Chapter Thirty-Eight. Pain relief in labour
CHAPTER CONTENTS
Introduction 517
Pain perception 517
Pain pathways in labour 521
The effect of pain 521
Introduction
The experience of pain can be discussed on three levels: pain transmission and perception; pain reception; and pain modulation. Pain is a complex process and is experienced differently depending on the following factors: the physiological process, the context and the previous experience of an individual. Pain can be modulated at different points in the physiological pathway and by education aimed at achieving an understanding of the accompanying events and the meanings attached to them by individuals and by their culture. Walsh (2007) highlights two models of dealing with labour pain (Table 38.1) and informs us that the ‘working with the pain relief approach’ rather than the ‘pain relief approach’ would be an important model for midwives to adopt when caring for labouring women. The terminology and philosophy underpinning the approach takes into consideration that pain is a normal physiological process when it comes to childbirth. However, this does not always alter people’s perception of pain related to birth.
| Pain relief approach | Working with pain approach |
|---|---|
| Language suggestive of pain as a problem | Language suggestive of pain as normative |
| Paternalistic ‘we can protect you from uneccessary stress’ | Egalitarian empowerment ‘we are alongside you’ |
| Techno/rationalism age, pain is preventable/treatable | Labour pain timeless component of ‘rite-of-passage’ transitions |
| Neutral impact of environment | Seminal impact of environment |
| Clinical expertise of professional companions | Supportive role of birth carers |
| Special session/focus in antenatal education | Woven throughout labour preparation sessions |
| ‘Menu approach’ to options for coping with pain | Supportive strategies for journey of labour |
| Pain as a management issue for assembly-line birth | Pain as one dimension of labour care in one-to-one, small-scale birth setting |
| Contributes to trend of rising birth rates | Contributes to trend of less pharmacological analgesia |
| Risks of pharmacological agents outweighed by benefits | ‘Cascade of intervention’ dynamic |
| First birth special case for ‘menu approach’ | First birth optimal opportunity for ‘working with pain’ |
| Informed choice means all options must be presented | Informed choice within context of birthing plan and philosophy |
Pain perception
The nature of pain depends not just on physiological parameters such as the part of the body affected and the extent of the injury but also on the psychological reaction to the pain (Allan et al 1996). McCaffery (1983) reminded us of the cognitive and emotional inputs into pain perception, stating that pain is what the patient says it is and exists when he says it does. Bryant & Yerby (2004) wrote that pain ‘is a complex, personal, subjective, multifactorial phenomenon which is influenced by psychological, physiological and sociocultural factors’. In similar fashion, Carlson (2004) reminds us that pain is not purely physical. Pain can be modified by placebo drugs, emotions and other stimuli such as acupuncture. The translation of pain messages into unpleasant feelings ensures that an individual avoids repeating the experience if possible. These are important factors in the management of pain.
Whereas the physiological threshold for pain sensation appears to be similar in all people, the cognitive and emotive factors alter the individual’s reaction to pain and the meaning attached to the experience. The anticipation of pain increases anxiety levels and the perceived intensity of pain. Hayward (1975) demonstrated that knowledge of events reduces anxiety and pain and this applies to pain in labour. Interesting work has been done by Walding (1991) on the ‘locus of control’ theory which suggests that pain is perceived as less threatening and with less intensity if women believe they are in control of events. Placing the woman at the centre of her care should therefore make labour less painful and less traumatic, even if problems such as occipitoposterior position occur.
Pain may also increase the level of catecholamines released into the blood. This in turn has the usual result of increased heart and respiration rate with decreased blood flow to the internal organs such as the uterus. The uterus in labour needs a good delivery of oxygen and nutrients to enable efficient contractions, and thus anxiety and fear increase pain, reduce uterine blood supply and may prolong labour.
Pain reception
The principle of pain reception is that several million bare sensory nerve endings weave their way through all the tissues and organs of the body (except the brain) and respond to noxious stimuli.
A chemical released from damaged tissue seems to act as a universal pain stimulus. This is bradykinin, which in turn releases inflammatory chemicals such as histamine and prostaglandin. Bradykinin is thought to bind to receptor endings, resulting in an action potential. However, pain perception is much more than the simple sensation relayed by neurons.
Classification of pain
Pain can be classified as somatic or visceral. Somatic pain arising from skin, muscles or joints can be deep or superficial. Superficial pain tends to be brief, highly localisable and sharp or pricking in character. This pain is transmitted along large myelinated fibres—the Aδ fibres. Deep somatic pain is more likely to be described as burning or aching; it is more diffuse and longer lasting and always indicates tissue destruction. Impulses travel along small unmyelinated fibres called C fibres. A third type of fibre, the myelinated Aβ fibre, relays light touch.
Pain pathways
Visceral pain results from the body’s viscera or organs; it is described as burning, gnawing or aching. Visceral sensory neurons (afferents) accompany autonomic sympathetic and parasympathetic fibres and send information about chemical changes, distension or irritation of the viscera. Both somatic and visceral pain stimuli pass along the dendrites of the first-order neurons to their cell bodies in the dorsal root ganglia. Their axons leave the dorsal root ganglia to enter the spinal cord and synapse with second-order neurons in the dorsal horns of the spinal cord. The pain impulse causes the release of the pain neurotransmitter, substance P, from the presynaptic membrane into the synaptic cleft.
The anatomy of the dorsal horn
The cells in the spinal cord are arranged in laminae (layers) in a dorsal–ventral direction and running the full length of the spinal cord (Fig. 38.1). The dorsal horn contains six laminae numbered from the tip of the horn inwards. The ventral horn contains three other laminae and another column of cells, lamina X, is clustered around the central canal. Laminae I and II are visible to the naked eye as a clear zone and are together called the substantia gelatinosa.
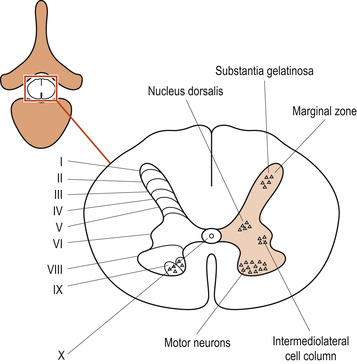 |
| Figure 38.1 Laminae (I–X) and named cell groups at mid-thoracic level. (From Montague S E, Watson R, Herbert R A 2005, with kind permission of Elsevier.) |
Ascending pathways
Sensory fibres returning to the dorsal horns do so in an orderly fashion (Fig. 38.2). The rule is that the thicker the fibre, the deeper it penetrates. The unmyelinated C fibres do not penetrate past lamina II; the small myelinated Aδ fibres mainly terminate in laminae I and II although a few make it to lamina V. The large myelinated fibres from the skin end mainly in laminae IV, V and VI. The specialised large muscle stretch afferents reach level VI (Melzack & Wall 1988).
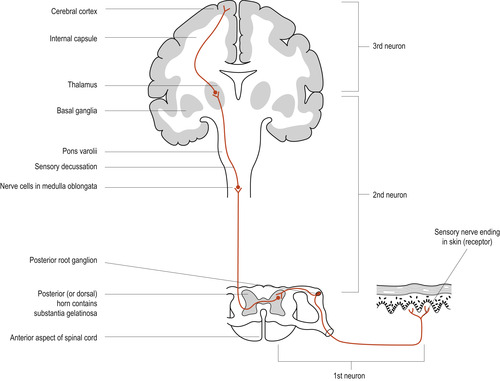 |
| Figure 38.2 The sensory pathway showing the structures involved in the appreciation of pain. (Reproduced with permission from Bevis 1984.) |
The axons of most of the second-order neurons cross the cord and enter the anterolateral spinothalamic tracts to ascend to the thalamus (Fitzgerald & Folan-Curran 2002). There they synapse with third-order neurons to pass the pain message to the sensory cortex for interpretation. The second-order fibres may make abundant synapses in the brainstem, hypothalamus and limbic system before reaching the thalamus. This will add a state of arousal and emotion to the perception of pain. The limbic system is the affective (emotional) part of the brain, where emotions and thoughts are closely linked (Marieb & Hoehn 2008). This would explain why Walsh (2007) argues that ‘working with the pain relief approach’ model is more advantageous as it deals with these aspects.
Pain modulation
Control systems descending from the brain
Nerve fibres descending in the white matter penetrate into the grey matter and innervate the nearest cells. The dorsolateral column is therefore able to send axons to the most dorsal laminae. In particular, fibres from the raphe, the locus caeruleus in the reticular formation and from the hypothalamus as well as the pyramidal tract from the cortex innervate the dorsal laminae III–VI. Descending fibres synapse in the dorsal horns and further modify the final ascending message by releasing endogenous opiates such as endorphins and encephalins into the synaptic cleft (Hughes et al 1975). Endogenous opiates have been shown to inhibit prostaglandin production. Prostaglandin is thought to be a key chemical necessary for pain perception.
The gate control theory of pain
In order to understand the theory of Melzack & Wall (1988), it is necessary to keep the following in mind:
• The ascending and descending tracts in the spinal cord.
• The relative conduction speeds of sensory nerve fibres returning to the spinal cord.
• The anatomy of the dorsal horns of the spinal cord.
Any theory of pain must explain several facts about pain perception (Melzack & Wall 1988):
• The high variability between injury and pain.
• The production of pain by innocuous stimuli.
• The perception of pain in areas seemingly removed from the area of damage.
• The persistence of pain in the absence of injury or after healing.
• The change in the location and nature of pain over time.
• The multidimensional nature of pain.
• The lack of treatment for some types of pain such as arthritic pain and migraines.
Melzack & Wall (1988) described their updated gate control theory of pain which they first proposed in 1965 (Fig. 38.3). Although they would emphasise that there is still work to be done to complete their understanding, most people would agree that the gate control theory offers satisfactory explanations for some of the above unusual phenomena.
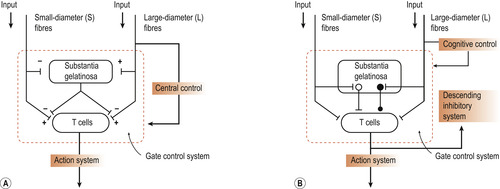 |
| Figure 38.3 The gate control theory of pain. (A) Original formulation of the theory. Large diameter (L) and small diameter (S) peripheral nerve fibres input to the substantia gelatinosa (SG) and to the first central transmission (T) cells of the spinal cord. The inhibitory effect exerted by the SG on the T cells is increased by activity of the S fibres (pain fibres). The central control mechanisms are represented as running from the L fibre system and feeding back to the gate control. (B) Updated model. On the basis of subsequent evidence, Melzack & Wall formulated the gate control theory to include excitatory (white circle) links from the SG to the T cells, as well as descending inhibitory control from the brainstem. All synaptic connections are excitatory except the inhibitory link from SG to T. The round knob at this inhibitory synapse implies that its action may be presynaptic, postsynaptic or both. (Reproduced with permission from Melzack & Wall 1988.) |
The essence of the gate control theory
Gating of the spinothalamic tract response to C fibre activity can be achieved by stimulating large myelinated mechanoreceptor afferents by rub or tickle. These impulses inhibit the ascending pain impulse. Inputs from the large myelinated fibres conveying touch and smaller Aδ and C fibres conveying pain interact at the level of the spinal cord. The large-diameter sensory nerve impulses come into the spinal cord more rapidly. This normally inhibits the slower smaller fibre pain impulses presynaptically. This inhibition constitutes the gate that is normally closed against small-diameter fibre impulses unless the stimulation is so great that it overcomes the gate (Fig. 38.3).
Other modifications of the ascending pain impulse take place in the substantia gelatinosa:
• Interneurons in the substantia gelatinosa can regulate and amplify the impulse conducted to the brain via the ascending pathways.
• Descending fibres synapse in the same area of the spinal cord and further modify the final ascending message by releasing endogenous opiates such as endorphins and encephalins into the synaptic cleft (see above text).
• Virtually all of the brain plays a part in pain perception; the thalamus, reticular system, limbic system and cortex add their effects to the physical, emotional and cognitive experience of pain.
Knowledge of the multidimensional nature of pain perception allows the management of pain to be approached in an equally multidimensional manner. Techniques to inhibit the gate include stimulation of the large nerve fibres so that the pain impulses from the smaller fibres are blocked. Methods include heat, massage and pressure. Transcutaneous electrical nerve stimulation (TENS) works by applying a stimulating electrode to the skin at the level of the noxious C fibre activity and delivering an electrical current sufficient to cause a buzzing sensation (Fitzgerald & Folan-Curran 2002). Descending fibre impulses can also inhibit transmission of pain by release of natural opiates and concentration techniques may work in this way (Blackburn 2007).
Visceral sensory neurons
Although the autonomic nervous system (ANS) is considered to be a motor system, there are sensory neurons, mainly visceral pain afferents, in autonomic nerves. These visceral pain afferents travel along the same pathways as somatic pain fibres. Pain perception is referred to the somatic area of the specific dermatome of the surface of the body: for example, the pain of a heart attack is felt in the chest and along the medial aspect of the left arm.
Pain pathways in labour
Both visceral and somatic pain are perceived in labour. Visceral pain is caused by the uterine contractions, the dilatation of the cervix and, later, by the stretching of the vagina and pelvic floor. The body of the uterus is served by autonomic nerves originating in thoracic 11 and 12 and lumbar 1 vertebrae (Fig. 38.4). Sensation from the body of the uterus is perceived as pain in response to stretch, infection and contraction and possibly ischaemia.
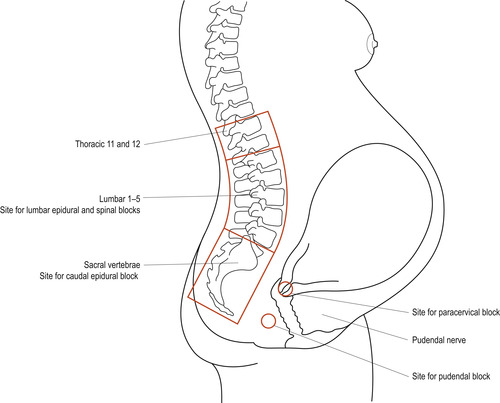 |
| Figure 38.4 Pain pathways in labour, showing the sites at which pain may be intercepted by local anaesthetic technique. (Reproduced with permission from Bevis 1984.) |
The cervix is innervated by the sacral plexus from sacral 2, 3 and 4 vertebrae nerves (Fig. 38.4), which then pass through the transcervical nerve plexi. Pain sensation from the cervix is in response to rapid dilatation. Somatic pain is caused by the pressure of the fetus as it distends the birth canal, vulva and perineum. Sensations from the pelvic floor are relayed from the pudendal nerve to the sacral plexus. Pain during the first stage of labour may be referred as nerve impulses from the uterus and cervix stimulate spinal cord neurons that innervate the abdominal wall. Pain may be felt between the umbilicus and the symphysis pubis, and around the iliac crests to the buttocks. It may radiate down the thighs and into the lumbar and sacral regions of the back.
The effect of pain
Besides the physical, emotional and cognitive factors affecting pain perception, abnormalities of labour may cause an increase in the pain perceived. Pain may be increased in labour complicated by prolongation, occipitoposterior position and borderline cephalopelvic disproportion.
Pain is a form of stress and may cause increased levels of catecholamine secretion; these substances will cause the following signs (Hamilton 2003):
• Increased cardiac output.
• Increased heart rate.
• A rise in blood pressure.
• Hyperventilation.
• Maternal alkalosis.
• Decreased cerebral and uterine blood flow due to vasoconstriction.
• Decreased uterine contractions.
• Delayed stomach emptying, leading to nausea and vomiting.
• Delayed bladder emptying.
Management of pain
Understanding of pain pathways and perception leads to the offering of a reasonable range of interventions. Care may include pharmacological and non-pharmacological methods of pain relief. Carers can offer:
• Non-pharmacological support.
• Transcutaneous electrical nerve stimulation (TENS).
• Systemic analgesia.
• Tranquillisers.
• Inhalational analgesia.
• Regional and local analgesia.
• Alternative methods.
Non-pharmacological support
Antenatal preparation
Pain management ideally begins during the antenatal period. Women should be given the opportunity to discuss their anxieties and fears and be given information about pain relief at a level they are able to understand. Every person’s needs are different but all women should participate in the planning of care in labour, including the choice of pain relief. There should be no feeling of finality in the choice made: women need to understand and feel reassured that they can change their minds during the course of labour, depending on their actual experience of pain. Some women may wish to attend preparation classes.
During labour
Environment
The environment is important. When women and their partners enter the labour environment it is essential that they find the atmosphere and attitude of staff to be relaxed, friendly and welcoming. This is often more powerful at putting them at ease than the physical surroundings themselves, which also have a role to play (Simkin & Ancheta 2005). The room should be furnished comfortably but in such a way that any emergency treatment needed can be carried out swiftly and efficiently (Hamilton 2003). Wallpaper, curtains and screens can be useful in creating a restful atmosphere. There is a move towards informal furnishings such as beanbags, reclining chairs and rocking chairs in many units. Music and television can provide pleasure and distraction for some women in early labour (Simkin & Ancheta 2005).



