The Superficial Back Line
This first line, the Superficial Back Line (SBL) (Fig. 3.1), is presented in considerable detail, in order to clarify some of the general and specific Anatomy Trains concepts. Subsequent chapters employ the terminology and format developed in this chapter. Whichever line interests you, it may help to read this chapter first.
Overview
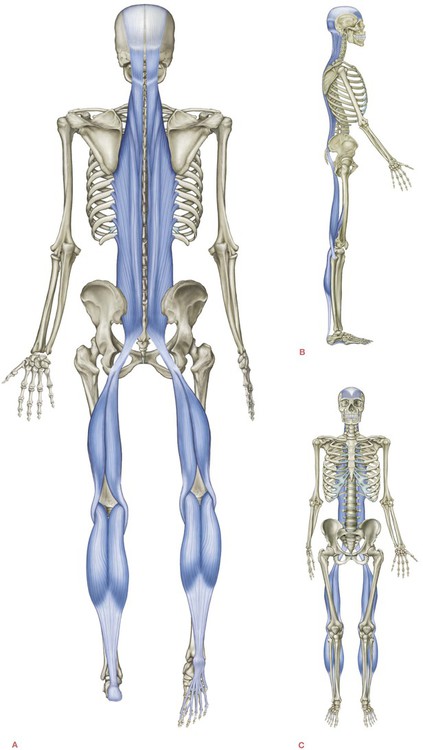
The Superficial Back Line (SBL) connects and protects the entire posterior surface of the body like a carapace from the bottom of the foot to the top of the head in two pieces – toes to knees, and knees to brow (Fig. 3.2/Table 3.1). When the knees are extended, as in standing, the SBL functions as one continuous line of integrated myofascia. The SBL can be dissected as a unity, seen here both on its own and laid over a plastic classroom skeleton (Figs 3.3 and 3.4).
Table 3.1
Superficial Back Line: myofascial ‘tracks’ and bony ‘stations’ (Fig. 3.2)
| Bony stations | Myofascial tracks | |
| Frontal bone, supraorbital ridge | 13 | |
| 12 | Galea aponeurotica/epicranial fascia | |
| Occipital ridge | 11 | |
| 10 | Sacrolumbar fascia/erector spinae | |
| Sacrum | 9 | |
| 8 | Sacrotuberous ligament | |
| Ischial tuberosity | 7 | |
| 6 | Hamstrings | |
| Condyles of femur | 5 | |
| 4 | Gastrocnemius/Achilles tendon | |
| Calcaneus | 3 | |
| 2 | Plantar fascia and short toe flexors | |
| Plantar surface of toe phalanges | 1 |
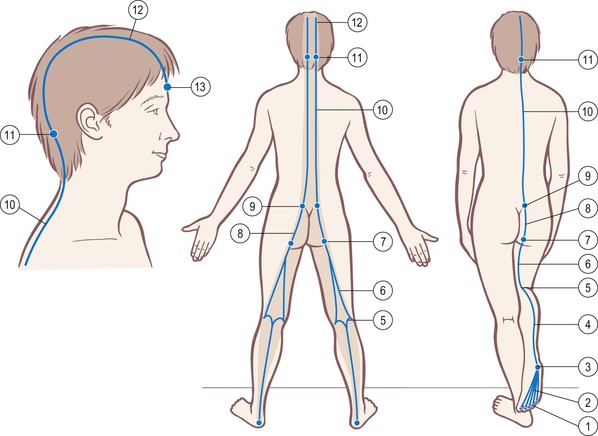
Fig. 3.2 Superficial Back Line tracks and stations. The shaded area shows where it affects and is affected by the more superficial fasciae (dermis, adipose, and the deeper fascia profundis).
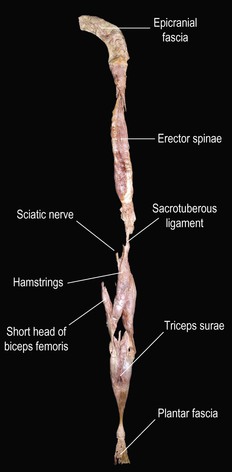
Fig. 3.3 The Superficial Back Line dissected away from the body and laid out as a whole. The different sections are labeled, but the dissection indicates the limitation of thinking solely in anatomical ‘parts’ in favor of seeing these meridians as functional ‘wholes’.

Fig. 3.4 The same specimen laid out on a classroom skeleton to show how the whole is arrayed. The cadaver was a good deal taller than the skeleton.
Movement function
With the exception of flexion from the knees on down, the overall movement function of the SBL is to create extension and hyperextension. In human development, the muscles of the SBL lift the baby’s head from embryological flexion, with progressive engagement and ‘reaching out’ through the eyes, supported by the SBL down through the rest of the body to the ground – belly, seat, knees, feet – as the child achieves stability in each of the developmental stages leading to upright standing about one year after birth (Fig. 3.5).
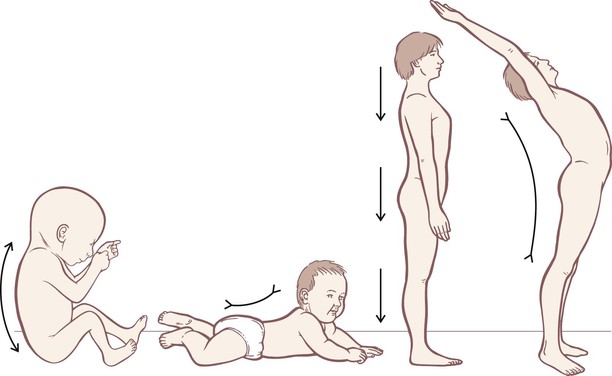
Fig. 3.5 In development, the SBL shortens to move us from a fetal curve of primary flexion toward the counterbalancing curves of upright posture. Further shortening of the muscles of the SBL produces hyperextension.
The Superficial Back Line in detail
General considerations
Common postural compensation patterns associated with the SBL include: ankle dorsiflexion limitation, knee hyperextension, hamstring shortness (substitution for inadequate deep lateral rotators), anterior pelvic shift, sacral nutation, lordosis, extensor widening in thoracic flexion, suboccipital limitation leading to upper cervical hyperextension, anterior shift or rotation of the occiput on the atlas, and eye–spine movement disconnection.
From toes to heel
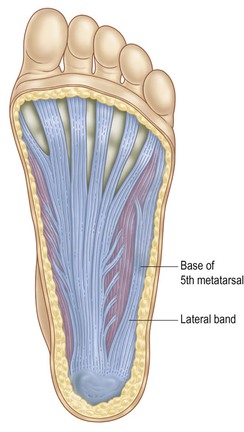
These five bands blend into one aponeurosis that runs into the front of the heel bone (the antero-inferior aspect of the calcaneus). The plantar fascia picks up an additional and important 6th strand from the 5th metatarsal base, the lateral band, which blends into the SBL on the outside edge of the heel bone (Figs 3.6 and 3.7).

Fig. 3.7 A dissection of the plantar fascia. Notice the lateral band (A) comprising a somewhat separate but related track. (©Ralph T. Hutchings. Reproduced from McMinn, et al. 1993.)
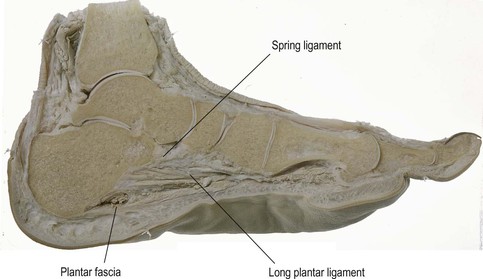
These fasciae, and their associated muscles that pull across the bottom of the foot, form an adjustable ‘bowstring’ to the longitudinal foot arches; this bowstring helps to approximate the two ends, thus maintaining the heel and the 1st and 5th metatarsal heads in a proper relationship (Fig. 3.8). The plantar aponeurosis constitutes only one of these bowstrings – the long plantar ligament and spring ligament also provide shorter and stronger bowstrings deeper (more cephalad) into the tarsum of the foot (visible below the subtalar joint in Fig. 3.9, see also Fig 3.34).
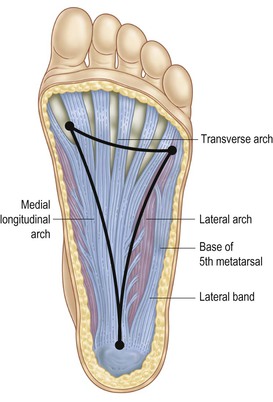
Fig. 3.8 The plantar aponeurosis forms a ‘trampoline’ under the arches – one springy arch between each point of contact: the 5th metatarsal head, the 1st metatarsal head, and the heel.
The plantar fascia
Compare the inner and outer aspect of your client’s foot. While the outer part of the foot (base of little toe to heel) is always shorter than the inner aspect (from base of big toe to heel), there is a common balanced proportion. If the inner aspect of the foot is proportionally short, the foot will often be slightly lifted off the medial surface (as if supinated or inverted) and seemingly curved toward the big toe in a ‘cupped hand’ pattern, as if a slightly cupped hand were placed palm down on the table. In these cases, it is the medial edge of the plantar fascia that needs opening.
Even in the relatively balanced foot, the plantar surface can usually benefit from enlivening work to make it more supple and communicative, especially in our urbanized culture where the feet stay locked up in leather coffins all day. A default approach to the plantar tissues is to lengthen between each of the points that support the arches: the heel, the 1st metatarsal head, and the 5th metatarsal head (Fig. 3.8).
A simple test
![]()
![]() For a sometimes dramatic and easily administered test of the relatedness of the entire SBL, have your client do a forward bend, as if to touch the toes with the knees straight (Fig. 3.10). Note the bilateral contour of the back and the resting position of the hands. Draw your client’s attention to how it feels along the back of the body on each side.
For a sometimes dramatic and easily administered test of the relatedness of the entire SBL, have your client do a forward bend, as if to touch the toes with the knees straight (Fig. 3.10). Note the bilateral contour of the back and the resting position of the hands. Draw your client’s attention to how it feels along the back of the body on each side.

Fig. 3.10 A forward bend with the knees straight links and challenges all the tracks and stations of the Superficial Back Line. Work in one area, as in this move for the plantar fascia, can affect motion and length anywhere and everywhere along the line. After work on the right plantar surface, the right arm hangs lower.
Have your client return to standing and roll a tennis ball (or a golf ball for the hardy) deeply into the plantar fascia on one foot only, being slow and thorough with the pressure rather than fast and vigorous. Keep it up for at least a couple of minutes, making sure the whole territory is covered from the ball of all five toes back to the front edge of the heel, the whole triangle shown in Figure 3.8.
Heel spurs
![]()
![]() It is ‘common knowledge’ that the muscles attach to bones – but this commonsense view is simply not the case for most myofasciae. The plantar fascia is a good case in point. People who run on the balls of their feet, for instance, or others who, for some reason, put repetitive strain on the plantar fascia, tug constantly on the calcaneal attachment of the plantar fascia. Since this fascia is not really attached to the calcaneus but rather blends into its periosteal ‘plastic wrap’ covering, it is possible in some cases for the periosteum to be progressively tugged away from the calcaneus, creating a space, a kind of ‘tent’, between this fabric and the bone (Fig. 3.11).
It is ‘common knowledge’ that the muscles attach to bones – but this commonsense view is simply not the case for most myofasciae. The plantar fascia is a good case in point. People who run on the balls of their feet, for instance, or others who, for some reason, put repetitive strain on the plantar fascia, tug constantly on the calcaneal attachment of the plantar fascia. Since this fascia is not really attached to the calcaneus but rather blends into its periosteal ‘plastic wrap’ covering, it is possible in some cases for the periosteum to be progressively tugged away from the calcaneus, creating a space, a kind of ‘tent’, between this fabric and the bone (Fig. 3.11).
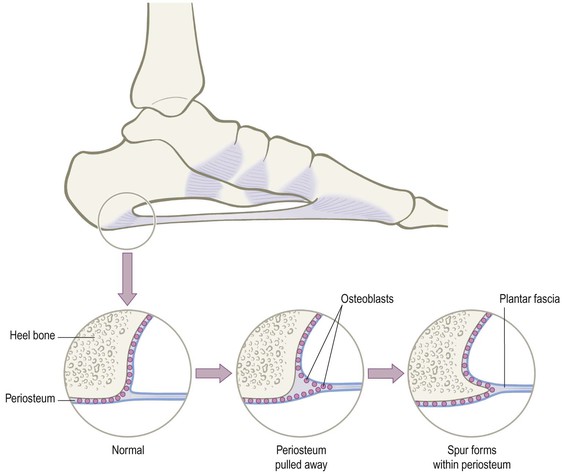
Fig. 3.11 The formation of a heel spur by the osteoblasts which fill in under a pulled-away periosteum illustrates both the adaptability of the connective tissue system and one limitation of the simplistic ‘muscles attach to bones’ concept.
From heel to knee
![]() As discussed in Chapter 2, the fasciae do not just attach to the heel bone and stop (as implied in Fig. 3.11). They actually attach to the collagenous covering of the calcaneus, the periosteum, which surrounds the bone like a tough plastic wrapping. If we begin to think in this way, we can see that the plantar fascia is thus continuous with anything else that attaches to that periosteum. If we follow the periosteum around the calcaneus, especially underneath it around the heel to the posterior surface (following a thick and continuous band of fascia – see Figs 3.12 and 3.15B), we find ourselves at the beginning of the next long stretch of track that starts with the Achilles tendon (Figs 3.12 and 3.13).
As discussed in Chapter 2, the fasciae do not just attach to the heel bone and stop (as implied in Fig. 3.11). They actually attach to the collagenous covering of the calcaneus, the periosteum, which surrounds the bone like a tough plastic wrapping. If we begin to think in this way, we can see that the plantar fascia is thus continuous with anything else that attaches to that periosteum. If we follow the periosteum around the calcaneus, especially underneath it around the heel to the posterior surface (following a thick and continuous band of fascia – see Figs 3.12 and 3.15B), we find ourselves at the beginning of the next long stretch of track that starts with the Achilles tendon (Figs 3.12 and 3.13).
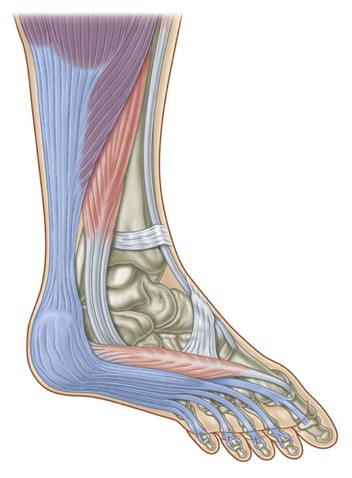
Fig. 3.12 Around the heel, there is a strong and dissectable fascial continuity between the plantar fascia and the Achilles tendon and its associated muscles.

Fig. 3.13 A dissection of the heel area demonstrates the continuity from plantar tissues to the muscles in the superficial posterior compartment of the leg. (© Ralph T. Hutchings. Reproduced from Abrahams, et al. 1998.)
Because the Achilles tendon must withstand so much tension, it is attached not only to the periosteum but also into the collagenous network of the heel bone itself, just as a tree is rooted into the ground. Leaving the calcaneus and its periosteum, our train passes up, getting wider and flatter as it goes (Fig. 3.12). Three myofascial structures feed into the Achilles tendon: the soleus from the profound side, the gastrocnemius from the superficial side, and the little plantaris in the middle.
Heel as arrow
![]()
![]()
![]() In simple terms, the heel is the patella of the ankle, as we can see in the X-ray of a foot (Fig. 3.14). From a ‘tensegrity’ point of view, the calcaneus is a compression strut that pushes the tensile tissues of the SBL out away from the ankle to create proper tone around the back of the tibio-talar fulcrum, with the soft tissue spanning from knee to toes. (Contrast this leverage with the proximity of the joint-stabilizing muscles: the fibularii (peroneals) of the Lateral Line that snake right around the lateral malleolus. Similarly, the long toe flexors of the Deep Front Line pass close behind the medial malleolus, lending them more stabilization advantage, but less leverage for jumping.)
In simple terms, the heel is the patella of the ankle, as we can see in the X-ray of a foot (Fig. 3.14). From a ‘tensegrity’ point of view, the calcaneus is a compression strut that pushes the tensile tissues of the SBL out away from the ankle to create proper tone around the back of the tibio-talar fulcrum, with the soft tissue spanning from knee to toes. (Contrast this leverage with the proximity of the joint-stabilizing muscles: the fibularii (peroneals) of the Lateral Line that snake right around the lateral malleolus. Similarly, the long toe flexors of the Deep Front Line pass close behind the medial malleolus, lending them more stabilization advantage, but less leverage for jumping.)
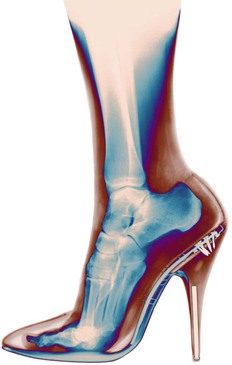
Fig. 3.14 This X-ray of a dancer’s foot shows how the calcaneus functions in a way parallel to the patella – what the patella does on the front of the knee, the calcaneus does on the back of the ankle – namely, pushing the soft tissue away from the fulcrum of the joint to give it more leverage. (© Bryan Whitney, reproduced with permission.)
To see the clinical problem this patterning can create, imagine this lower section of this Superficial Back fascial line – the plantar fascia and Achilles-associated fascia – as a bowstring, with the heel as an arrow (Fig. 3.15). As the SBL chronically over-tightens (common in those with the ubiquitous postural fault of a forward lean of the legs: an anterior shift of the pelvis), it is capable of pushing the heel forward into the subtalar joint; or, in another common pattern, such extra tension can bring the tibia–fibula complex posteriorly on the talus, which amounts to the same thing.
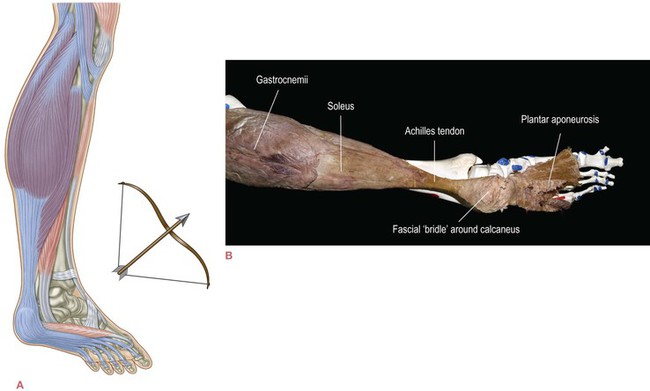
Fig. 3.15 When the myofascial continuity comprising the lower part of the SBL tightens, the calcaneus is pushed into the ankle, as an arrow is pushed by the tautened bowstring (A). Notice how the fascia around the heel acts as a ‘bridle’ or a ‘cup’ to embrace and control the heel bone (B).
To assess this, look at your client’s foot from the lateral aspect as they stand, and drop an imaginary vertical line down from the lower edge of the lateral malleolus (or, if you prefer, place your index finger vertically down from the tip of the malleolus to the floor). See how much of the foot lies in front of this line and how much behind. Anatomy dictates that there will be more foot in front of the line, but, with a little practice, you will be able to recognize a normal proportion (Fig. 3.16A) versus comparatively little heel behind this line (Fig. 3.16B).


Fig. 3.16 The amount of the foot in front of the ankle joint should be balanced by about  to
to  behind the ankle joint. Without this support for the back body, the upper body will lean forward to place the weight in front.
behind the ankle joint. Without this support for the back body, the upper body will lean forward to place the weight in front.
• ![]() release the plantar fascia, including the lateral band, in the direction of the heel (DVD ref: Superficial Back Line, 10:57–16:34, 20:29–22:25);
release the plantar fascia, including the lateral band, in the direction of the heel (DVD ref: Superficial Back Line, 10:57–16:34, 20:29–22:25);
• ![]() release the superficial posterior compartment of the leg (soleus and gastrocnemius) down toward the heel (DVD ref: Superficial Back Line, 22:27–24:30);
release the superficial posterior compartment of the leg (soleus and gastrocnemius) down toward the heel (DVD ref: Superficial Back Line, 22:27–24:30);
• mobilize the heel by stabilizing the front of the tarsum with one hand while working the heel through its inversion and eversion movements in your cupped hand.
In more recalcitrant cases, it may be necessary to further release the ligaments of the ankle by working deeply but slowly from the corner of each malleolus (avoiding the nerves) diagonally to the postero-inferior corner of the heel bone. The result will be a small but visible change in the amount of foot behind the malleolar line, and a very palpable change in support for the back of the body in the client. Therefore, strategically, this work should precede any work designed to help with an anterior pelvic shift.
‘Expresses’ and ‘locals’
![]()
![]()
![]() Two large muscles attach to the Achilles band: the soleus from the deep side, and the gastrocnemius from the superficial side (Fig. 3.15a). The connection of the SBL is with the superficial muscle, the gastrocnemius. First, however, we have an early opportunity to demonstrate another Anatomy Trains concept, namely ‘locals’ and ‘expresses’.
Two large muscles attach to the Achilles band: the soleus from the deep side, and the gastrocnemius from the superficial side (Fig. 3.15a). The connection of the SBL is with the superficial muscle, the gastrocnemius. First, however, we have an early opportunity to demonstrate another Anatomy Trains concept, namely ‘locals’ and ‘expresses’.
The importance of differentiating expresses and locals lies in this postural position is most often held in the underlying locals, not in the more superficial expresses. Express trains of myofascia cross more than one joint; locals cross, and therefore act on, only one joint. With some exceptions in the forearms and lower leg, the locals are usually deeper in the body – more profound – than the expresses. (See Ch. 2 for a full definition and examples.)
Derailment
In order to understand this first important exception, we need to look more closely at the interface between the two heads of the gastrocnemius and the tendons of the three hamstrings (Fig. 3.17).

Fig. 3.17 The relationship between the heads of the gastrocnemii and the tendons of the hamstrings in the popliteal space behind the knee. (© Ralph T. Hutchings. Reproduced from Abrahams, et al. 1998.) See also Figure 3.3.
It is easy to see from comparing with Figure 3.17 that the gastrocnemius and hamstrings are both separate and connected. In dissection, strong areolar fascia clearly links from near the distal ends of the hamstrings to near the proximal ends of the gastrocnemii heads. In Figure 3.17 this tissue has been dissected away; in Figure 3.3 it has been retained. Such areolar tissue, long thought to be simply a passive ‘filler’, has now been shown to be an effective force transmitter when tightened.1
In practice, then, flexion of the knees delinks the one from the other. While by strict Anatomy Trains rules they are a myofascial continuity, they do function as one primarily when the knee is extended. The gastrocnemii heads reach up and around the hamstring tendons to insert onto the upper portions of the femoral condyles. The hamstrings reach down and around the gastrocnemii to attach to the tibia and fibula. As long as the knee is bent, these two myofascial units go their own ways, neighboring but loosely connected (Fig. 3.18A). As the knee joint comes into extension, however, the femoral condyles come back into tightening the tendon complex, engaging these elements with each other, and making them function together almost as if they were two pairs of hands gripped at the wrists (Fig. 3.18B–D). This configuration also bears a strong resemblance to a square knot, loosened when the knee is bent, tightened as the knee straightens.
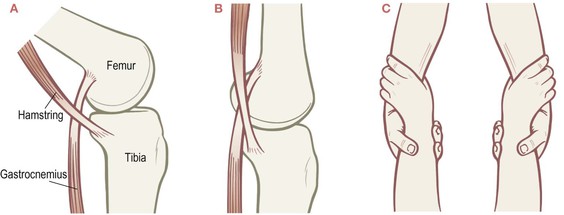
Fig. 3.18 When the knee is flexed, the myofascia of the thigh and the myofascia of the lower leg function separately (A). When the knee is extended, these myofasciae link into one connected functioning unit (B), like the interlocked hands of a pair of trapeze artists (C – compare to Fig. 3.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree