112
CHAPTER OUTLINE
■ ON-SITE VERSUS LABORATORY ANALYSIS
■ INTERPRETATION OF TEST RESULTS
■ ETHICAL ISSUES IN CLINICAL SETTINGS
Drug testing—that is, use of an objective laboratory test for recent use of specific drugs—is useful in deterring and detecting drug use in many settings, including physicians’ offices, the workplace, schools, athletic programs, and the criminal justice system. Testing is needed and expected in sports (1).
Drug testing identifies recent use of specific drugs, including alcohol and nicotine. It does not identify addiction or dependence. Through blood and breath—but not urine— alcohol concentrations roughly correlate with the degree of impairment, while tests for drugs and drug metabolites in urine generally do not. Results of drug tests thus are interpreted as evidence of recent use of specific drugs, rather than as evidence of drug dependence or impairment. The identification of recent drug use has great value because patients’ denial of alcohol and drug use is a cardinal feature of substance use disorders.
Drug testing has many uses in clinical and forensic medicine even though testing has not been included in the curriculum and practical experience of most physicians. As with other recently introduced tests in medicine (e.g., functional magnetic resonance imaging or HIV testing), physician education and expert guidelines are needed to make use of new technologies that have the potential to greatly enhance medical care. Whereas the technology of testing is evolving rapidly, physicians’ use of testing remains in an early stage of development. In fact, some professional organizations have called on experts, to produce guidelines for the use of testing (2). In 2013, the American Society of Addiction Medicine (ASAM) released a White Paper promoting the use of drug testing “as a primary prevention, diagnostic and monitoring tool” (3, p. 1).
Physicians working within larger medical care settings, including drug treatment and hospital and outpatient clinics, often have clinical drug testing available to them. Physicians in office-based practices can collect samples of urine, hair, or oral fluids as they, or their staff, collect other samples for submission to their routine clinical laboratory, virtually all of whom do drug tests. Physicians can also purchase on-site drug testing kits from their usual providers of medical supplies.
This chapter is a practical overview of the use of drug testing in clinical practice, with a focus on improving the application of this technology to improve substance use prevention efforts, as well as the identification, treatment, and long-term management of individuals with substance use disorders.
EVOLUTION OF DRUG TESTING
Fifty years ago, drug testing was an uncommon, expensive, and laborious component of death investigations, but even then, drug testing was commonly employed in emergency departments when a drug overdose was suspected. During the 1970s, the use of drug testing spread rapidly into substance abuse treatment programs and the criminal justice system. In the 1980s, successful use of drug testing in the military led to dramatic reductions in drug use (4) and inspired subsequent use of drug testing in the workplace. Over the past decade, drug testing has been used in drug prevention programs, including within school systems, in highway law enforcement, and in athletic competition.
Over the past five decades, the technology utilized for drug testing has progressed rapidly, permitting the identification of drugs and their metabolites at far lower concentrations, far more economically. These analytical enhancements are related to the development of benchtop mass spectrometry. At the same time, drug testing expanded to include testing of oral fluid (saliva), hair, and sweat. Because drugs also are present in breath, the future holds the promise of breath testing for drugs of abuse (5). The leading issue many years ago—the problem of false positives—has been virtually eliminated (6).
Drug tests now are available over the counter for home use. When drug testing is conducted by families, it is useful for them to be educated about what testing does and does not do and how to handle positive tests most effectively and wisely (7). When drug testing migrated from clinical settings to prevention in the workplace, controversy ensued over the application of modern drug testing technology and the use of forensic standards became commonplace for the first time in toxicology. Drug testing also is used in research and evaluation studies to validate self-reports in surveys of drug use and to evaluate the effectiveness of treatment programs in reducing patients’ drug use (8,9).
Drug testing has expanded in recent years to include pain management clinics and other settings where potent opioids and other medications are prescribed on a regularly basis. Drug test profiles are extensive and include many opioids and benzodiazepines, as well as illicit drugs (including amphetamines, cannabinoids—metabolites of cannabis— and cocaine). These analyses are used to monitor patient adherence to prescribed medications and to identify the potential use and abuse of other, nonprescribed substances.
THE SCIENCE OF DRUG TESTING
Although drugs of abuse, including alcohol, are used primarily for their effects on the brain reward centers and are ingested through many routes of administration (e.g., oral, intranasal, smoking, and intravenous), they are distributed by the blood to all areas of the body. For this reason, drugs and their metabolites can be detected in nearly all body fluids and tissues.
In general, drugs and drug metabolites are detectible in urine for 1 to 3 days after acute administration, although after heavy chronic use, some drugs—especially cannabis— may be detected for longer periods of time. After a single episode of cannabis use, many users have negative urine tests at usual cannabinoid cutoffs within 24 hours, and almost all will be negative within 3 to 5 days of last use. However, with chronic use of cannabis, positive urine tests can be obtained for a month or longer.
The immunoassay screening test makes use of the remarkable specificity and sensitivity of the antigen–antibody reaction. Manufacturers of early drug tests used bacteria to produce patented antibodies that were highly specific for the tested drugs and drug metabolites. In the early years of drug testing, there was some unwanted cross-reactivity to a few of the antibodies being used. Today, with improved antibody specificity, this virtually never occurs. The on-site tests described later in this chapter rely on antibodies to detect low concentrations of drugs and their metabolites in urine and oral fluid.
In standard drug testing, an initial immunoassay screening test is followed by a more sensitive and specific confirmation test that is based on mass spectrometry. The confirmation of drugs and drug metabolites by gas chromatography–mass spectrometry (GC-MS) is now compulsory in many settings, especially when there are serious consequences for a positive test. However, in many clinical settings (such as emergency departments, drug treatment programs, and the criminal justice system), only the initial immunoassay test is required, thereby reducing the cost of testing and increasing the speed with which results are available.
The GC-MS identifies drugs and drug metabolites primarily on the basis of the chemical structure of the compound. It is an accurate method of detecting drugs and drug metabolites; the false-positive rate of GC-MS is nil. The current highest standard is liquid chromatography–mass spectrometry–mass spectrometry (LC-MS), which is a sophisticated technology that is increasingly being used, particularly in the field of pain management.
When there are controversies surrounding or severe consequences attached to a single drug test result, not only is the two-step analytical testing process desirable but the ultimate fail-safe is to retain the positive sample in the original collection container in a frozen state for potential retesting. Such repeat testing is easily done with urine testing. It is the ultimate rebuttal to those who say no drug testing process is completely foolproof.
A frequently asked question is, “How accurate is the drug test?” When the two-step process (including the immunoassay screen and the mass spectrometry confirmation) is employed, the drug identification process is highly accurate. If a specific drug is identified on a drug test of a specimen from a donor, then that drug (or a drug metabolite) was present in the donor’s body. An evaluation by a medical review officer (MRO) usually can determine whether the drug was in the donor’s body as a result of a drug prescribed by a physician. While the highest level of science, including the two-step process, the MRO validation, and the retained positive specimen are desirable in certain cases, such as when there are potential legal challenges, even an immunoassay screen alone is highly reliable for many medical purposes, such as the identification of specific drugs, even though it does not rise to the highest (or forensic) degree of certainty.
ON-SITE VERSUS LABORATORY ANALYSIS
Most drug tests are conducted at clinical laboratories following the collection of a sample at some other site (e.g., at a drug treatment center or a physician’s office). The laboratory-testing process usually requires a day or two from the time of collection until the result is available to the clinician. In recent years, more drug testing is done on-site when the initial immunoassay test is done at the point of collection rather than at a laboratory. In forensic settings, the sample that tests positive on-site is sent to a laboratory for a confirming test before being reported as positive. In many clinical settings, such confirmation may be unnecessary, especially if the donor admits to recent drug use.
The ability to obtain results at the time of collection is enormously useful. However, on-site tests, especially oral fluid tests, may be less sensitive than laboratory-based analyses. In addition, a confirmation test is not available on-site. On-site tests seldom produce false-positive results, although that does happen. False-negative results are more common when using on-site test kits, and this problem mitigates some of the benefits of immediate results. It is possible to define the extent of the problem of false-negative test results with any on-site device by splitting some samples and sending one sample for laboratory-based testing or, in the case of oral fluid testing, by comparing the oral fluid on-site test results with the results of urine samples taken from the same donor at the same time and then analyzed at a laboratory.
CHOICE OF MATRIX
The choice of a testing matrix relates to the period of time after drug use that the drugs and their metabolites are detectable, the distribution of the drugs and drug metabolites, the ease of specimen collection, and the level of vulnerability to cheating.
Urine is a particularly attractive matrix for drug testing because it is easy to collect (compared to blood), most drugs and drug metabolites can be readily detected in urine without complex extraction processes, and drugs and their metabolites often can be detected for longer periods of time in urine than in blood and oral fluid. Nevertheless, testing for drugs of abuse in oral fluid, hair, and sweat is valuable. For that reason, it is important that physicians who use drug tests understand the potential benefits of testing samples other than urine.
Urine
Drug testing outside of the medical examiner’s office and the emergency department began with urine. There are many reasons to recommend urine as a matrix for drug testing, including the fact that virtually all clinical laboratories perform drug tests on urine samples, creating a highly competitive marketplace whose effect is to lower costs and enhance the choice of drug test suppliers.
When urine drug testing first became widespread in drug abuse treatment and the criminal justice system in the 1970s, the standard was to directly observe the collection— that is, to directly observe the urine leaving the donor and entering the collection cup. However, when drug testing came to the workplace in the 1980s, direct observation was considered objectionably intrusive. To accommodate this objection, unobserved urine collection became common practice. That change opened the door for cheating. Donors developed a remarkable range of strategies to cheat on drug tests, which led to one of the more active areas on the Internet and to the publication in 1987 by Abbie Hoffman of a book entitled Steal This Urine Test (10). Thus, began a cat-and-mouse game that continues to the present day, when the Internet provides ready access to information on the latest cheating strategies (11,12). Cheating thus is the Achilles heel of urine as an attractive testing matrix. When cheating is suspected, it is useful to use another matrix and/or to engage in direct observation of the specimen collection.
The determinants of the concentration of drug and drug metabolites found in urine after a single use of a drug are complex. They include the dose of the drug taken and the duration of time between the last drug use and collection of the urine sample. Also important is how the drug was ingested and how much of it was ingested over what period of time in the days prior to collection of the sample. A further variable in urine drug concentrations is the amount of fluid recently ingested because whatever the kidneys excrete of the drug and/or its metabolites is diluted by the fluid excreted between the time of the most recent voiding and the time of collection. By special order, creatinine determinations can be used to normalize drug concentrations, thus removing the dilution problem (13).
Because urine testing is dominant in the drug testing marketplace, it is relatively easy and inexpensive to add drugs to the federal government’s basic five-drug panel, which consists of cannabis, cocaine, phencyclidine (PCP), amphetamines, and opiates. This is a major advantage of urine testing, as a large proportion of drug use involves drugs other than those in the basic panel (14). Widely referred to as the “DHHS-5” because the Department of Health and Human Services (DHHS) manages the federal standards for regulated drug testing, in 2010 confirmatory testing of the panel was expanded by DHHS to include the following amphetamines:methylenedioxymethamphetamine, methylenedioxyamphetamine, and methylenedioxyethylamphetamine. Urine drug test suppliers offer more extensive panels of commonly used drugs and can add additional drugs when needed, usually at substantially higher prices.
Depending on whether confirming tests and MRO validation are required, as well as the volume of tests and the number of drugs in the panel, urine drug tests typically cost $15 to $40. Both on-site and laboratory-based urine tests are widely available.
Hair
Drugs and drug metabolites are incorporated in the hair while it is formed in the hair follicle. Head hair grows approximately 1/2 inch a month. The typical hair specimen is 1.5 inch long, thus producing a record of drug use over the preceding 90 days. However, it takes about 1 week for hair to grow from the base of the follicle to a point at which it can be snipped at the level of the scalp; there is no record in hair of drug use during the week prior to sample collection. Alcohol is not incorporated in hair, although alcohol’s major metabolites, including ethyl glucuronide (EtG), are detectable in hair samples (15).
Over the course of the 90 days covered by a typical 1.5-inch hair sample, even a few uses of most drugs of abuse are detectable. Cannabis is an exception because concentrations of tetrahydrocannabinol (THC) and cannabinoids in the body—including the hair—are significantly lower than the concentrations of most other drugs of abuse. For this reason, cannabis must be used about twice a week for the entire 90 days to produce a positive result at the standard cutoff concentrations. Hair tests are very resistant to cheating because hair collection is always under direct observation.
A problem with urine testing is that recent consumption of poppy seeds can produce a test result that is falsely positive for morphine or a codeine positive test result that is difficult to distinguish from heroin use. This makes the urine test virtually useless in identifying heroin use in contested nonclinical settings. Hair samples are not positive for morphine and/or codeine even after repeated consumption of poppy seeds, which makes hair testing an attractive option when urine tests produce positive morphine and/ or codeine results. Hair testing also is an attractive option when cheating on a urine drug test is suspected.
Because hair testing gives results that cover the period from seven to 90 days prior to collection, while urine tests provide results that cover 1 to 3 days prior to collection, these two matrices do not cover the same time periods. When the issue is drug use in the preceding 7 days, hair testing has no value. However, when the question relates to use of specific drugs of abuse, the question of when the drug use occurred is not particularly relevant.
Hair testing has two additional features of clinical importance. The first is that the concentration in the hair is a rough measure of the intensity of use over the 90 days covered by the typical sample. Thus, at intake into treatment, if it is useful to objectively assess the intensity of use of specific drugs during the preceding 3 months, a hair sample allows a distinction between heavy, moderate, and light use of specific drugs over that time period. Second, a 1.5-inch hair sample can be tested separately for each half inch, thus permitting a separate assessment of drug use in each of the past 3 months. This test, called segmental analysis, is sometimes useful in forensic settings.
Although the same drugs that are identified in urine tests can be identified in hair tests, because hair testing is used less commonly, the laboratories that conduct hair tests are likely to offer only a fairly narrow panel of drugs, often the DHHS-5.
Hair testing has been criticized as racially biased because of an early study finding that when a mouse was given an antipsychotic drug, higher concentrations of the drug were found in the black hair on that mouse than in the white hair. However, it is important to recognize that the claim that hair testing is color biased does not relate to an assertion that black hair or one ethnic or racial group is can be found positive on hair testing without using the drug identified. Rather, the claim is that after drug use, the hair test is more likely to be positive with one hair color than another. The appropriate response to these claims is that, in drug testing, there usually is no attempt to normalize the test results for various biologic factors. Instead, the tests are read to a particular concentration in the tested sample. For example, alcohol tests on the highway use the blood alcohol concentration (BAC) of 0.08 as the cutoff for violations for both men and women, even though a woman typically can reach that concentration at a lower level of alcohol consumption than would a man.
Further, several studies using large samples of tested subjects unanimously found that the proportion of subjects who tested positive are the same for African Americans and whites, based on urine testing, hair testing, and self-report (16–18).
There are no on-site hair tests at this time, although they may become available in the future. Thus, only laboratory-based hair tests are available, from a small number of commercial laboratories. Hair tests typically cost about $40 to $80 per test.
Oral Fluid
The liquid content of the oral cavity (e.g., saliva or oral fluid) can be analyzed for drugs of abuse with both on-site and laboratory-based techniques. Oral fluid testing is highly resistant to cheating, as the oral fluid sample is collected under direct observation. The most significant problem with oral fluid testing is that, like hair testing, the tests are relatively insensitive to cannabis use. While the detection of other drugs of abuse is roughly similar for oral fluid testing and urine testing, significantly fewer recent users of cannabis are detected using oral fluid.
The on-site kits for oral fluid testing are particularly prone to miss cannabis use because they are generally less sensitive than laboratory-based analyses. With both hair testing and oral fluid testing, this sensitivity problem is the result of the lower level of THC and metabolites present compared to the level of other drugs of abuse. As the tests are refined to have greater sensitivity, this limitation of both hair and oral fluid testing can be expected to vanish.
In general, oral fluids are most closely correlated with blood testing, with which saliva is in equilibrium. This means that oral fluid testing generally identifies drug use within the 12 to 24 hours prior to sample collection.
Because oral fluid testing is much less common than urine testing, the panel of drugs identified is usually limited to the DHHS-5 in on-site kits. Even though other drugs and their metabolites are present in oral fluids, as a practical matter, it is not yet possible to identify other drugs with oral fluid using on-site test kits. However, laboratory-based testing of oral fluids can detect other drugs of abuse.
For many applications, oral fluid testing is widely expected to be the test of the future because it does not pose the problems with direct observation of sample collection that occurs with urine and because it is resistant to cheating. On the other hand, the current sensitivity limits of oral fluid testing leave much to be desired. The expectation is that in the future, as the technology improves, oral fluid will deliver on its great promise. An oral fluid test typically costs about $20 to $60.
Sweat
Because drugs of abuse are contained not only in saliva but in sweat, sweat is an attractive matrix for drug testing. A patch that is similar to a nicotine patch worn in smoking cessation is applied to the tested person. The patch is removed after a week or two for analysis at a laboratory. The sweat is collected in an absorbent pad that is protected by a permeable cover. The water in sweat evaporates through the covering membrane, leaving the drug and drug metabolites concentrated in the gauze.
Sweat allows prospective testing from the time the patch is applied, whereas all other drug tests are retrospective from the time of collection. There is no on-site option for the analysis of drugs and drug metabolites in sweat. Sweat testing is resistant to cheating because the patch puckers when removed and reapplied. A sweat patch test typically costs about $35.
Breath
Alcohol is commonly quantified in breath, with the results widely used in clinical and medicolegal settings. In addition, recent studies have demonstrated the presence of amphetamines, THC, and methadone in breath (19–21). Breath testing has become an important tool to detect impaired driving (22). As the test technology improves, including the development of a better collection device, it is likely that drugs of abuse will be detected in breath as they now are for alcohol.
Breath testing for drugs of abuse is likely to become practical well after oral fluid testing is practical, as both depend on improving technology. Moreover, the level of drugs present in oral fluids, while lower than in urine, is far higher than in breath. Nevertheless, the ultimate in drug testing is likely to be achieved with breath testing because it is resistant to cheating and far easier to collect than urine, oral fluids, or hair.
Testing for Alcohol
Since the dose of alcohol needed to produce brain reward is a thousand or more times higher than the dose of the commonly used drugs of abuse, testing for drugs has been more challenging and more reliant on the evolution of technology than it has been for alcohol.
Alcohol is rapidly metabolized, primarily by the liver, so alcohol levels in the blood decrease rapidly—typically to zero within a few hours after the last drink. The acute impairing effects of alcohol are related to the blood alcohol levels as modified by the moderating effects of tolerance and the subject’s familiarity with the task being measured. The alcohol concentration is in equilibrium with the blood at the time the urine leaves the kidneys. The urine in the bladder is a reflection of the blood alcohol levels over the period of time that the urine in the bladder was being produced by the kidneys. For this reason, the urine alcohol level lags the blood level at the time of urination, meaning that the urine alcohol level is lower than the blood alcohol level at the time of urine collection during the ascending slope of the blood level and higher during the descending slope of blood level after drinking stops. The detection window for urine alcohol tests generally is 12 hours or less after drinking has stopped, in contrast to 1 to 3 days for detection of most drugs of abuse.
The concentration of alcohol in the urine is of limited value in settings such as highway safety when the BAC standard is typically 0.08. However, in settings in which there is a zero tolerance policy for alcohol use—such as for underage youth, persons in drug and alcohol treatment, and those facing legal sanctions for any drinking (as may occur in probation or child custody settings)—urine testing for alcohol can be helpful. Urine testing for alcohol is especially practical when drug tests are being conducted on a urine sample, at which time it is easy to add an alcohol test.
An important new testing option is the test for EtG or ethyl sulfate (EtS), both of which are metabolites of alcohol that are found in urine for 5 to 7 days following the consumption of alcohol. These tests are especially useful in settings where alcohol use is completely prohibited (e.g., in persons undergoing drug or alcohol treatment and others under supervision that includes a requirement not to use alcohol). A negative EtG test is especially valuable in establishing that the donor of the urine sample has not used alcohol in the preceding 5 to 7 days. As most EtG tests are negative, this is valuable information in many settings in which abstinence from drinking is required.
Because the EtG tests may be positive when the donor has used an alcohol hand sanitizer or an alcohol-containing mouthwash, interpreting a positive EtG test result requires clinical judgment, especially if the consequences for a single positive test are severe. Individuals who are subject to EtG testing for alcohol should be warned specifically and in detail to avoid alcohol-containing products—which are ubiquitous—or risk a positive test result (13).
Comparing Matrices
Refer to Table 112-1 for a comparison of the clinically available test matrices. There are clinical settings in which each of the four matrices discussed in this chapter is particularly useful. Urine is the default matrix for most drug tests because it is the most familiar and because most clinical laboratories conduct these tests. Urine also is the most practical matrix when special-order tests are required, including tests for drugs that are less commonly used. On the other hand, urine has a much shorter detection window than does hair. In addition, urine is the matrix most vulnerable to cheating. Oral fluids are the most easily obtained matrix but can be less sensitive to drug use and have a shorter detection window than urine. Sweat patch testing is prospective—meaning it identifies drug use after the patch is in place. Like oral fluids and hair testing, sweat patch testing is highly resistant to cheating. Hair testing is particularly helpful in scheduled testing, including pre-employment tests where cheating is common. On the other hand, hair is the most expensive drug test matrix.
Table 112-1 Comparison of Blood, Urine, Hair, Saliva, and Sweat Patch Testing for Drugs of Abuse
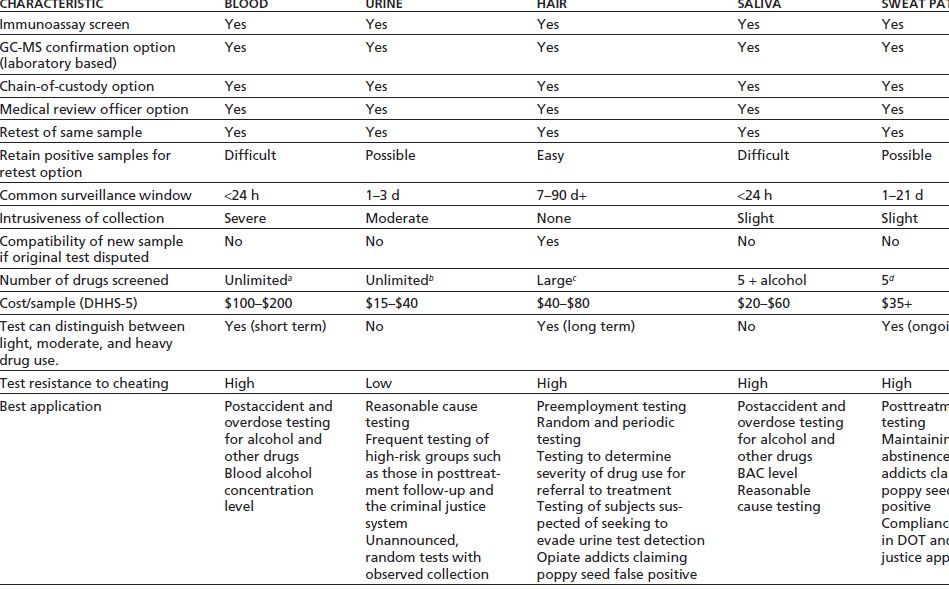
(Note that costs vary dramatically based on prices negotiated with laboratories and fees related to collection, administration, and reporting.)
aBlood testing for alcohol is routine, costing about $25/sample, but blood testing for drugs is done by only a few laboratories in the United States. Blood testing for drugs is relatively expensive, costing about $60 for each drug tested for.
bUrine tests for nonroutine drugs are available from most reference laboratories, and costs for broad screens are generally <$200.
cHair testing is commonly performed for the NIDA 5 (cocaine, opiates, marijuana, amphetamines, and phencyclidine). However, a large number of drugs and metabolites can be detected, and routine broad testing is performed in several toxicology reference laboratories. The cost of nonroutine testing of hair is <$500 in most cases.
dCommonly limited to the NIDA 5. Tests can also be performed for alcohol.
DOT, U.S. Department of Transportation; GC-MS, gas chromatography–mass spectrometry; NIDA, National Institute on Drug Abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


