It is important to correctly characterize the movement disorder because different movement disorders can be managed by different interventions.
Spasticity
Spasticity is the most common movement disorder, affecting between 60% and 80% of children with cerebral palsy (Fig. 15.1). Spasticity is defined as hypertonia in which one or both of the following signs are present:
- resistance to externally imposed movement increases with increasing speed of stretch and varies with the direction of joint movement
- resistance to externally imposed movement rises rapidly above a threshold speed or joint angle.
When focal, spasticity is often managed by injections of botulinum neurotoxin (BoNT). When severe or generalized, spasticity may be managed by selective dorsal rhizotomy or intrathecal baclofen.
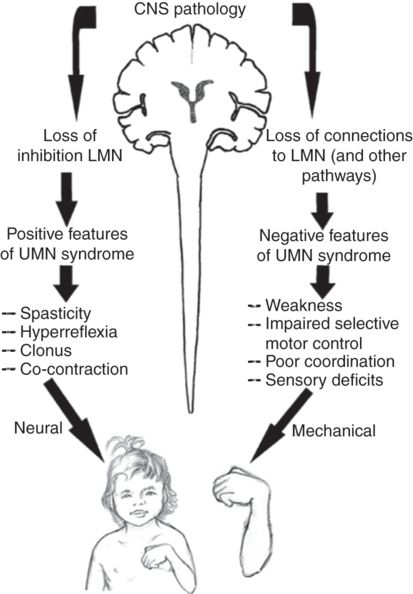
Fig. 15.1 Scheme of spasticity. LMN, lower motor neuron; UMN, upper motor neuron.
Dystonia
Dystonia is characterized by involuntary sustained or intermittent muscle contractions that cause twisting and repetitive movements, abnormal postures, or both. Focal dystonia may also be treated with BoNT. In generalized dystonia, intrathecal baclofen may have a role. However, selective dorsal rhizotomy does not appear to offer improvement.
Athetosis
Athetosis, or intermittent writhing movement, is also very common. It is sometimes managed by oral medications and when severe by intrathecal baclofen pump, but never by selective dorsal rhizotomy.
Ataxia
Ataxia is less common in cerebral palsy and is difficult to treat successfully. In addition to the overactivity (positive) features of cerebral palsy such as spasticity and dystonia, there are also negative features – principally weakness and loss of selective motor control. In the long term, weakness and difficulty in controlling muscles have a much greater impact on gross motor function than the various forms of muscle overactivity. Nevertheless, spasticity has been implicated in the development of fixed deformities, which can further impair function and quality of life in the child or adolescent affected by cerebral palsy.
Topographical symptom distribution and anatomical approach to management
Understanding the topographical distribution of symptoms and recognizing the common clinical patterns of muscle overactivity form the basis for development of management strategies. These patterns are reviewed as the basis for intervention with BoNT and other therapies before turning to injection techniques.
As indicated in Box 15.1, involvement may be unilateral (monoplegic or hemiplegic) or bilateral (diplegic, paraplegic or quadriplegic). Spastic diplegia usually refers to individuals with minimal involvement of the upper limbs but bilateral lower limb involvement. Spastic quadriplegia refers to individuals with involvement of all four limbs, with the upper limbs sometimes more affected than the lower limbs. However, the differentiation between spastic diplegia and spastic quadriplegia is not clear cut and it is more clinically useful to classify bilateral cerebral palsy according to gross motor function, as noted above.
Unilateral cerebral palsy: spastic hemiplegia
In hemiplegia, motor pathway involvement on one side of the brain leads to contralateral motor symptoms (Fig. 15.2). The most common movement disorder is spastic but mixed spastic and dystonic types are also very common. Sometimes the upper limb has mainly a dystonic movement disorder and the lower limb a mainly spastic movement disorder.
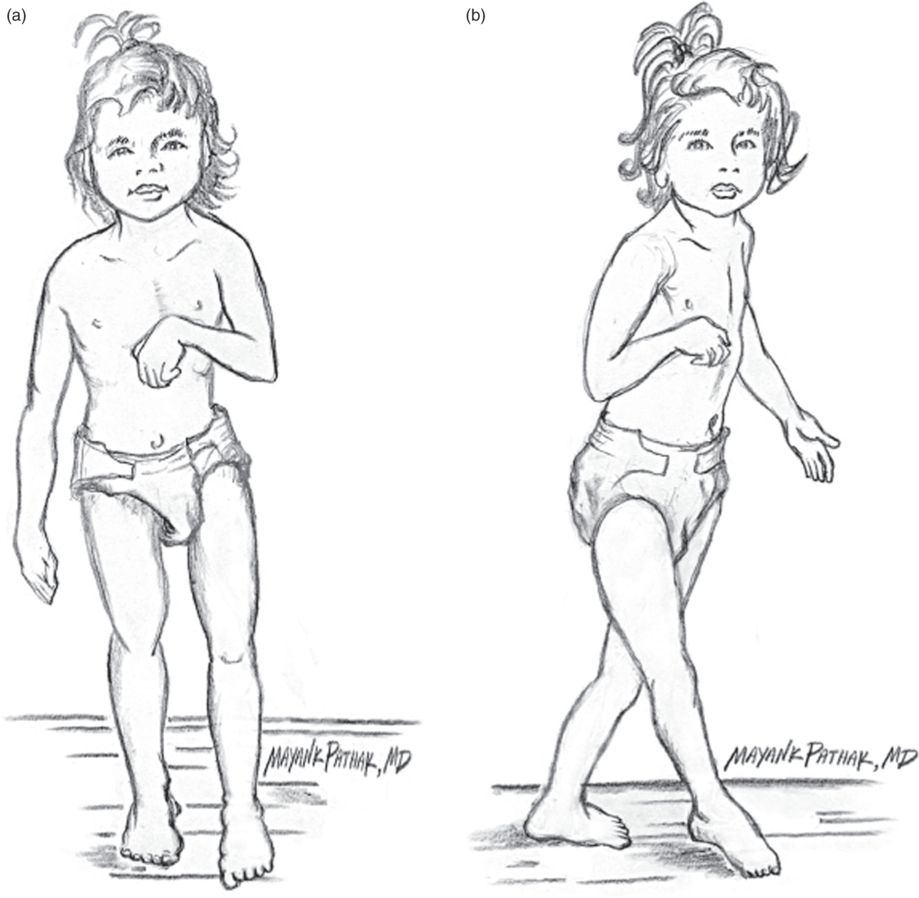
Fig. 15.2 Spastic hemiplegia, frontal (a) and lateral (b) views. Muscles that are involved in spastic hemiplegia are biceps, brachialis, adductor pollicis, flexor carpi ulnaris, flexor carpi radialis, pronator teres, gastrocnemius, soleus, tibialis posterior.
Upper limb
Typical upper limb posturing includes adduction and internal rotation at the shoulder, pronation and flexion at the elbow/forearm, and flexion and ulnar deviation at the wrist with flexed digits and “thumb in palm.” The muscles typically involved in each pattern are indicated in Table 15.1, along with guidelines for injection of BoNT-A as onabotulinumtoxinA (Botox, Allergan, Irvine, CA, USA).

Without intervention, spastic posturing in the hemiplegic upper limb can progress to painful fixed contracture and deformities, which further impair function, and cosmesis. It is tempting to think that the spasticity or dystonia is the main functional limitation in the hemiplegic upper limb, and that relaxing the overactive muscles will necessarily restore function. On the contrary, the main barriers to function are impaired selective motor control and sensation. Muscle relaxation may set the stage for functional gains but may not be adequate by itself. Therefore, focal treatment with BoNT alone is rarely indicated and it should usually be combined with a program of splinting and occupational therapy or upper limb training.
Lower limb
The involved lower limb is usually slightly shorter than that on the uninvolved side, with muscle atrophy particularly affecting the calf muscle. Typically, involvement is more pronounced distally than proximally (Box 15.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


