 Thoracic Aorta
Thoracic AortaSurgical Anatomy of the Great Vessels of the Chest
Overview
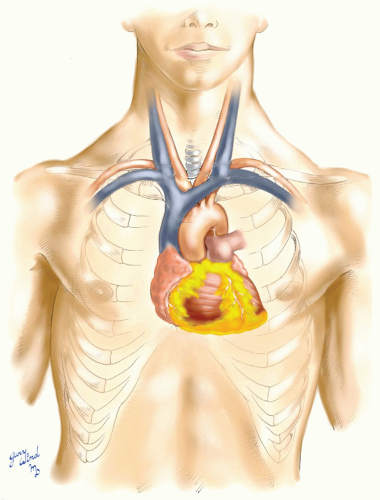
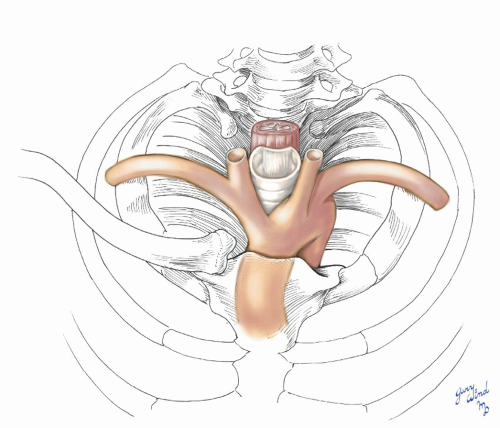
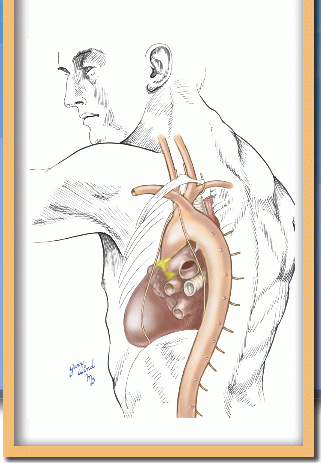
To understand the anatomic disposition of the great vessels of the chest, one must view them in the context of the mediastinum and the superior thoracic aperture. The mediastinum is a short handspan in height from its base at the subcardiac portion of the diaphragm to the superior thoracic aperture (Fig. 3-1). The origin of the great vessels from the base of the heart lies at the midpoint of this length. The aortic arch, superior vena cava, and their branches lie closely packed with the trachea and esophagus in the superior mediastinum. At the superior thoracic aperture, the major branches blossom out to the arms and head. Understanding the relationships at these two key sites leads to an appreciation of the surgical approaches to these vessels.
The Mediastinum
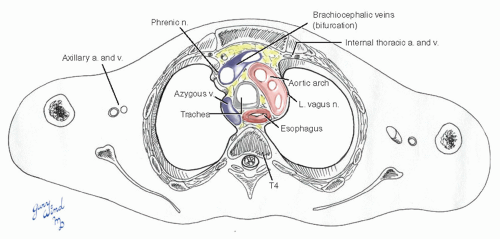
At the level of the superior mediastinum, half the A-P diameter of the chest is occupied by the vertebrae (Fig. 3-2). In the small anterior component of this cross-section lie the great vessels, tracheobronchial tree, and esophagus. The lateral surfaces of this space are covered by closely applied parietal pleura, giving the underlying structures the appearance of having been shrink-wrapped.
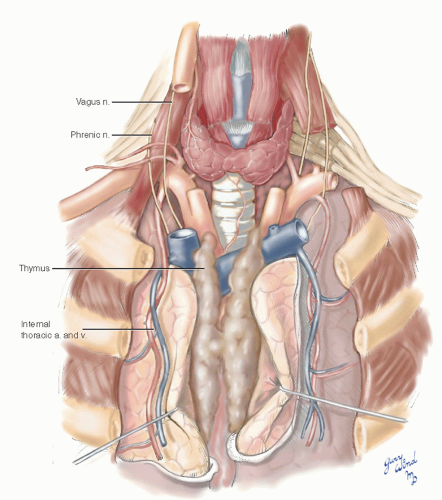
The parietal pleura surrounds the pulmonary hilum, forming a short, broad-based bundle, and is reflected onto the medial lung surfaces (Fig. 3-3). The leaves of pleura surrounding the lung hila extend caudally between the lung and mediastinum to form the inferior pulmonary ligaments. The aorta frames the left lung root, and the ascending, transverse, and descending segments of the aorta are approached by reflecting the lung away in the appropriate direction. Between the pleura and pericardium, the phrenic nerves descend to the diaphragm accompanied by thin pericardiophrenic vessels (Fig. 3-4). The latter arise from the brachiocephalic vessels and/or from the internal thoracic (internal mammary) vessels.
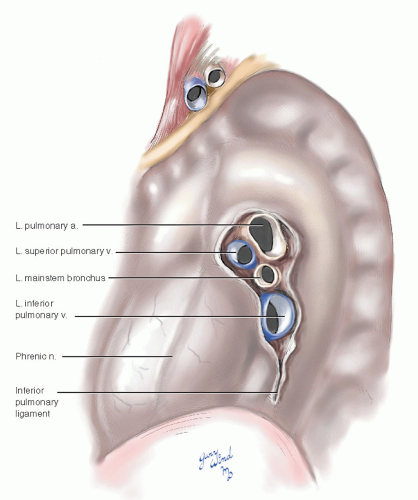 Fig. 3-3 The closely applied parietal pleura encloses the mediastinum laterally and surrounds the hilar stalks of the lungs. |
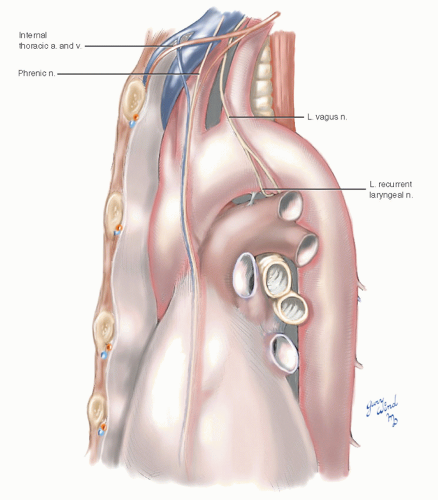 Fig. 3-4 The phrenic and vagus nerves lie beneath the parietal mediastinal pleura. The distal part of the phrenic nerve lies between pleura and pericardium. |
The second set of major nerves traversing the mediastinum is the right and left vagus (Fig. 3-5). These are worth considering separately. The right vagus passes in front of the subclavian artery just lateral to its origin from the brachiocephalic artery. The right recurrent laryngeal nerve turns posteriorly beneath the subclavian artery and ascends in the tracheoesophageal groove, while the vagus descends behind the right main stem bronchus to reach the esophagus. The left vagus nerve passes between the left subclavian artery and left brachiocephalic vein to reach the lateral side of the aortic arch. Here the left recurrent laryngeal nerve diverges to pass beneath the aortic arch behind the ligamentum arteriosum. The vagus descends to reach the left side of the esophagus. At their junction with the esophagus, the vagi shift position, with the left moving anteriorly and the right moving posteriorly. Both trunks break up into multiple branches, which freely anastomose around the esophagus. This plexus coalesces into two major and several minor nerves at the distal esophagus. The major trunks lie anterior and posterior to the esophagus.
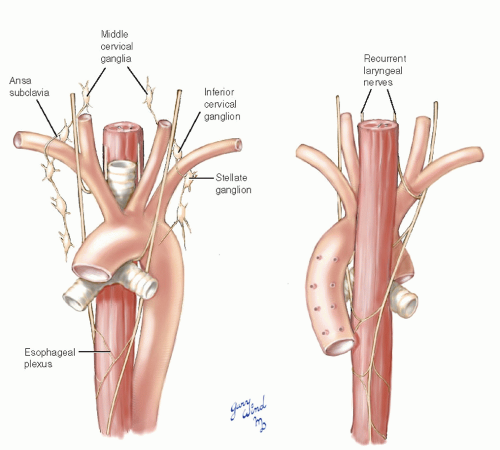 Fig. 3-5 The vagus nerves pass posterior to the lung roots to reach the midesophagus where they form an interconnecting plexus. |
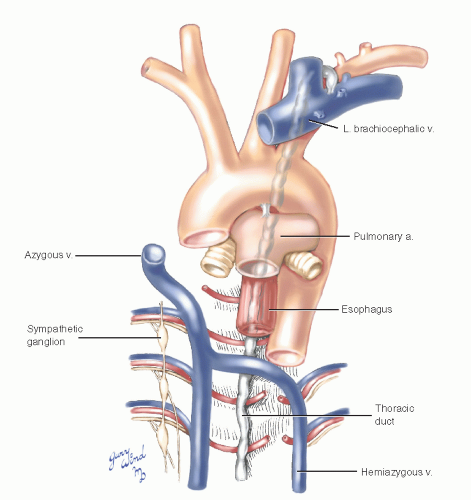
Two additional anatomic features should be noted for completeness. At the posterior limit of the mediastinum, the thoracic duct ascends between the esophagus and the vertebral bodies (Fig. 3-6). An extensive plexus of autonomic nerves surrounds the vascular and bronchial structures of the superior mediastinum.
The Aorta
The ascending aorta lies beneath the sternomanubrial joint and is accessible directly through the sternum (Fig. 3-7). The only intervening tissue is the remnant of the thymus gland. Flanking the sternum on either side are the internal thoracic vessels, which are tethered at their origins proximally. The medial pleural reflections closely approach the midline over the ascending aorta. The apex of the aortic arch lies
in a diagonal direction relative to the sagittal plane of the chest (Fig. 3-8). As a result, the origins of the brachiocephalic and left common carotid arteries arise relatively anteriorly, while the left subclavian is more posteriorly placed. The confined space at the tapering lung apices restricts anterior access to the proximal left subclavian artery and mandates a left transthoracic approach for adequate exposure.
in a diagonal direction relative to the sagittal plane of the chest (Fig. 3-8). As a result, the origins of the brachiocephalic and left common carotid arteries arise relatively anteriorly, while the left subclavian is more posteriorly placed. The confined space at the tapering lung apices restricts anterior access to the proximal left subclavian artery and mandates a left transthoracic approach for adequate exposure.
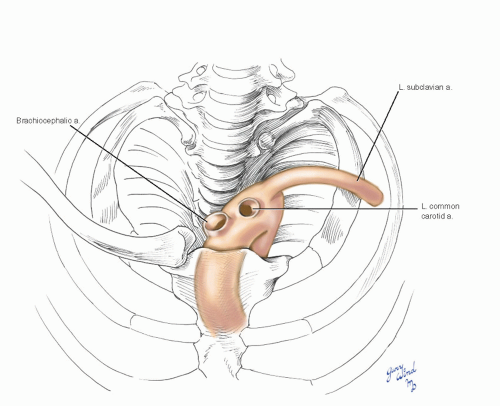 Fig. 3-8 The oblique axis of the aortic arch relative to the transverse plane of the chest places the origin of the left subclavian artery posteriorly. |
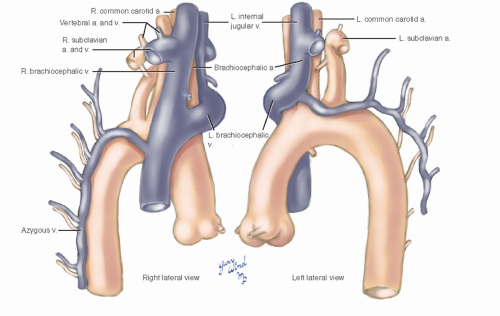
As these vessels ascend and diverge, they surround the trachea and esophagus on three sides (Fig. 3-9). The arteries in turn are covered by an outer layer of major venous trunks. The superior vena cava lies lateral and parallel to the ascending aorta (Fig. 3-10). At the bifurcation of brachiocephalic veins, the right branch lies in the same coronal plane as the vena cava, inclined slightly to the right. The left brachiocephalic vein, on the other hand, arches anteriorly over the origins of the left common carotid and brachiocephalic arteries in its descent from left to right (Fig. 3-11). On the right side, the azygous vein drains into the superior vena cava just above the upper limit of the pericardium. On the left, the accessory hemiazygous vein drains into the brachiocephalic vein.
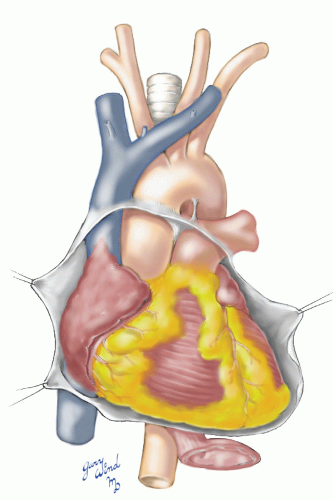 Fig. 3-10 The superior vena cava parallels the ascending aorta, and both are covered with pericardium to their midpoints. |
The Superior Thoracic Aperture
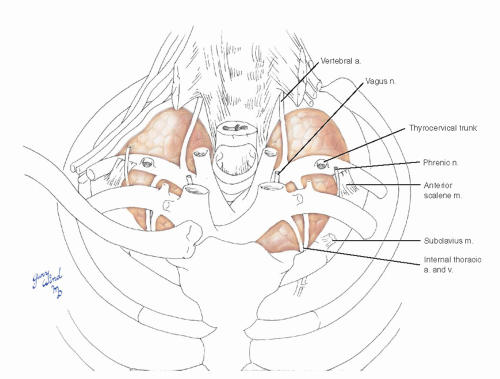
The central viscera at the thoracic aperture are confined anteriorly by the manubrium of the sternum and posteriorly by the vertebral column. A strong dome of fascia (Sibson’s), continuous with the endothoracic fascia, covers the apex of each lung. The anterior halves of these domes support the arching subclavian vessels (Fig. 3-12). The cords of the brachial plexus descend over the posterior margin of the domes to converge with the subclavian arteries over the first ribs. Proximal branches of the subclavian vessels arise and ramify above these domes.
The clavicle articulates with the manubrium medially and acts as a protective barrier over the subclavian vessels. The costoclavicular ligament between the clavicle and the first rib forms the anterior
boundary of the aperture where the axillary vein passes over the first rib to become the subclavian. This structure marks the highest limit of an axillary dissection and is an important landmark for subclavian puncture.
boundary of the aperture where the axillary vein passes over the first rib to become the subclavian. This structure marks the highest limit of an axillary dissection and is an important landmark for subclavian puncture.
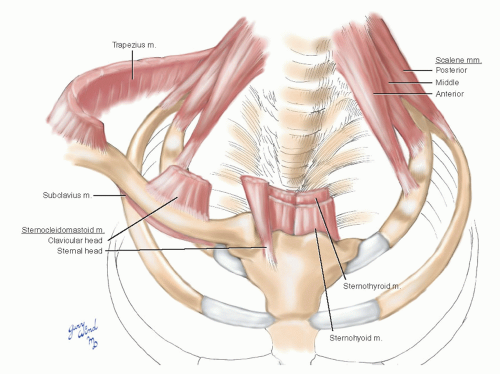
An inverted cone of muscles attaches around the rim of the superior thoracic aperture (Fig. 3-13). The anterior and middle scalene muscles attach to the first rib, and the posterior scalene to the second rib, the strap muscles attach to the manubrium, and the sternocleidomastoid muscles attach to the medial part of the clavicle and to the manubrium. With all this protective architecture, it takes considerable force to fracture the first rib. When such a fracture occurs, associated major vessel injury must be suspected.
Beyond the arch, the proximal descending aorta lies to the left of the thoracic vertebral bodies (Fig. 3-14). It becomes progressively more midline as it approaches the aortic hiatus at the level of the twelfth thoracic vertebra. These relationships determine the optimal surgical approaches to the great vessels of the chest for control of hemorrhage in trauma and for elective surgical procedures.
Exposure of the Aortic Arch Branches
The importance of obtaining vascular control proximal and distal to an arterial injury is nowhere more evident than in the mediastinum. Rapid exsanguination, airway compromise, and cardiac tamponade threaten patients who have sustained injuries to the major branches of the aortic arch. Although endovascular management may have a place in the treatment of highly selected patients with contained hematomas, immediate open exploration is indicated in unstable patients.1 Standard open surgical approaches remain the standard of care to treat blunt and penetrating injuries of the aortic arch branches because the long-term stent graft durability is unknown in the trauma population.1,2
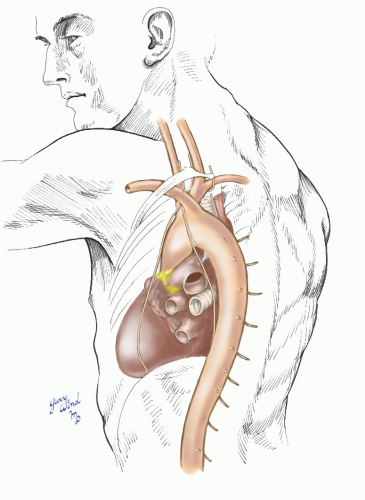 Fig. 3-14 The descending aorta initially lies anterolateral to the vertebral column and assumes a midline position at the aortic hiatus of the diaphragm in front of the twelfth thoracic vertebra. |
The aortic arch branches include the left subclavian, left common carotid, and brachiocephalic arteries. Adequate exposure of these arteries without a thoracic incision is virtually impossible. Injuries to vascular structures at the base of the neck (zone I, see Chapter 1) are also difficult to manage without exposure of more proximal arteries in the chest. Early thoracotomy or sternotomy and rapid proximal arterial control in the chest can significantly reduce the mortality associated with injuries to the vessels of the mediastinum and base of the neck.3,4,5 Although repair of aortic arch injuries almost always requires hypothermic cardiac arrest and or/cardiopulmonary bypass, arch vessels can usually be repaired without extracorporeal circulatory support or arterial shunts.6
Exposure of the brachiocephalic artery, proximal right subclavian and carotid arteries, and the proximal left common carotid artery requires median sternotomy.4,5 Because of the relatively posterior location of the left subclavian artery in the mediastinum (see Fig. 3-9), a left thoracotomy is required for adequate proximal exposure of the proximal left subclavian artery, usually in combination with a separate supraclavicular incision or “trap door” extension.4,7
Patients with chronic occlusions of aortic arch branches rarely require thoracic incisions. Extrathoracic arterial revascularizations such as the carotidsubclavian bypass have been shown to be simple and durable approaches with low morbidity.8 Likewise, preoperative revascularization of the left subclavian artery before thoracic endovascular aortic repair can be performed through an extrathoracic incision.9 One notable exception is the repair of symptomatic brachiocephalic artery lesions, which are best treated with direct arterial repair or bypass through a median sternotomy.10,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree