16
CHAPTER OUTLINE
DEFINITION
There is good consensus on what constitutes inhalant abuse. Typically, abused inhalants are breathable chemicals that can be self-administered as gases or vapors. The products can be gases, liquids, aerosols or, in some cases, solids, but products that begin as liquids or solids are vaporized and inhaled. There are historical examples of liquids that are both inhaled and consumed orally (e.g., ether), but the overwhelming majority of abused inhalants, by definition, are inhaled. Drugs such as crack cocaine, which is aerosolized, and cannabis, which is smoked, are consumed by inhalation but are not generally, or usefully, classified as inhalants.
DRUGS IN THE CLASS
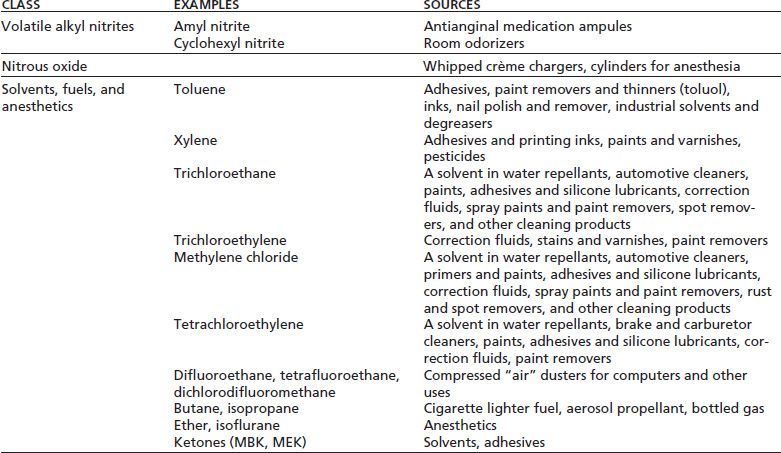
With other drugs of abuse, it has proved most useful for addiction medicine to classify the substances primarily on the basis of shared pharmacologic and behavioral effects rather than by structure, source, or form. It would be desirable if the same could be done for inhalants (1). The problem is that there is no sufficient knowledge of the effects of inhalants to make very fine distinctions among them. In addition, the toxicologic effects of these compounds differ, and these differences do not necessarily follow classifications based on acute abuse-related pharmacologic and behavioral effects. Nonetheless, three subdivisions of abused inhalants are useful, as shown in Table 16-1. The rationale for this subclassification has been presented elsewhere (2) and is summarized below.
TABLE 16-1 PHARMACOLOGIC CLASSIFICATION OF ABUSED INHALANTS
Volatile Alkyl Nitrites
The prototypic alkyl nitrite is amyl nitrite, used medically as a vasodilator for treatment of angina. Amyl nitrite is available as a volatile liquid in ampules that are broken open and the vapor inhaled. At one time, the ampules were available over the counter and abusers would “pop” them open—hence the street name “poppers.” When amyl nitrite was brought under prescription control by the U.S. Food and Drug Administration (FDA), retailers made room odorizer products from other alkyl nitrites with names such as “Locker Room” (nitrites smell like a locker room), “Rush,” “Hardware,” and “Climax.” The latter connote their use in the context of sexual activity. As of this writing, cyclohexyl nitrite appears to be the most easily obtained volatile nitrite. Very little is known about the safety of these products.
Relatively little research has been done to determine the mechanisms of action for the abuse-related effects of volatile nitrites. It is clear from animal studies that they do not produce acute intoxications similar to those of abused solvents such as toluene and trichloroethane. It seems likely that they are abused because of their ability to produce syncope secondary to venous pooling in the periphery and because of their effects on tumescence and smooth muscles, making them popular as aids to sexual activity. The attractiveness of syncope as a drug effect might be questioned until one recalls that even children like to hold their breath or twirl around until dizzy. It also may be that during dancing, for example, the pounding in the head one might experience from anoxia could enhance a user’s appreciation of the situation. More research is needed on this point.
Nitrous Oxide
Nitrous oxide is somewhat distinct in that it is a gas at room temperature and pressure. It is popular to divert anesthetic nitrous oxide for illegitimate use. The tanks can be used to fill balloons for ready sale at concerts, “raves,” or parties. The acute pharmacologic and behavioral effects of subanesthetic concentrations of nitrous oxide are poorly understood. Certainly, it can produce euphoria (“laughing gas”) and feelings of intoxication (3,4), but the qualitative nature of this intoxication appears to be different from that produced by anesthetic vapors such as isoflurane and sevoflurane or by other drugs of abuse (3,5). It should be remembered that nitrous oxide is very impotent as an anesthetic, requiring concentrations of about 15% to 20% to produce intoxication. In fact, many users breathe almost 100% nitrous oxide (e.g., from a balloon). This action, of course, can lead to some anoxia and, as with nitrite-produced syncope, has acute psychological effects as well.
Another interesting aspect to nitrous oxide pharmacology is that, unlike vaporous anesthetics, it can produce good analgesia, as seen in animal models, and there is some evidence for opiate receptor involvement in the analgesic effects (6), although opiate antagonists do not appear to reverse either anesthesia or subanesthetic intoxication with nitrous oxide (3). GABAergic effects may be responsible for the anesthetic and other depressant effects of nitrous oxide (6).
Volatile Solvents, Fuels, and Anesthetics
This category includes a large collection of chemicals that further research probably will reveal to have different profiles of acute effects as well, but the state of the science is insufficient at this point to propose a further subclassification. Among the prototypic chemicals for this class are 1,1,1- trichloroethane (TCE) and other halogenated hydrocarbons; toluene and other alkyl benzenes; butane and other alkanes; and various ketones, alcohols, and ethers (see Table 16-1). It has been hypothesized that many of these commercial chemicals share profiles of acute effects with subanesthetic concentrations of volatile anesthetics such as halothane, sevoflurane, and isoflurane (7,8). These anesthetics offer a safer alternative to the study of toluene and similar chemicals in humans, and they have been directly compared in many animal studies (8,9). As a point of comparison, it is useful to recall that beverage alcohol (ethanol) also is a solvent and produces a type of anesthesia at very high blood levels. Ethanol actually is much less potent than the other solvents for acute central nervous system (CNS) effects, discouraging use by inhalation. Alcohol shares pharmacologic and behavioral effects with depressant drugs such as the barbiturates, nonbarbiturate sedatives, and benzodiazepines, and perhaps abuse of these solvents and anesthetics could be viewed clinically as special instances of abuse of depressant drugs (7). To be sure, the acute depressant-like intoxication and presentation of overdose can be the same among all these compounds.
ABUSE OF INHALANTS
History
The abuse of inhalants has a long history. Perhaps the best known instances are the use of anesthetics for purposes of intoxication that began with their discovery more than 200 years ago. The euphoriant effects of nitrous oxide were noted by Sir Humphry Davy, who synthesized the substance in 1798 and began calling it “laughing gas.” Laughing gas subsequently was used as part of comedic traveling shows at the beginning of the 19th century. The early vapor anesthetics, including ether and chloroform, were used recreationally and as “nerve tonics,” both by inhalation and drinking. It may seem odd to drink an anesthetic, but one must remember that alcohol is a highly volatile liquid with irritant properties, yet its oral consumption surprises no one.
Today, abused inhalants differ widely in their availability. Some, such as nitrous oxide and amyl nitrite, are under control of the FDA as prescription medications, although forms of nitrous oxide are available commercially (e.g., as aerosol propellants). Commercial sales of volatile alkyl nitrites are regulated in the United States by the Consumer Product Safety Commission, a step that has greatly reduced the availability and abuse of most of these substances. However, many are still advertised for sale on Internet sites. Many other types of abused inhalants can be found in homes or workplaces or are readily purchased at retail establishments. Gasoline, a very complex mixture of volatile compounds, is available everywhere, and butane lighter fluid is not very difficult to obtain. There have been discussions of strategies to prevent access to abused inhalants, to change their labeling, or to reformulate products to limit their abuse potential. Each of these strategies needs to be viewed on a case-by-case basis to be certain that it will achieve the desired effect and not result in abusers seeking potentially more toxic products that almost certainly cannot be restricted (e.g., gasoline). Harwood (10) has undertaken a policy analysis of the inhalant abuse problem in the United States, including the roles of treatment and prevention.
Epidemiology
More than 22 million Americans aged 12 or over have used inhalants, and every year, about 750,000 use them for the first time (11). Results of national surveys suggest that the prevalence of inhalant use is greatest among 12- to 17-year-olds compared to other age groups. For example, the school-based Monitoring the Future national survey in the United States of 8th, 10th, and 12th graders (12) estimated that inhalant use in 2012 was somewhat less than its peak in the mid-1990s, yet it still remains high (Fig. 16-1). One important difference from other drugs of abuse is that the prevalence of inhalant use actually decreases from 8th to 12th grade. Except for alcohol and tobacco, the prevalence of inhalant use among youth is second only to marijuana in this age range. The 2010 U.S. National Survey on Drug Use and Health estimated lifetime, past-year, and past-month prevalence for marijuana, inhalants, and cocaine use in the United States (13). About 1 in 10 youths used inhalants sometime in their life, and 3.6% used them in the past year (Fig. 16-2). Among older youths and adults, the prevalence of inhalant use falls considerably below that of marijuana, cocaine, and heroin, but current users remain a significant minority of substance abusers. Use of inhalants in the United States is common among both sexes but disproportionately involves non-Hispanic white youths compared with other age and ethnic groups (15). It is particularly prevalent among juvenile justice-involved youth (14). Although many inhalant users quit as they reach young adulthood, it is incorrect to characterize this problem as a passing fad in youth. For about half of current users, duration of use exceeds 1 to 2 years, with about 10% using inhalants for 6 years or more (15). Abuse of inhalants is an even more significant problem in other parts of the world, particularly in the developing countries (16).
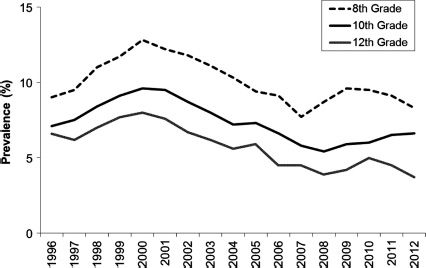
FIGURE 16-1 Trends in the annual prevalence of the use of inhalants for 8th, 10th, and 12th graders in the United States. Shown is estimated use in the past year during each of the reporting years from 1996 to 2012. (Based on data from Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the future national results on adolescent drug use: overview of key findings 2012. Ann Arbor, MI: Institute for Social Research, University of Michigan, 2012.)
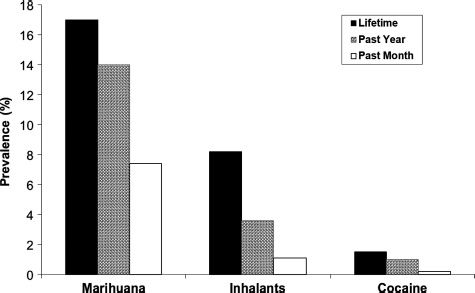
FIGURE 16-2 Lifetime, past-year, and past-month prevalence estimates for marijuana, inhalant, and cocaine use in 2010 in youths aged 12 to 17 in the United States. (Based on data from the National Household Survey on Drug Use and Health [Substance Abuse and Mental Health Services Administration, 2010].)
Inhalant users often develop substance use disorders. In one study (17), 8% of past-year inhalant users 18 years and older met DSM criteria for inhalant abuse or dependence within that period. Inhalant use is also associated with other substance use disorders and may be an even stronger predictor of subsequent drug abuse problems than marijuana use. Several studies have shown a clear progression from early inhalant use to later use of drugs such as cocaine and heroin. In one such study, researchers found that youth who had used inhalants by age 16 had more than a nine-fold greater likelihood of using heroin by age 32 than did youth who had not used inhalants, even when controlling for other risk factors associated with inhalant abuse (18). In another study, a history of inhalant use independently increased the odds of becoming an injection drug user by more than fivefold (19). In the latter study, the magnitude of the increased risk associated with inhalant use exceeded that for marijuana use. There is also evidence that users of both inhalants and marijuana are at especially greater risk. For example, among adolescents who had used both (20), 35 % had a 1-year prevalence of alcohol abuse or dependence, and 39% had a drug abuse disorder.
ABSORPTION AND METABOLISM
The abused inhalants include compounds that are self- administered as gases, vapors, and aerosols. These three forms of inhalants have somewhat different absorption characteristics and require different methods of use (e.g., balloons for gases and bags or rags for volatile liquids). In the case of abused aerosol products such as spray paint, the likely “active ingredient” for abusers is the propellant (e.g., butane) that exists in the aerosol can under pressure; however, the other materials in the cans (e.g., pigments) also can be absorbed.
A useful way to think about the bioavailability of abused inhalants is to apply knowledge of inhalation anesthesia. Gases and vapors rapidly penetrate deep into the lung and, because of their high lipophilicity, are rapidly absorbed and distributed into arterial blood. What distinguishes inhalant abuse from anesthetic use is that the partial pressure of the inhalant vapor inhaled generally is very high and quite variable over time, as users intermittently sniff from balloons or from rags or bags saturated with liquid. With these high concentrations in the inspired air, effects on the brain are almost immediate. As with anesthetics, key factors that would be expected to affect brain concentrations of inhalants are concentration in the inspired air, pulmonary ventilation rate, pulmonary blood flow, and the amount of body fat; however, the practical significance of these variables outside of a well-controlled anesthesia situation is uncertain. Because physical activity increases cardiac output, it is likely that inhalant distribution to the brain in someone who is active will be markedly greater than in someone at rest. Inhalants easily cross the placenta and expose the fetus, with consequences that will be discussed later.
The situation with aerosols is somewhat different. Aerosol propellants typically are gases or vapors. Some of the constituents of aerosol products actually are droplets (i.e., aerosols) when inhaled, and, for these, the rapidity and efficiency of absorption are determined by particle size (median aerodynamic diameter). Both the propellant and the aerosolized content may have behavioral effects. For all practical purposes, even aerosols have an almost immediate onset of action. Thus, it is common for inhalant users to breathe the gas or vapor and instantly stumble or fall down, posing a risk to themselves and others.
It is likely that, for many use situations with inhalants, the concentrations in inspired air exceed concentrations that would be lethal if the user were to be exposed continuously. Lethal concentrations could occur, for example, if a user became unconscious while still exposed to the inhalant. This situation is probably the most common form of acute overdose. It happens when someone using a rag or a bag laden with solvent falls in such a way as to maintain contact with the solvent. Also, some users have devised methods for exposing themselves to inhalants without having to use their hands, such as for use in sexual situations, and become vulnerable to overdose while using the devices.
Elimination of inhalants is very rapid once the source is removed from the inspired air. For most of these chemicals, expired air is the major route of elimination. Those that are relatively insoluble in blood and brain (e.g., TCE) are eliminated more quickly than those with greater solubility in these reservoirs (e.g., toluene).
Most abused inhalants are metabolized to some extent, but this metabolism probably plays a greater role in determining their hepatic toxicity than their CNS effects. Another important factor affecting recovery is the duration of the use episode. Someone who has been inhaling for a few hours might achieve considerable accumulation in muscle, skin, and fat. For obese individuals, recovery can be a bit more prolonged, as the chemicals are more slowly relocated.
Intoxication with inhalants is of shorter duration than with other drugs of abuse, with the result that many health care providers, as well as friends and family of users, rarely see an inhalant abuser who is grossly intoxicated. Unless comatose, such users typically are not brought to emergency departments because they will have recovered before they get there. Law enforcement personnel occasionally encounter intoxicated users if they come upon them during a use episode, but there is little they can do, even in cases of driving under the influence, because of the rapid recovery time. Perhaps, it is this lack of direct experience with intoxicated inhalant users and the difficulty of obtaining confirming clinical chemistry that have contributed to an underappreciation of the adverse public health effects of this form of substance abuse.
MECHANISMS OF ACTION
The neuropharmacologic mechanisms by which inhalant intoxication occurs are poorly understood. Once inhaled, solvents rapidly enter the brain and distribute to lipid-containing membranes within the CNS, placing them in proximity to key functional components. Although it is presumed that the inhalants disrupt normal neural function, it is not clear which systems are most affected and the mechanism by which such disruption occurs. Even the question of whether specific receptors are affected by these agents remains unresolved.
Because of the properties that solvents share with alcohol, it is logical to turn to new discoveries about the mechanisms for the abuse-related effects of ethanol for hypotheses about how abused solvents might act in the brain. Currently, evidence is accumulating that ethanol and solvents can have effects at certain ligand-gated and other ion channel receptors, including those for gamma-aminobutyric acid (GABAA), glutamate, and acetylcholine (8). The best current evidence is that acute solvent intoxication is probably associated with enhancement of GABAA and antagonism at the N-methyl-D-aspartate receptors (21–23). Of particular interest is the discovery that these effects can be very selective for different structural subtypes of these heteromeric proteins, with different chemicals having somewhat different profiles of selectivity. Nevertheless, definitive knowledge about the cellular mechanisms for the abuse of inhalants lags far behind our knowledge of most other classes of abused drugs.
Although scientific evidence would support the view that most of the chemicals in this class of inhalants produces alcohol- and depressant drug-like effects, published descriptions include a much wider array of potential subjective and pharmacologic effects, including hallucinations, tremor, and seizures (24). Certainly, vapors can have excitatory effects in animals (such as flurothyl), and animal studies provide some evidence that even aromatic hydrocarbons like benzene or the isoparaffins can produce a different profile of acute effects than the prototypic depressant solvents such as toluene (25,26). Considering how many commercial products containing very complex mixtures are inhaled, it should not be surprising that users experience a diverse array of acute effects, depending on the product used.
ADDICTION LIABILITY
All of the vapors that have been tested produce clear, reversible, drug-like behavioral effects in animal studies (7). In addition, self-administration studies in rodents (27) and humans (4,5) have shown toluene and nitrous oxide to have reinforcing properties. Toluene also produces a conditioned place preference in rats and mice (28,29). When given repeatedly to animals, many drugs of abuse produce sensitization to their locomotor stimulant effects, a phenomenon thought to reflect engagement of addictive processes in the brain. Trichloroethane has been shown to produce locomotor sensitization in mice (30), and repeated toluene exposure in rats produces cross-sensitization to cocaine and increased cocaine-produced dopamine release (30,31). Indeed, toluene itself has been shown to enhance dopaminergic function in various portions of the brain reward system (32,33), suggesting that there may be a common neural basis for abuse of inhalants and other well-studied drugs of abuse.
Tolerance and Dependence
Little is known about the development of tolerance to and dependence on inhalants, but in general, they do not appear to be prominent features. It may be useful first to describe what has been learned from carefully controlled animal studies of tolerance and dependence, in which exposure conditions are easily manipulated. Under conditions in which many drugs of abuse show considerable tolerance development when given repeatedly, abused inhalants do not readily produce a significant degree of tolerance to their behavioral effects (34). It has also been difficult to demonstrate cross-tolerance with other depressant drugs of abuse. This fact is somewhat surprising because animal models for tolerance to ethanol are readily established. However, with continuous exposure (such as that achieved with mice in inhalation exposure chambers), a mild withdrawal syndrome can be observed with TCE (35); other vapors have not been systematically studied. The withdrawal effects appear within hours after discontinuation of exposure and can be considered excitatory in nature. Ethanol and barbiturates can suppress these withdrawal signs, suggesting a cross-dependence within the depressant class.
Inhalant abuse typically is episodic in nature and thus generally would not occur with sufficient frequency and intensity to maintain a constant exposure throughout a day, much less the weeks or months it might take for physical dependence to develop. Thus, it is not surprising that physical dependence on inhalants is not seen often, if at all, in clinical settings.
On the other hand, several studies find that users report withdrawal signs associated with inhalant use (36,37), but this may not represent a true abstinence syndrome so much as a manifestation of toxicity. There is little evidence of the use of inhalants to avoid a withdrawal syndrome, and a characteristic withdrawal syndrome is not included in the DSM-IV Inhalant Dependence Disorder criteria set; its status in DSM-5 is uncertain at this time. However, regular users of inhalants clearly can develop a pattern of uncontrolled use, marked by a devotion of considerable time and efforts to obtaining and using inhalants that is characteristic of all the substance abuse problems.
Clinical Chemistry
Although few, if any, clinical facilities will routinely conduct tests for the presence of abused inhalants, such tests can be ordered through special services provided by commercial laboratories. Typically, these tests are performed on blood or urine and appear to be available mainly for the abused solvents such as toluene, TCE, and methyl ethyl ketone (MEK). Because inhalants are eliminated so rapidly after acute exposure, such tests would be expected to have a high probability of producing false negatives. Nevertheless, technologic advances can be expected in this area. Problems associated with postmortem detection of abused volatile solvents have also been described (38).
TOXICITY/ADVERSE EFFECTS
It is difficult to summarize what is known and not known about the adverse consequences of inhalant abuse. The discussion that follows focuses almost exclusively on the subclass of inhaled solvents, fuels, and anesthetics. Their toxicity differs depending on which of this broad array of chemicals and chemical mixtures is being abused. The toxicology of commonly used solvents is reviewed in reference texts (39), which can be consulted for specific information on compounds of interest. A brief overview of the information is provided here. Nitrous oxide will be mentioned when appropriate, but the situation with alkyl nitrites is probably very different. The known side effects of organic nitrites used for smooth muscle relaxation would be relevant to abuse of these compounds, but a systematic study of the health consequences in nitrite abusers has not been done. The health effects of nitrite abuse have been reviewed (40).
Acute Effects
Deaths related to the acute effects of inhalants are well documented (41–43). There are two primary sources: behavioral toxicity and overdose. Because the solvent class of inhalants can produce profound intoxication and even anesthetic-like effects at high concentrations, it would not be surprising for accidents and injuries related to behavioral toxicity to occur. Vulnerability to these events probably is enhanced by the rapid onset of intoxication. Additive effects would be expected when these inhalants are used in combination with alcohol or other CNS depressant drugs. Overdose occurs when users lose consciousness while being continually exposed, allowing lethal concentrations to accumulate in the brain. As with anesthetic vapors, the concentration- effect curves for inhalants are very steep, with toxic exposures achieved easily under the poorly regulated exposure conditions of actual use.
It appears that the proximate cause of most overdose deaths is CNS depression, leading to respiratory problems or suffocation. Treatment of overdose rarely occurs in emergency departments because overdose victims usually are either dead or recovered by the time they arrive. In addition to these overdose situations, at least some of the inhalants appear capable of producing acute cardiotoxicity, even in otherwise healthy young users. The mechanism may be increased sensitivity of the myocardium to circulating catecholamines, which may occur when an intoxicated individual engages in some strenuous activity. This phenomenon has been termed “sudden sniffing death” (41) and has been associated particularly with the abuse of aerosols containing chlorofluorocarbon and butane propellants and refrigerants that contain them. The contribution of hypoxia to the acute toxicity of inhalants should be considered, especially with the use of nitrous oxide, in which even 100% concentrations are not lethal except for the loss of oxygen.
Chronic Toxicity
Because of the diverse array of chemicals subject to inhalant abuse, it is difficult to summarize their chronic toxicity. The situation is made even more complicated by the fact that few chronic users confine themselves to a single product or a single chemical agent. Add to this the fact that many abused commercial products are complex mixtures, and it becomes difficult for a toxicologist to ascertain the specific etiology of any adverse health effects seen in inhalant users. Some adverse effects may be secondary to inhalant abuse and reflect lifestyles seen in solvent abusers. These may include such known predictors of poor health as homelessness, inadequate diet, and other substance abuse. Thus, data from case reports in inhalant abusers always should be viewed cautiously. Careful epidemiologic work that controls for key covariants in this population has yet to be done.
In animal studies, it is easier to study individual chemicals, but research in this area typically has been done to simulate the long duration and low-concentration exposures that might be experienced in the home or workplace. Few studies attempt to model the repeated high concentration and intermittent exposure most typical of inhalant abusers. Many chronic inhalant abusers manifest adverse health effects, some of which can be used in diagnosing the problem. Common target organs are the nose and mouth area, lungs, brain, liver, and kidney. There also are physical dangers in using highly inflammable and explosive chemicals.
Neurotoxicity
Many, if not all, abused inhalants can be neurotoxic, and some components of abused products are well-characterized neurotoxicants. Among these are hexane and methyl n-butyl ketone (MBK), which produce axonopathies. The lead in leaded gasoline (still used in many countries throughout the world) produces classic demyelination. Other commonly abused chemicals (such as toluene, TCE, and propane) have less well-described chronic effects on the brain and behavior. Human neural imaging studies and clinical observations suggest that they can produce neurotoxic effects at high exposures, but systematic studies with proper controls are lacking. Most of the information on neurotoxicity of inhalants comes from case reports or small series of patients. It is not known what percentage of abusers have detectable brain damage or whether the inhalants alone were responsible for the observed effects. Brain scanning, neurologic and neuropsychological assessment, or autopsy reports of inhalant abusers show many types of neuropathologies, including loss of white matter, brain atrophy, and damage to specific neural pathways (44–46). Of particular concern are the effects of abused inhalants on the developing nervous system where animal studies have revealed evidence for developmental delays (47,48) and reversible changes in white matter maturation (49), suggesting that the prenatal period through adolescence may be particularly vulnerable periods for inhalant exposures.
Psychiatric Disorders
The association of early inhalant abuse with increased risk of many substance use disorders has been described. For example, Wu and Howard (50) recently reported a very high rate of psychiatric disorders among inhalant abusers in the general US population. For example, 70% of inhalant users in this sample met criteria for at least one lifetime mood, anxiety or personality disorder, and 38% experienced a mood or anxiety disorder in the past year. Females were more likely than males to have multiple comorbid psychiatric illness. Conduct disorder, mood disorders, and suicidality are common among adolescent inhalant abusers (51–53).
Effects on Major Organ Systems
Many chronic solvent users develop irritation of the eyes, nose, and mouth and exhibit rhinitis, nose bleeding, conjunctivitis, and a localized skin rash. When these signs are accompanied by the odor of solvents on the breath or in clothing; by paint, adhesive, or other similar stains on clothing; or by possession of abusable products in unusual circumstances or amounts, inhalant abuse should be considered. With chronic use, inflammation of the lungs can result in coughing and may compromise respiration, and bone mass toxicity has been reported.
The liver is an important target in chronic exposure to many solvents, particularly those that undergo some metabolism. Of particular concern are some of the halogenated hydrocarbons, such as carbon tetrachloride. It could be speculated that persons with other types of liver disease, such as hepatitis or alcoholism, would be particularly vulnerable. Kidney damage also has been reported, in the form of glomerulonephritis and kidney stones. There have been reports of renal tubular acidosis in acute toluene intoxication (54). Benzene and vinyl chloride are known carcinogens. Nitrites and methylene chloride can produce methemoglobinemia.
Fetal Solvent Syndrome
It has been estimated that as many as 12,000 women use inhalants while pregnant in the United States alone. The research on inhalant abuse and pregnancy (47) suggests that decreased fertility and spontaneous abortions in some women may be related to inhalant abuse. Clinical reports of adverse effects in the offspring of solvent abusers include low birth weight, facial and other physical abnormalities, microcephaly, and delayed neurologic and physical maturation. Because certain features seen in these children resemble the fetal alcohol syndrome, a “fetal solvent syndrome” has been proposed. Whether these features result from direct teratologic effects of the abused chemicals or some lifestyle covariants associated with solvent abuse is unknown at this time. Nevertheless, confirmation of adverse effects of prenatal solvent exposure has been obtained in animal studies (47,48). Thus, clinicians should be alert to this possibility in patients who abuse inhalants during pregnancy.
FUTURE RESEARCH DIRECTIONS
Inhalant abuse is one of the least understood substance abuse problems. This is primarily related to the fact that there has been little research in this area (55), generally because of mistaken beliefs about inhalant abuse that even exist within the scientific community. These beliefs include the ideas that (1) inhalant abuse is a transient phenomenon of adolescence that has relatively little associated morbidity and mortality, (2) abused inhalants have “nonspecific effects” on the brain and behavior that do not lend themselves to study with modern technologies in behavioral and molecular neurobiology, (3) laboratory studies of vapors and gases are very difficult to perform, and (4) there are too many chemicals to successfully sort out the similarities and differences in terms of their abuse potential and toxicity.
Our understanding should improve with the increasing information available from animal models (8). However, there are some unique problems inherent in the study of inhalant abuse. The most significant is that it will be difficult to conduct laboratory-based human exposure studies of many of these compounds at behaviorally active concentrations. Such studies have been very important with other drugs of abuse. One approach to overcoming this problem may be to draw lessons about the effects of chemicals of this type by studying the medical use of general anesthetics. This approach has been used successfully by Zacny et al. (3–5). It is particularly useful in studying nitrous oxide. Animal studies of abused inhalants will be especially important because there are fewer limitations on the exposure conditions.
We need a lot more information on the phenomenology and adverse health and social consequences of acute inhalant intoxication, some of which could be obtained from prospective longitudinal studies of inhalant use (56). Epidemiologic studies are made difficult by the numerous types of products and chemicals subject to inhalant abuse and by the fact that subclassifications have differed from study to study. There has been an increased appreciation that alkyl nitrite abuse differs from the rest, and this difference is reflected in separate analyses of prevalence data in many reports. The U.S. National Survey on Drug Use and Health now contains a breakdown of specific subtypes of abused inhalant products, which should be useful for analyses, although it may complicate comparing prevalence figures from one survey to another. Such progress should lead to a better understanding of inhalant abuse and improved treatment and prevention strategies.
Although it seems clear that chronic use of inhalants can cause damage to the brain and other organs, much more information is needed about the patterns of use that produce such effects and whether the chemicals themselves cause the damage or whether inhalant abuse interacts with other factors to produced the observed effects in some users. Considering the very large number of persons who have experimented with inhalants, it seems certain that only a fraction of these experience organ damage. Much more data are needed on the etiologic factors in observed cases of organ toxicity in inhalant abusers, and more general population studies with appropriate control groups are needed to assess the incidence of these effects.
CASE FOR CONSIDERATION
The parents of a 14-year-old boy report that they are concerned about behavioral changes they see taking place. The boy often spends several hours a day after school in the garage, sometimes with friends and sometimes alone. He and his friends have stacked up boxes to sit on, but there are no obvious recreational activities available in the garage. He did not spend as much time with the family, slept more, ate less, and was more argumentative and more irritated. His school performance had deteriorated. Although the boy sometimes returned from the garage slightly intoxicated, a search of the garage and his room revealed no evidence of alcohol or other drug paraphernalia. The boy denied drinking or smoking pot. The mother becomes especially concerned when she noticed that her son had red eyes and sores around his mouth. The parents were advised to bring their son to see the family physician for assessment. They make an appointment, but before the date for the physician visit, they find their son comatose in the garage. He had fallen with his face into a paint rag that had obviously been moistened with the fluid from an open can of paint thinner that was stored in the ground. The garage had a strong chemical smell. They opened the garage door, moved the boy outside, and called 911, but before the emergency response vehicle arrived, the boy recovered consciousness, displaying slurred speech and signs similar to alcohol intoxication. After a discussion with the family physician, the family arranged for their son to see a psychologist experienced in adolescent conduct disorder and substance abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


