Chapter Forty. The third stage of labour
Physiology of the third stage of labour
During the 3rd stage, separation and expulsion of the placenta and membranes occur and bleeding from the placental site is minimised through normal haematological and physiological processes. This stage is most hazardous for the mother because of the risk of haemorrhage and other complications (discussed in Chapter 45). The physiological 3rd stage normally lasts from 5 to 30 min but may take up to an hour (NICE 2007). During the second stage of labour, the uterus is steadily emptied, accompanied by accelerated myometrial contraction and retraction.
Separation of the placenta
Separation of the placenta usually begins with the contraction that delivers the baby’s body (Fig. 40.1). The sudden emptying of the uterus with the delivery of the baby rapidly reduces the surface area of the placental site to an area approximately 10 cm in diameter (Blackburn 2007). This reduction in the support base for the placenta leads to compression and shearing of the placenta from the uterine wall. The placenta is compressed so that blood in the intervillous spaces is forced back into the spongy layer of the decidua. Retraction of the oblique muscle fibres constricts the blood vessels supplying the placenta so that the blood cannot drain into the maternal vascular tree. This causes the congested veins to rupture, the villi to shear off the spongy decidua basalis, and the inelastic placenta to become wrinkled and peel away from the uterine wall. The weight of the placenta also increases due to congestion of blood and this helps to strip the membranes off the uterine wall. It is useful to note that the formation of the retroplacental clot is no longer believed to be a (natural) physiological event occurring in the separation process (Blackburn 2007, Wattis 2004).
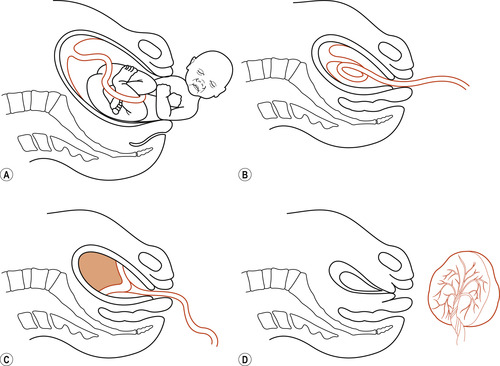 |
| Figure 40.1 The mechanism of placental separation. (A) The placenta before the child is born. (B) The placenta partially separated immediately after the birth of the child. (C) The placenta completely separated. (D) The placenta expelled and the uterus strongly contracted and retracted. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
The placenta may separate from the central area to the borders with inversion so that the fetal surface presents first. This is known as the Schultze mechanism of placental delivery (named after the German anatomist who first described this method). Generations of midwives have termed this process as ‘shiny Schultze’, referring to the glistening appearance of the fetal surface of the placenta at the vulva.
Alternatively, the placenta may separate unevenly from the borders towards the centre with the maternal surface of the placenta appearing at the vulva. This process usually takes longer and there is more risk of incomplete expulsion of the membranes, often referred to as ragged membranes. This mechanism was first described by Matthew Duncan an eminent Scottish gynaecologist (1826–1890) and has been called ‘dirty Duncan’ as an aide-mémoire for students due to the bulky blood ingested at the maternal surface appearing first.
Placentas implanted in the fundus of the uterus are more likely to separate via Schultze mechanism; those implanted lower in the uterine wall usually separate by Duncan mechanism, although these placentas may invert before expulsion (Blackburn 2007).
Control of bleeding
Once separation is complete, the uterus contracts strongly (Fig. 40.2) and the placenta and membranes fall into the lower uterine segment and then into the vagina. It is important to remember that between 450 and 700 ml/min of blood flows to the uterus where 80% is perfusion for the placenta and 20% is perfusion for the myometrium (Murray 2003). This flow must be stopped in seconds to prevent serious haemorrhage. Three factors are involved in the process:
1. Living ligatures: The tortuous uterine blood vessels are surrounded by the oblique muscle fibres, which retract and act as ‘living ligatures’ (Fig. 40.3) and constrict the blood vessels.
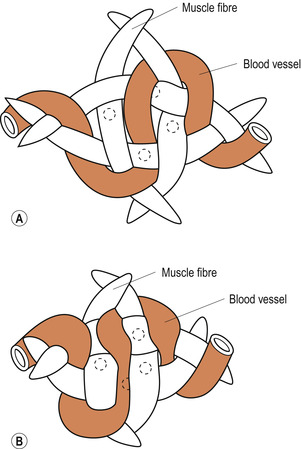 |
| Figure 40.3 How the blood vessels run between the interlacing muscle fibres of the uterus. (A) Muscle fibres relaxed and blood vessels not compressed. (B) Muscle fibres contracted, blood vessels compressed and bleeding arrested. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
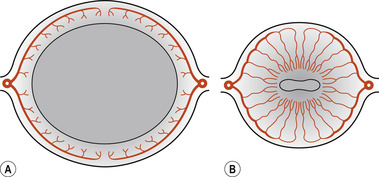 |
| Figure 40.2 Transverse sections of the uterus. (A) Relaxed before the 3rd stage. (B) Contracted and retracted after the 3rd stage; blood vessels are compressed and bleeding arrested. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
2. Pressure: Once the placenta has left the upper segment, a vigorous contraction brings the walls of the uterus in opposition, applying pressure to the placental site.
3. Blood clotting: There is a transitory increase in the activity of the coagulation system during and immediately after placental separation so that clot formation in the torn blood vessels is maximised. The placental site is rapidly covered by a fibrin mesh.
Attaching the baby on the breast will help achieve placental separation and assist with the control of bleeding by causing a release of oxytocin from the maternal posterior pituitary gland resulting in contraction of the uterus, whilst assisting with the above factors.
Management of the third stage of labour
The management of the 3rd stage of labour should be based on an understanding of the physiological process. For at least the last decade there has been as much discussion on the method of management of the 3rd stage of labour. The argument centres on the benefits of active management versus physiological management (also known as expectant or conservative management) of the 3rd stage. Active management involves using a prophylactic oxytocic drug followed by controlled cord traction (Fig. 40.4) to control the length of the 3rd stage and lessen the amount of bleeding. Physiological management involves letting nature take its course; it involves a ‘hands-off approach’, waiting for signs of placental separation and allowing the placenta to deliver spontaneously (possibly aided by gravity and nipple stimulation). The placenta and membranes are expelled by maternal effort but carefully retrieved by the midwife to avoid retention of placental tissue or membranes.
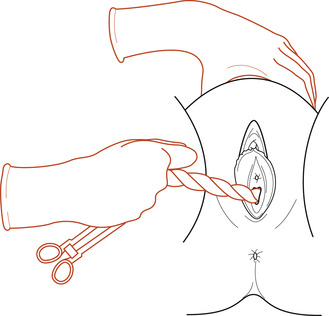 |
| Figure 40.4 Controlled cord traction. (From Henderson C, Macdonald S 2004, with kind permission of Elsevier.) |
The development and use of oxytocic drugs to manage the third stage of labour
There has been a great deal of debate over the last decade about the optimum method for the safe expulsion of the placenta after childbirth (Anderson 2003). Active versus physiological management remains a controversial issue. Begley (1990) reminded us that in the first half of the last century postpartum haemorrhage (PPH) was a major cause of maternal death, with figures between 8% and 22%, depending on when and where the statistics were gathered. Increased availability of blood transfusions, the role of better antenatal care and nutrition in the prevention of anaemia and improved general health of women in westernised countries reduced this to between 4% and 7% by 1978. However, PPH still remains the most common cause of maternal mortality in the world with haemorrhage contributing to 11% of all global maternal deaths (Anderson 2003, Lewis 2007).
Van Dongen & de Groot (1995) wrote an informative historical paper on the use of ergot alkaloids. The alkaloid used in the management of the 3rd stage, ergometrine, was first isolated in 1932 and was synthesised in 1938. The World Health Organization (WHO) (1998) estimated that of over 500 000 (half a million) women who die during childbirth, PPH is one of the most common causes, accounting for 13% of maternal deaths in developed countries but 33% of deaths in developing countries. Latest WHO statistics (WHO 2007) estimate that 536 000 women die every year from complications of pregnancy and childbirth; 99% of these deaths occur in developing countries.
The first routine use of intramuscular ergometrine 0.5 mg was in 1951 and it was given as the head crowned. This shortened the 3rd stage of labour and reduced blood loss in all deliveries but, more significantly, it reduced the incidence of PPH. However, van Dongen & de Groot (1995) also mention that oxytocin is as efficient as ergometrine without its dangers. The risks associated with the administration of ergometrine are severe hypertension, nausea and vomiting, and side-effects due to vasoconstriction. Maternal deaths have occurred following its administration and for these reasons the writers considered that the administration of oxytocin may be safer.
Begley (1990) cited Embrey et al (1963), who compared the use of intramuscular ergometrine with intramuscular Syntometrine, a product combining ergometrine (500 μg) and synthetic oxytocin (5 IU), and this rapidly became the drug of choice in Britain. Figure 40.5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


