelines for clinical practice for the evaluation and treatment of thyrotoxicosis and hypothyroidism. Endocr Pract 8:457-469, 2002. • American College of Obstetricians and Gynecologists (ACOG): Thyroid disease in pregnancy, Washington, DC, 2002, ACOG. • Treat hypothyroidism with levothyroxine. • Dosage of all thyroid medication must be individualized. Dosage is based on laboratory findings and the patient’s clinical response. Treatment of choice for hypothyroidism is T4. It has a relatively slow onset of action, and its effects are cumulative over several weeks. T3 has a more rapid onset of action and dissipation of action. T3 may be the preferred treatment for use in rapidly correcting a hypothyroid state, in radioisotope scanning procedures, and in thyroid cancer. No evidence shows that the addition of T3 to T4 supplement has any benefit except in the very rare instances when patients cannot convert or metabolize T4 to T3. • The mean replacement dosage of levothyroxine is 1.6 mcg/kg of body weight per day, although the appropriate dosage varies among patients. The pace of treatment depends on the duration and severity of hypothyroidism and on whether other associated medical problems are present. The patient should undergo reassessment, and therapy should be titrated after an interval of 4 to 6 weeks following any change in levothyroxine brand or dose. Dosage should be titrated until a normal TSH is obtained. Adults younger than age 65 without coronary artery disease may begin with 50 to 100 mcg per day. Elderly patients and those with coronary artery disease generally should be started on a daily dose of 25 mcg. The usual maintenance dose is 75 to 150 mcg po daily. • Thyroid hormone should be administered as a single daily dose, preferably before breakfast. Levothyroxine doses are commonly measured in micrograms rather than milligrams to avoid confusion regarding the dosage. A correct dose is 75 mcg, which is the equivalent of 0.075 mg. • The AACE emphasizes that many brands of levothyroxine are available, and these are not compared against a levothyroxine standard. Bioequivalence of levothyroxine preparations is based on total T4 measurement and not on TSH levels; therefore, bioequivalence is not the same as therapeutic equivalence. It is recommended that patients should receive the same brand of levothyroxine throughout treatment. In general, desiccated thyroid hormone, combinations of thyroid hormones, or triiodothyronine should not be used as replacement therapy. See Tables 52-2 and 52-3. TABLE 52-2 Laboratory Evaluation of Thyroid Disorders TABLE 52-3 Normal Range for Thyroid Function Laboratory Tests
Thyroid Medications
Class
Generic Name
Trade Name
Thyroid supplements
levothyroxine sodium (synthetic T4)
Synthroid ![]()
Levoxyl
Levothroid
Unithroid
liothyronine (synthetic T3)
Cytomel
liotrix (T4:T3 = 4:1)
Thyrolar, Euthyroid
Thyroid suppressants
methimazole
Tapazole, generic
propylthiouracil (PTU)
Generic
Adjunctive (diagnostic tool for thyroid cancer)
thyrotropin
Thyrogen
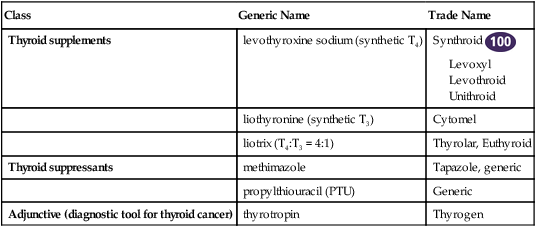
![]() Top 100 drug. Thyroid supplements will be discussed separately from thyroid suppressants.
Top 100 drug. Thyroid supplements will be discussed separately from thyroid suppressants.
Therapeutic Overview
Anatomy and Physiology
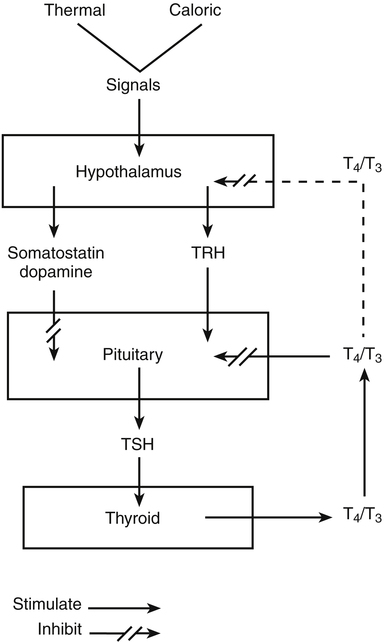
Thyroxine (T4) and triiodothyronine (T3) from the thyroid gland exert negative feedback on the pituitary by blocking the action of TRH. Negative feedback of T4 and T3 at the level of the hypothalamus is less well established. Somatostatin and dopamine each tonically inhibits TSH secretion. (From Berne RM, Levy MN: Physiology, ed 4, St Louis, 1998, Mosby; The Endocrine Society: Management of thyroid dysfunction during pregnancy and postpartum, 2007. Accessed at www.endo-society.org.)
Disease Process
Dysfunctional States
TSH
T4/Free T4
T3/Free T3
Free Thyroxine Index (FTI)
T3 Uptake
rT3
HYPOTHYROID STATES
Primary
Increased
Decreased
Decreased
Decreased
Not useful
Normal
Secondary
Normal or decreased
Decreased
Decreased
Decreased
Not useful
Normal
Subclinical hypothyroidism
Increased
Normal
Normal
Normal
Not useful
Normal
HYPERTHYROID STATES
Primary
Decreased
Increased
Increased
Increased
Increased
Normal
Secondary
Increased
Increased
Increased
Increased
Increased
Normal
EUTHYROID
Sick syndrome
Normal or decreased
Normal or decreased
Decreased
Increased
Not useful
Increased
Treatment Principles
Standardized Guidelines
Cardinal Points of Treatment
How to Monitor
Test
Hormone Evaluated
Interpretation of Test Results
TRH (thyrotropin)
Thyrotropin-releasing hormone
Assesses the function of the hypothalamic-pituitary-thyroid axis. Most useful when other tests are inconclusive
TSH
Thyroid-stimulating hormone
Assesses the function of the hypothalamic-pituitary-thyroid axis
TBG (thyroglobulin)
Thyroxine-binding globulin
As the primary protein for hormone binding, it is most useful for evaluating discrepancies in clinical findings and other serum hormone levels
T4 (T4 RIA, thyroxine)
Tetraiodothyronine, thyroxine
Concentration of bound and unbound thyroid hormone (T4) in the serum
FT4
Free thyroxine, free T4
Concentration of unbound thyroid hormone (T4) in the serum. It is most helpful for diagnosis when TBG level is abnormal.
T3 (T3 RIA)
Triiodothyronine
Concentration of bound and unbound thyroid hormone (T3) in the serum
FT3
Free triiodothyronine, free T3
Concentration of unbound, active T3 in the serum
T3-U (T3 RU)
Resin T3 uptake
Indirectly measures the concentration of thyroglobulin (TBG) by measuring the empty TBG binding sites in serum. Direct measurement of TBG may be more useful.
rT3
Reverse T3
A T3 antagonist, rT3 can be increased in euthyroid sick syndrome.
FTI (F T4-I, T7, T12)
Free T4 index
Derived by multiplying T4 and T3-U, it reflects the free (unbound) T4 in serum. This test essentially has been replaced by direct FT3 and FT4 measurements.
LATS
Long-acting thyroid stimulator
A positive test supports the diagnosis of Graves’ disease.
Antithyroid antibodies
Antithyroglobulin antibodies and/or antithyroid peroxidase antibodies
Anti-TSH receptor antibodies
High titers in individuals with Hashimoto’s thyroiditis and Graves’ disease
High titers in individuals with Graves’ disease
Name of Test
Normal Range for Values
TRH (thyrotropin-releasing hormone)
Males: 14-24 mcg/ml
Females: 16-26 mcg/ml
TSH (thyroid-stimulating hormone)
Newborn: <20 mcg/ml
Adult: 0.30-5.5 mcg/ml
TBG (thyroglobulin)
16-34 micro units/ml
T4 (thyroxine)
Newborn: 6.4-23.2 mcg/ml
Child (1-10 yr): 6.4-15 mcg/ml
Adult: 5-12 mcg/ml
FT4 (free thyroxine)
0.9-1.7 ng/dl
T3 (triiodothyronine)
Newborn: 32-250 ng/ml
Child (1-10 yr): 94-269 ng/ml
Adult: 95-190 ng/ml
FT3 (free triiodothyronine)
0.2-0.52 ng/dl
T3-U (resin T3 uptake)
25%-35%
FTI (free thyroxine index)
1.3-4.2
Antithyroid antibodies: Anti-TBG antimicrosomal
Negative or titer <1:100
LATS (long-acting thyroid stimulator)
Negative
Patient Variables
Geriatrics
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thyroid Medications
Only gold members can continue reading. Log In or Register to continue
