Chapter 13
The urinary system
The effects of ageing on the urinary system
Diseases of the renal pelvis, ureters, bladder and urethra
![]() Animations
Animations
13.1 The urinary system 338
13.2 Gross structure of the kidney 339
13.3 Structure of the nephron 339
13.4 Filtration 341
13.5 Renal filtration 341
13.6 Reabsorption 342
13.7 Aldosterone regulation mechanism 343
13.9 Urinary mechanism of pH control 345
13.13 Renal stone 354
13.14 Hydroureter 354
13.15 Hydronephrosis 355
The urinary system is the main excretory system and consists of the following structures:
• 2 kidneys, which secrete urine
• 2 ureters that convey the urine from the kidneys to the urinary bladder
• the urinary bladder, which collects and stores urine
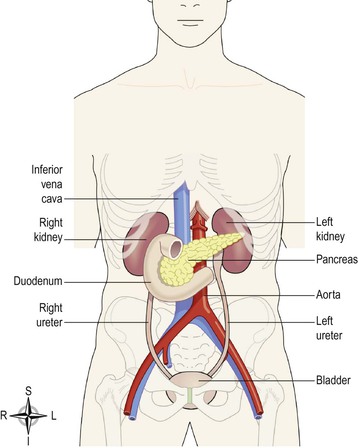
Figure 13.1 shows an overview of the urinary system. The urinary system plays a vital part in maintaining homeostasis of water and electrolytes within the body. The kidneys produce urine that contains metabolic waste products, including the nitrogenous compounds urea and uric acid, excess ions and some drugs. The main functions of the kidneys are:
Urine is stored in the bladder and excreted by the process of micturition.
The first sections of this chapter explore the structures and functions of the organs of the urinary system and the impact of ageing on kidney function. In the final section the consequences of abnormal functioning of the various parts of the urinary system on body function are considered.
Kidneys
The kidneys (Fig. 13.2) lie on the posterior abdominal wall, one on each side of the vertebral column, behind the peritoneum and below the diaphragm. They extend from the level of the 12th thoracic vertebra to the 3rd lumbar vertebra, receiving some protection from the lower rib cage. The right kidney is usually slightly lower than the left, probably because of the considerable space occupied by the liver.
Kidneys are bean-shaped organs, about 11 cm long, 6 cm wide, 3 cm thick and weigh 150 g. They are embedded in, and held in position by, a mass of fat. A sheath of fibrous connective tissue, the renal fascia, encloses the kidney and the renal fat.
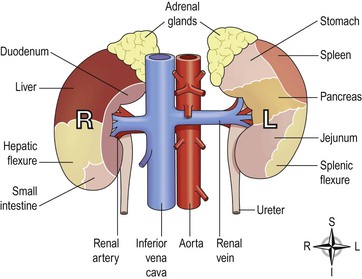
Organs associated with the kidneys (Figs 13.1 and 13.2)
As the kidneys lie on either side of the vertebral column, each is associated with different structures.
Gross structure of the kidney  13.2
13.2
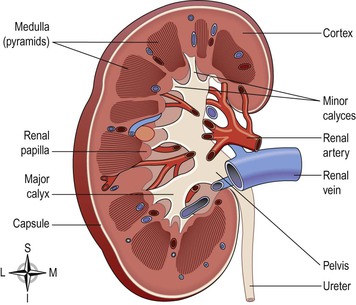
There are three areas of tissue that can be distinguished when a longitudinal section of the kidney is viewed with the naked eye (Fig. 13.3):
• an outer fibrous capsule, surrounding the kidney
• the medulla, the innermost layer, consisting of pale conical-shaped striations, the renal pyramids.
The hilum is the concave medial border of the kidney where the renal blood and lymph vessels, the ureter and nerves enter.
Urine formed within the kidney passes through a renal papilla at the apex of a pyramid into a minor calyx (Fig. 13.3). Several minor calyces merge into a major calyx and two or three major calyces combine forming the renal pelvis, a funnel shaped structure that narrows when it leaves the kidney as the ureter. The walls of the calyces and renal pelvis are lined with transitional epithelium and contain smooth muscle. Peristalsis, intrinsic contraction of smooth muscle, propels urine through the calyces, renal pelvis and ureters to the bladder.
Microscopic structure of the kidney  13.3
13.3
The kidney contains about 1–2 million functional units, the nephrons, and a much smaller number of collecting ducts. The collecting ducts transport urine through the pyramids to the calyces, giving the pyramids their striped appearance (Fig. 13.3). The collecting ducts are supported by connective tissue, containing blood vessels, nerves and lymph vessels.
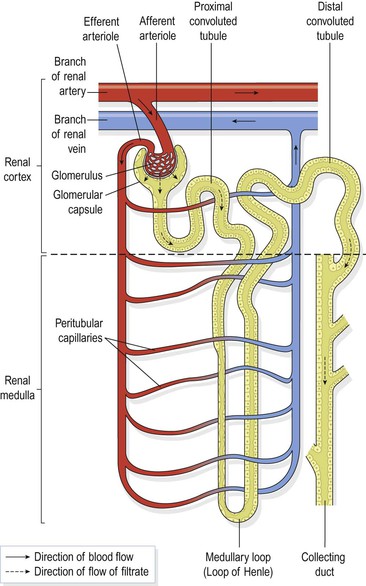
The nephron (Fig. 13.4)
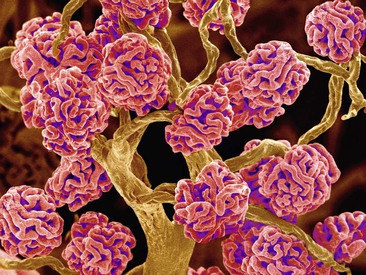
The nephron is essentially a tubule closed at one end that joins a collecting duct at the other end. The closed or blind end is indented to form the cup-shaped glomerular capsule (Bowman’s capsule), which almost completely encloses a network of tiny arterial capillaries, the glomerulus. These resemble a coiled tuft and are shown in Figure 13.5. Continuing from the glomerular capsule, the remainder of the nephron is about 3 cm long and described in three parts:
• the proximal convoluted tubule
• the medullary loop (loop of Henle)
• the distal convoluted tubule, leading into a collecting duct.
The collecting ducts unite, forming larger ducts that empty into the minor calyces.
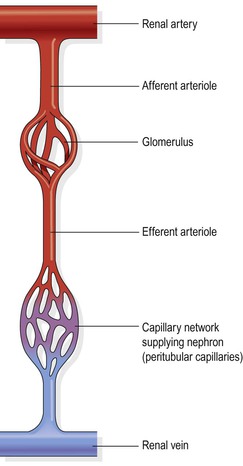
The kidneys receive about 20% of the cardiac output. After entering the kidney at the hilum, the renal artery divides into smaller arteries and arterioles. In the cortex an arteriole, the afferent arteriole, enters each glomerular capsule and then subdivides into a cluster of tiny arterial capillaries, forming the glomerulus. Between these capillary loops are connective tissue phagocytic mesangial cells, which are part of the monocyte–macrophage defence system (p. 70). The blood vessel leading away from the glomerulus is the efferent arteriole. The afferent arteriole has a larger diameter than the efferent arteriole, which increases pressure inside the glomerulus and drives filtration across the glomerular capillary walls (Fig. 13.6). The efferent arteriole divides into a second peritubular (meaning ‘around tubules’) capillary network, which wraps around the remainder of the tubule, allowing exchange between the fluid in the tubule and the bloodstream (Figs 13.4 and 13.7). This maintains the local supply of oxygen and nutrients and removes waste products. Venous blood drained from this capillary bed eventually leaves the kidney in the renal vein, which empties into the inferior vena cava.
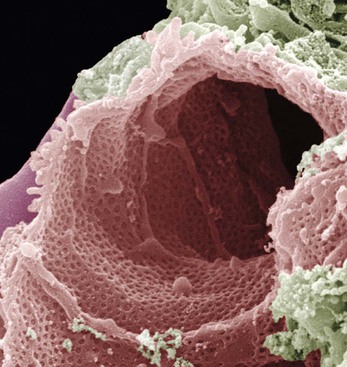
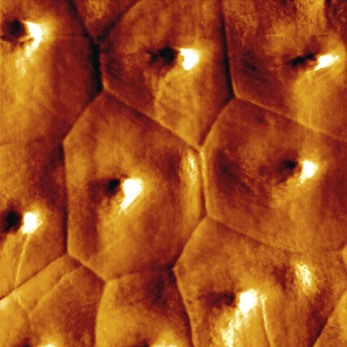
The walls of the glomerulus and the glomerular capsule consist of a single layer of flattened epithelial cells. The glomerular walls are more permeable than those of other capillaries. The remainder of the nephron and the collecting duct are formed by a single layer of simple squamous epithelium (Fig. 13.8).
Renal blood vessels are supplied by both sympathetic and parasympathetic nerves. The presence of both divisions of the autonomic nervous system controls renal blood vessel diameter and renal blood flow independently of autoregulation (p. 342).
Functions of the kidney
Formation of urine
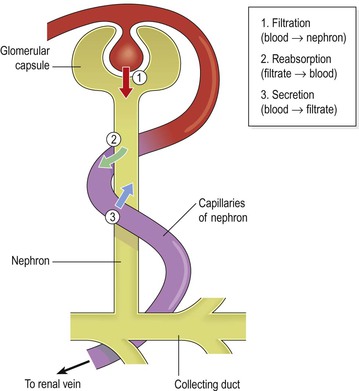
The kidneys form urine, which passes to the bladder for storage prior to excretion. The composition of urine reflects exchange of substances between the nephron and the blood in the renal capillaries. Waste products of protein metabolism are excreted, water and electrolyte levels are controlled and pH (acid–base balance) is maintained by excretion of hydrogen ions. There are three processes involved in the formation of urine:
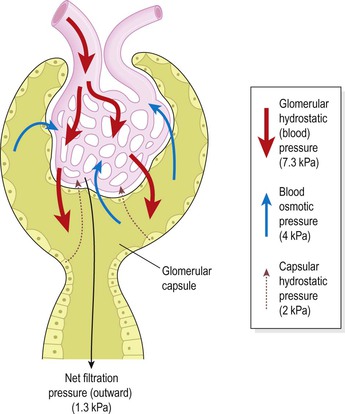
Filtration (Fig. 13.10)  13.4, 13.5
13.4, 13.5
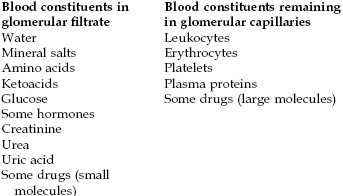
This takes place through the semipermeable walls of the glomerulus (Fig. 13.9) and glomerular capsule. Water and other small molecules readily pass through, although some are reabsorbed later. Blood cells, plasma proteins and other large molecules are too large to filter through and therefore remain in the capillaries (Box 13.1). The filtrate in the glomerulus is very similar in composition to plasma with the important exceptions of plasma proteins and blood cells.
Filtration takes place because there is a difference between the blood pressure in the glomerulus and the pressure of the filtrate in the glomerular capsule. Because the efferent arteriole is narrower than the afferent arteriole, a capillary hydrostatic pressure of about 7.3 kPa (55 mmHg) builds up in the glomerulus. This pressure is opposed by the osmotic pressure of the blood, provided mainly by plasma proteins, about 4 kPa (30 mmHg), and by filtrate hydrostatic pressure of about 2 kPa (15 mmHg) in the glomerular capsule. The net filtration pressure is, therefore:
The volume of filtrate formed by both kidneys each minute is called the glomerular filtration rate (GFR). In a healthy adult the GFR is about 125 mL/min, i.e. 180 litres of filtrate are formed each day by the two kidneys. Nearly all of the filtrate is later reabsorbed from the kidney tubules with less than 1%, i.e. 1–1.5 litres, excreted as urine. The differences in volume and concentration are due to selective reabsorption of some filtrate constituents and tubular secretion of others (see below).
Autoregulation.
Renal blood flow, and therefore glomerular filtration, is protected by a mechanism called autoregulation, whereby renal blood flow is maintained at a constant pressure across a wide range of systolic blood pressures (from around 80–200 mmHg). Autoregulation operates independently of nervous control, i.e. if the nerve supply to the renal blood vessels is interrupted, autoregulation continues to operate. It is therefore a property inherent in renal blood vessels; it may be stimulated by changes in blood pressure in the renal arteries or by fluctuating levels of certain metabolites, e.g. prostaglandins.
In severe shock, when the systolic blood pressure falls below 80 mmHg, autoregulation fails and renal blood flow and the hydrostatic pressure decrease, impairing filtration within the glomeruli.
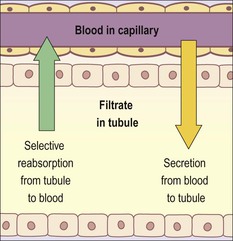
Selective reabsorption (Fig. 13.11)  13.6
13.6
Most reabsorption from the filtrate back into the blood takes place in the proximal convoluted tubule, whose walls are lined with microvilli to increase surface area for absorption. Many substances are reabsorbed here, including some water, electrolytes and organic nutrients such as glucose. Some reabsorption is passive, but some substances, e.g. glucose, are actively transported. Only 60–70% of filtrate reaches the medullary loop. Much of this, especially water, sodium and chloride, is reabsorbed in the loop, so that only 15–20% of the original filtrate reaches the distal convoluted tubule, and the composition of the filtrate is now very different. More electrolytes are reabsorbed here, especially sodium, so the filtrate entering the collecting ducts is actually quite dilute. The main function of the collecting ducts is to reabsorb as much water as the body needs.
Active transport takes place at carrier sites in the epithelial membrane, using chemical energy to transport substances against their concentration gradients (p. 37).
Some ions, e.g. sodium and chloride, can be absorbed by both active and passive mechanisms depending on the site in the nephron.
Some constituents of glomerular filtrate (e.g. glucose, amino acids) do not normally appear in urine because they are completely reabsorbed unless blood levels are excessive.
Reabsorption of nitrogenous waste products, such as urea, uric acid and creatinine is very limited.
The kidneys’ maximum capacity for reabsorption of a substance is the transport maximum, or renal threshold. For example, the normal blood glucose level is 3.5–8 mmol/L (63 to 144 mg/100 mL) and if this rises above the transport maximum of about 9 mmol/L (160 mg/100 mL), glucose appears in the urine. This occurs because all the carrier sites are occupied and the mechanism for active transport out of the tubules is overloaded. Other substances reabsorbed by active transport include sodium, calcium, potassium, phosphate and chloride.
The transport maximum, or renal threshold, of some substances varies according to body need at a particular time, and in some cases reabsorption is regulated by hormones.
Hormones that influence selective reabsorption ![]() 13.7
13.7
Parathyroid hormone.
This is secreted by the parathyroid glands and together with calcitonin from the thyroid gland regulates the reabsorption of calcium and phosphate from the distal collecting tubules, so that normal blood levels are maintained. Parathyroid hormone increases the blood calcium level and calcitonin lowers it.
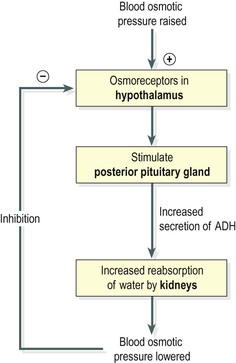
Antidiuretic hormone, ADH.
This is secreted by the posterior pituitary. It increases the permeability of the distal convoluted tubules and collecting tubules, increasing water reabsorption. Secretion of ADH is controlled by a negative feedback system (Fig. 13.12).
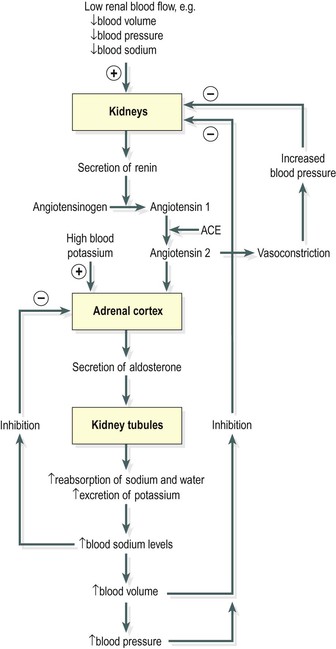
Aldosterone.
Secreted by the adrenal cortex, this hormone increases the reabsorption of sodium and water, and the excretion of potassium. Secretion is regulated through a negative feedback system (Fig. 13.13).
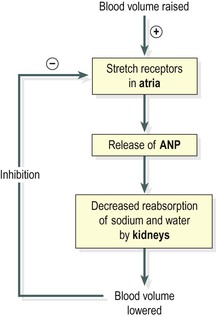
Atrial natriuretic peptide, ANP.
This hormone is secreted by the atria of the heart in response to stretching of the atrial wall when blood volume is increased. It decreases reabsorption of sodium and water from the proximal convoluted tubules and collecting ducts. Secretion of ANP is also regulated by a negative feedback system (Fig. 13.14).
Tubular secretion (Fig. 13.11)  13.8
13.8
Filtration occurs as blood flows through the glomerulus. Substances not required and foreign materials, e.g. drugs including penicillin and aspirin, may not be entirely filtered out of the blood because of the short time it remains in the glomerulus. Such substances are cleared by secretion from the peritubular capillaries into the filtrate within the convoluted tubules. Tubular secretion of hydrogen ions (H+) is important in maintaining normal blood pH.
Summary of urine formation
The three processes involved – filtration, selective reabsorption and tubular secretion – are described above and summarised in Figure 13.15.
Composition of urine
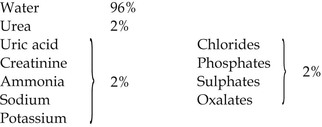
Urine is clear and amber in colour due to the presence of urobilin, a bile pigment altered in the intestine, reabsorbed then excreted by the kidneys (see Fig. 12.37, p. 311). The specific gravity is between 1020 and 1030, and the pH is around 6 (normal range 4.5–8). A healthy adult passes from 1000 to 1500 mL per day. The volume of urine produced and the specific gravity vary according to fluid intake and the amount of solute excreted. The constituents of urine are:
Water balance and urine output
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree