Chapter 15
Resistance and immunity
![]() Animations
Animations
15.1 Phagocytosis 376
15.2 Complement 377
15.3 The acute inflammatory response 377
15.4 T-cells 380
15.5 B-cells 381
15.6 Antibodies 381
Non-specific defence mechanisms.
These protect against any of an enormous range of possible dangers.
Specific defence mechanisms.
These are grouped together under the term immunity. Resistance is directed against only one specific invader. In addition, immunological memory develops, which confers long-term immunity to specific infections. An antigen is anything that stimulates an immune response.
The later sections of the chapter describe the effects of ageing on the immune system, and consider some disorders of lymphatic system function.
Non-specific defence mechanisms
These are the first lines of general defence; they prevent entry and minimise further passage of microbes and other foreign material into the body.
There are five main non-specific defence mechanisms:
Defence at body surfaces
Healthy, intact skin and mucous membranes provide an efficient physical barrier protecting the body’s exposed surfaces. Few pathogens can establish themselves on healthy skin. Sebum and sweat secreted onto the skin surface contain antibacterial and antifungal substances.
Epithelial membranes lining body cavities and passageways exposed to the external environment (e.g. the respiratory, genitourinary and digestive tracts) are more delicate, but are also well defended. Epithelia produce antibacterial secretions, often acidic, containing antibodies and enzymes, as well as sticky mucus for trapping passing microbes.
Hairs in the nose act as a coarse filter, and the sweeping action of cilia in the respiratory tract (Fig. 10.12) moves mucus and inhaled foreign materials towards the throat. Then it is coughed up (expectorated) or swallowed.
The one-way flow of urine from the bladder minimises the risk of infection ascending through the urethra into the bladder. In the female, the acidity of vaginal secretions discourages microbial growth.
Phagocytosis  15.1
15.1
The process of phagocytosis (cell eating) is shown in Figure 4.11, page 69. Phagocytic defence cells such as macrophages and neutrophils are the body’s first line of cellular defence. They actively migrate (chemotaxis, p. 68) to sites of inflammation and infection, because neutrophils themselves and invading microbes release chemicals that attract them (chemoattractants). Phagocytes attack and engulf their targets (Fig. 15.1). They indiscriminately digest and destroy foreign cells, antigenic material and damaged body cells and debris. They may also release chemicals toxic to invading microbes into the interstitial fluid. Macrophages have an important role as a link between the non-specific and specific defence mechanisms. After ingestion and digestion of an antigen, they act as antigen-presenting cells, displaying their antigen on their own cell surface to stimulate T-lymphocytes and activate the immune response (p. 379).
The body’s population of fixed and roaming macrophages (the monocyte-macrophage system) is also discussed in Chapter 4.
Natural antimicrobial substances
Hydrochloric acid.
This is present in high concentrations in gastric juice, and kills the majority of ingested microbes.
This antibacterial enzyme is present in granulocytes, tears, and other body secretions, but not in sweat, urine or cerebrospinal fluid. It destroys bacterial cell walls but does not affect viruses or other pathogens.
Antibodies.
These protective proteins are found coating membranes and in body fluids, and inactivate bacteria (p. 381).
Saliva.
This is secreted into the mouth and washes away food debris that may otherwise encourage bacterial growth. It contains antibodies, lysozyme and buffers to neutralise bacterial acids that promote dental decay.
Interferons.
These chemicals are produced by T-lymphocytes, macrophages and body cells that have been invaded by viruses. They prevent viral replication within infected cells, and the spread of viruses to healthy cells.
Complement ![]() 15.2.
15.2.
Complement is a system of about 20 proteins found in the blood and tissues. It is activated by the presence of immune complexes (an antigen and antibody bound together) and by foreign sugars on bacterial cell walls. Complement:
• binds to, and damages, bacterial cell walls, destroying the microbe
• binds to bacterial cell walls, stimulating phagocytosis by neutrophils and macrophages
• attracts phagocytic cells such as neutrophils into an area of infection, i.e. stimulates chemotaxis.
The inflammatory response  15.3
15.3
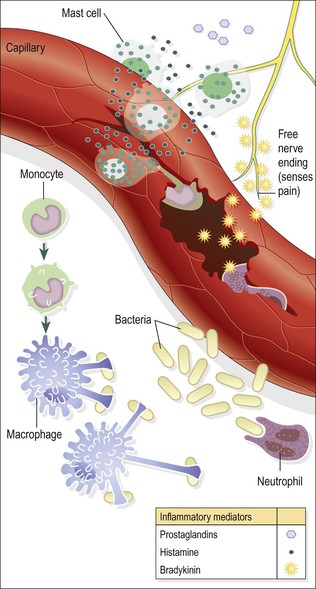
This is the physiological response to tissue damage and is accompanied by a characteristic series of local changes (Fig. 15.2). Its purpose is protective: to isolate, inactivate and remove both the causative agent and damaged tissue, so that healing can take place. The cardinal signs of inflammation are redness, heat, swelling and pain.
Inflammatory conditions are recognised by their Latin suffix ‘-itis’; for example, appendicitis is inflammation of the appendix and laryngitis is inflammation of the larynx.
Causes of inflammation
Any form of tissue damage stimulates the inflammatory response, even in the absence of infection. The wide range of causative agents includes extremes of temperature, trauma, corrosive chemicals including extremes of pH, abrasion and infection by pathogens.
Acute inflammation
Acute inflammation is typically of short duration, e.g. days to a few weeks, and may range from mild to very severe, depending on the extent of the tissue damage. Most aspects of the inflammatory response are hugely beneficial, promoting removal of the harmful agent and setting the scene for healing to follow.
The acute inflammatory response is described here for convenience as a collection of separate events: increased blood flow, accumulation of tissue fluid, migration of leukocytes, increased core temperature, pain and suppuration. In reality, these events significantly overlap and develop together.
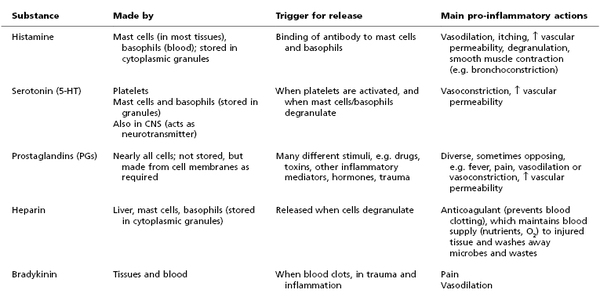
Some of the most important substances released in inflammation are summarised in Table 15.1.
Increased blood flow
Following injury, both the arterioles supplying the damaged area and the local capillaries dilate, increasing blood flow to the site.
This is caused mainly by the local release of a number of chemical mediators from damaged cells, e.g. histamine and serotonin. Increased blood flow to the area of tissue damage provides more oxygen and nutrients for the increased cellular activity that accompanies inflammation. Increased blood flow causes the increased temperature and reddening of an inflamed area, and contributes to the swelling (oedema) associated with inflammation.
Increased tissue fluid formation
One of the cardinal signs of inflammation is swelling of the tissues involved, which is caused by fluid leaving local blood vessels and entering the interstitial spaces.
This is partly due to increased capillary permeability caused by inflammatory mediators such as histamine, serotonin and prostaglandins, and partly due to elevated pressure inside the vessels because of increased blood flow. Most of the excess tissue fluid drains away in the lymphatic vessels, taking damaged tissue, dead and dying cells and toxins with it.
Plasma proteins, normally retained within the bloodstream, also escape into the tissues through the leaky capillary walls; this increases the osmotic pressure of the tissue fluid and draws more fluid out of the blood. These proteins include antibodies, which combat infection, and fibrinogen, a clotting protein. Fibrinogen in the tissues is converted by thromboplastin to fibrin, which forms an insoluble mesh within the interstitial space, walling off the inflamed area and helping to limit the spread of any infection. Some pathogens, e.g. Streptococcus pyogenes, which causes throat and skin infections, release toxins that break down this fibrin network and promote spread of infection into adjacent, healthy tissue.
Sometimes tissue oedema can be harmful. For instance, swelling around respiratory passages can obstruct breathing, and significant swelling often causes pain. On the other hand, the swelling around a painful, inflamed joint cushions it and limits movement, which encourages healing.
Migration of leukocytes
Loss of fluid from the blood thickens it, slowing flow and allowing the normally fast-flowing white blood cells to make contact with, and adhere to, the vessel wall. In the acute stages, the most important leukocyte is the neutrophil, which adheres to the blood vessel lining, squeezes between the endothelial cells and enters the tissues (diapedesis, see Fig. 4.10, p. 69), where its main function is in phagocytosis of antigens. Phagocyte activity is promoted by the raised temperatures (local and systemic) associated with inflammation.
After about 24 hours, macrophages become the predominant cell type at the inflamed site, and they persist in the tissues if the situation is not resolved, leading to chronic inflammation. Macrophages are larger and longer lived than neutrophils. They phagocytose dead/dying tissue, microbes and other antigenic material, and dead/dying neutrophils. Some microbes resist digestion and provide a possible source of future infection, e.g. Mycobacterium tuberculosis (p. 268).
Chemotaxis.
This is the chemical attraction of leukocytes, including neutrophils and macrophages, to an area of inflammation.
Increased temperature
The increased temperature of inflamed tissues has the twin benefits of inhibiting the growth and division of microbes, whilst promoting the activity of phagocytes.
The inflammatory response may be accompanied by a rise in body temperature (fever, pyrexia), especially if there is bacterial infection. Body temperature rises when an endogenous pyrogen (interleukin 1) is released from macrophages and granulocytes in response to microbial toxins or immune complexes. Interleukin 1 is a chemical mediator that resets the temperature thermostat in the hypothalamus at a higher level, causing pyrexia and other symptoms that may also accompany systemic inflammation, e.g. fatigue and loss of appetite. Pyrexia increases the metabolic rate of cells in the inflamed area and, consequently, there is an increased need for oxygen and nutrients.