17
CHAPTER OUTLINE
Within the addiction field, the term steroids has come to define those compounds that possess anabolic or tissue-building effects, but because most also have some androgenic properties, they are more appropriately called anabolic–androgenic steroids (AAS). This profile of effects distinguishes them from the corticosteroids and the female gonadotrophic hormones; neither of which is subject to abuse. There is a rather long list of AAS that have been produced for both human and veterinary use; the major source of abused steroids is diversion from licit manufacture and distribution, as clandestine laboratory synthesis of these products is rare. The major distinction between use and abuse is that abusers employ supraphysiologic dose compounds to increase muscle growth and performance. It is the consequence of these extremely high doses that results in rather dangerous, often, but not always reversible, organ toxicity.
DRUGS IN THE CLASS
The prototypic hormone, testosterone, is the standard to which all of the synthetic products are compared, and it is one of four structurally distinct groups of AAS. The other three groups are 17α-alkylated derivatives of testosterone, 17β-esterified derivatives of testosterone, and modified ring structure analogues (1). The history of how testosterone and its effects on male sexual development and tissue building were discovered is well detailed by Kochakian (2). Although hormonal involvement in male sexual development was known in 1849, it was not until 1930 when androsterone (a metabolite of testosterone) was isolated from human urine. In the 1940s, after chemists had succeeded in synthesizing testosterone, their efforts were directed toward separating its anabolic from its androgenic effects and to make a formulation that could be taken orally. The androgenic component of these synthetics has never been completely separated from the anabolic effects; only the relative percentage of the two has been manipulated. Commercially prepared products were used briefly during World War II to promote wound healing. In 1939, Boje (3) postulated that AAS might not only increase muscle mass but improve physical performance as well. Hartgens and Kuipers (4) provide a comprehensive review of the pharmacology and toxicity of AAS in athletes.
The introduction of AAS to the United States has been traced to the 1954 World Weightlifting Championships in Vienna, when the Soviet Union’s coach informed the US coach that his team members were taking testosterone (5). In the ensuing years, use of AAS by elite weight lifters, power lifters, and bodybuilders increased. Over the years, their use spread to many professional sports, especially those in which strength and body weight were important for success (e.g., football). Testosterone was the drug of choice in the 1950s, which was replaced by more elegant synthetic compounds over the next three decades, primarily because of their slightly higher percent of anabolic versus androgenic effects and their relative resistance to detection by current laboratory tests. Use spread to collegiate and amateur athletes as evidenced by the 50% positive tests obtained by the International Olympic Committee during unannounced urine screens in 1984 and 1985 (6). The 1990s saw a return to the use of testosterone, which is thought to be due to improved gas chromatographic methods of detecting the synthetic compounds and the continued difficulty of accurately detecting exogenously administered testosterone (7). However, another trend toward using other types of performance-enhancing aids has evolved in the wake of pure AAS abuse.
It often is difficult to determine whether the attraction of the drugs is related to any beneficial effect on the individual’s performance, because the drugs rarely are taken in the absence of a training program that includes exercise and sound nutrition (8). This concept punctuates the second aspect of AAS abuse among athletes—it usually occurs during training periods, which typically can begin weeks and even months before a competitive event or season. The need for these drugs by most athletes decreases during actual competition, and so the active use can decline. However, with the advent of mandatory urine testing at major athletic events, the risk of being caught also curtails use. Positive urine screens that are collected during the actual competitive event are usually due to the high sensitivity of the analytic methods to detect small amounts of metabolites that have persisted long since use of the AAS has ceased. The fact that a hair gas chromatographic test has been validated may have a greater impact on detecting AAS among athletes (9). Despite the enhanced methods of detecting these complex compounds, controversial use of AAS has tainted a large number of sporting events including Major League Baseball, track and field, and, most recently, professional cycling— some of these have led to congressional investigations, and elite athletes continue to be stripped of accolades because of discovered abuse in some cases like the Tour de France—no winner was declared because drug use was so pervasive.
New-Generation “Performance Enhancers”
With the availability of more sophisticated urine testing procedures, the likelihood that an athlete can avoid being caught using AAS is decreasing somewhat, and the advent of detecting drugs like erythropoietin has contributed to the identification of a widespread use of this performance enhancer in professional cycling. Nevertheless, the desire for new-generation performance-enhancing drugs and nutritional supplements continues to grow. Moreover, many of these agents have been extremely difficult to detect using standard laboratory procedures, not because the technology is limited but because these substances are found naturally in the body (10), and so carbon isotope mass spectrometry is needed (11). These include other hormones such as human growth hormone (somatotropin), dehydroepiandrosterone, erythropoietin, and thyroxine. Cadaver pituitary growth hormone has been replaced by recombinant human growth hormone, and the latter has been found to increase strength, peak power output, and fat-free mass index decreased after only a short course of the recombinant hormone (12).
Drugs belonging to other pharmacologic classes continue to be popular as potential agents to “boost” performance. These include the mixed agonist/antagonist opioids such as butorphanol and nalbuphine; the beta-adrenergic agonist clenbuterol; “hormone helpers” such as gamma hydroxybutyrate, clonidine, and human chorionic gonadotropin; and testosterone stimulants such as clomiphene and human chorionic gonadotropin. In addition, a variety of diuretics (acetazolamide, furosemide, spironolactone, and triamterene) are used to help clear the AAS and their metabolites from the urine before drug testing. Knowledge of these drugs, where to get them, doses to use, and even recipes for adding them to training programs can be found in a number of “underground” guides as well as from a variety of Web sites. In fact, a growing concern is that many individuals have now turned to the web as a major source for purchasing these agents, and it appears that there are hundreds of thousands of sites offering underground information on how to use them (13) and even offering to sell AAS outright (14); clinicians are well advised to be aware of these practices because the sites are often very “pro” drug use and question the knowledge or authority of those in the medical field. The accuracy of many of the claims on these sites is dubious at best.
It is not just the novel drugs that are of interest, but users continue to seek out veterinary or animal husbandry products. For example, trenbolone is an AAS that is often used to increase muscle growth/meat production in cattle (15) and is usually delivered via an implant into the cow’s ear. In their paper on web-based AAS information, Brennan et al. (13) noted that there were many sites that described how to remove the estrogens from this formulation, rendering it more suitable for human bodybuilding purposes.
At-Risk Populations
It is now well established that athletes are not the only individuals to use and abuse AAS. Abuse has now appeared in adult nonathletes and even in young boys who may be using them to simply improve their appearance (16). Women are also using these drugs, but all estimates indicate that the percentage remains much lower than in males. These factors encouraged the U.S. Congress to enact the Anabolic Steroids Control Act, which effectively placed all of these compounds, including testosterone and its many analogues, in Schedule III of the federal Controlled Substances Act (states, of course, have the option of scheduling these drugs even more restrictively under state law). Schedule III includes opioids such as nalorphine, stimulants such as benzphet-amine, and depressants such as butabarbital and thiopental.
The 1990s was rife with a number of surveys demonstrating that the incidence of AAS use and abuse by adults and adolescents was lower than that of other drugs of abuse (17,18). The data suggested that AAS were used by less than 2% of the adolescents surveyed and less than 1% of older respondents. During the ensuing 5 to 6 years, new data revealed some concerning trends in AAS abuse, particularly among the youth. Use among boys in general was reported to be greater than 3% (19), and in certain populations of 15- to 19-year-old boys, nearly 10% reported using AAS (20). In a cross-sectional assessment using the 2003 Centers for Disease Control and Prevention National School–based Youth Risk Behavior Survey database (21), Elliot et al. (22) reported that 5.3% of the 7,544 females in grades 9 to 12 used AAS. In addition, these young women also engaged in a number of other unhealthy life choices including using tobacco, marijuana, diet pills, carrying weapons, and having sexual relations before the age of 13. These authors also noted that AAS-using females were less likely to participate in team sports; this fuels the belief that children and adolescents have poor body image (23). This rate of AAS use among females punctuates the twofold to fourfold increase in AAS use that was reported by Yesalis et al. (24) in the 1990s. However, steroid use appears to decline with age, and desire to weigh more was a strong predictor of AAS use by males, but female AAS users were more likely to have higher body mass indices and a poorer knowledge of nutrition (25). Another complicating factor in obtaining accurate information about AAS use in teenage girls is that surveys may contain imprecise language so that the term steroid is misinterpreted (26), leading to an inflated estimate of AAS use. Nevertheless, the recent report of the Monitoring the Future (27) notes that annual prevalence rates for 8th, 10th, and 12th grade boys are about 0.7%, 1.3%, and 2.5%, respectively. The rates for same age girls were 0.3% to 0.5%. Unfortunately, questions regarding “perceived risk” and “disapproval” of AAS were asked for only a few years. Peak perceptions of risk occurred in 1993 and have steadily dropped with a rather large plummet in 1998 and 2000. In general, when perceived risk drops such as when public events surrounding use by famous athletes (especially androstenedione) become widespread, use increases. Perceived risk has only slightly increased in past years, but disapproval rates have remained high for some years, which shows that it can be dissociated from perceived risk. While use among the lay public remains low, the incidence of use among individuals engaged in power sports and/or weight lifting can be 20% to more than 50% (28,29). As such, the clinician may need to weigh the impact of the media, peer pressure, and teasing/comments from parents as factors that predict or at least facilitate AAS use among young boys. Smolak and Stein (30) reported that the media and endorsements about male physical characteristics were strong correlates of a desire to attain a more muscular body. Indeed, in a web-based survey of 500 AAS users, 78% were noncompetitive bodybuilders and not otherwise engaged in athletic events (31).
Web-based surveys have another role as revealing potential indicators of future AAS use, based on current drug use patterns (32). Dunn et al. reported that 80% of respondents to the survey said that they used sports supplements such as vitamins and protein supplements. The authors suggest that the widespread use of sports supplements may in some way remove “barriers” for the future use of AAS. The sample also reported a high incidence (52%) of illicit drugs, which challenges the preconceived notion that AAS users are a health conscious group as a whole and rarely engaged in other drug use. This is apparently not the case as it has been shown that AAS use is positively correlated with the use of other licit and illicit drugs such as alcohol, cocaine, licit painkillers, methylphenidate, ketamine, and legal performance-enhancing agents (33). As might be expected, abuse of the two smoked drugs, tobacco and cannabis, was not consistently reported in the studies. The fact that AAS abusers are engaging in polypharmacy practices will only complicate efforts to define and implement safe and effective treatments.
The use of nutritional supplements by adolescent athletes has increased dramatically (e.g., testosterone precursors such as androstenedione, dehydroepiandrosterone, and androstenediol) (34–37), and use continues in spite of repeated evidence that small to moderate doses resulted in transient and modest increases in testosterone and as such had no discernible effect on body composition or performance (38–44). This dissociation between real efficacy and perceived effects is thought to be due to a lack of knowledge about supplements so that a comprehensive educational program might be useful in curtailing the use of these supplements (45).
In the Syrian hamster animal model, there is compelling evidence that adolescents are far more sensitive to the effects of AAS than their adult counterparts (46). The AAS-treated adolescent males had significantly higher sexual and aggressive behavior, whereas similarly treated adults had significantly lower levels of sexual and aggressive behavior. This model relates to the clinical condition as it is suspected that the neural “rewiring” that occurs in males during puberty sets the tone for future aggressive and violent tendencies (47) and that exposure to AAS during this critical time can increase the likelihood that aggressive acts result in violent behavior. The link between testosterone and aggressive behavior was further made by van Bokhoven et al. (48) who reported that 16-year-old boys who had criminal records had elevated testosterone levels than their peers and concluded that there was a positive relationship between testosterone and proactive and reactive aggression and self-reported delinquent behavior.
Figure 17-1 depicts some of the more commonly identified effects and side effects of AAS use in adolescents. High-dose AAS use during adolescence has the potential of causing significantly more problems when adulthood is reached (49). Some of the effects are easier to identify than others, so the challenge to the clinician in detecting AAS use in his or her patients is to know the risk factors, be able to identify the constellation of signs and symptoms of use, and ask the correct questions when exploring use patterns (50). The clinician may need to be vigilant when presented with requests to treat moderate to severe acne, especially in 18-to 26-year-old males, because the incidence of acne is 50% in AAS users and thus may be a clinical indicator of abuse (51). As always, the clinician must be well informed of the facts about these drugs and be able to present themselves as a credible source of information.
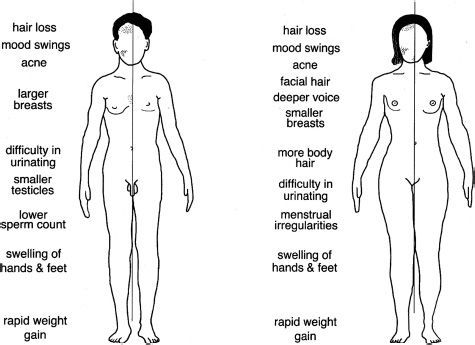
FIGURE 17-1 Side effect profiles of AAS in male and female users.
THERAPEUTIC USE AND MISUSE
Therapeutic Use
Although one might think that the therapeutic uses of AAS are of less concern to the addiction medicine specialist, in reality, most physicians are asked to give prescriptions for these drugs far more often than they are asked to help treat someone who is dependent on the drugs. Thus, knowledge of these medical situations might help in discussions with a potential abuser because these individuals are likely to be aware of the medical reasons for their prescription and may use such information in their initial attempts to obtain legal medications to support their training or alter their appearance.
Males may receive AAS for replacement therapy when the testicles fail to function, because of either congenital or traumatic factors, or when puberty is delayed and short stature would result. The doses that are prescribed, however, are much lower than those used by bodybuilders. The equivalent of 75 to 100 mg per week of testosterone suffices as replacement, but weight lifters and bodybuilders have reportedly used weekly doses of 1,000 to 2,100 mg of methandienone (52,53). Women are occasionally treated with androgens when metastatic breast cancer has spread to bone. Methyltestosterone is combined with estrogen (Premarin) to help alleviate some of the signs and symptoms of menopause. Very recently, nandrolone has been used in combination with exercise to increase lean body mass in patients who are on dialysis (54).
Both males and females might receive the more anabolic agents during treatment of a rare form of hereditary angioedema. Acquired aplastic anemia and myelofibrosis both result in deficiencies of red blood cell production, which is combated with drugs that have equal amounts of anabolic and androgenic effects. Sometimes, these drugs can be useful in treating the trauma associated with burns and AIDS. Finally, just as was done in post–World War II, steroids with more anabolic activity are useful in treating muscle wasting that is secondary to starvation.
Misuse
AAS are abused by three distinct populations: (a) athletes who use them to improve performance, (b) aesthetes who use them solely to improve appearance and perhaps gain some weight, and (c) the fighting elite who use them to enhance aggression and fighting skills (55). Identifying to which of these three populations a patient belongs is the first step to understanding the pattern of use and determining the best treatment plan to follow.
Athletes
Athletes use AAS for one reason: to improve their performance. Perhaps one of the greatest mistakes a clinician makes in dealing with an athlete is attempting to dissuade their use on the grounds that the drugs cannot improve performance. In fact, this is not true. The older research studies that purported to show that the effects of AAS were no different than placebo suffered from a number of methodologic problems, did not control for motivation, and failed to document the amount of physical training. In addition, ethical considerations prevented the investigators from administering extremely high doses, which are considered necessary to achieve the muscle-building effect. Negative findings also have been attributed to the use of only one drug at a time in the research studies, whereas athletes in training typically use multiple drugs in combination. The continued use of these drugs is based on the belief that they increase muscle capacity, reduce body fat, increase strength and endurance, and hasten recovery from injury (56). Many athletes also believe that AAS-assisted training allows the user to increase both the frequency and the intensity of workouts—factors that contribute to any direct benefits of the drugs (57). A recent web-based survey revealed that bodybuilders and weight lifters use on average 3.1 agents, engage in cycles that last 5 to 10 weeks in length, and use doses that are 5 to 29 times greater than physiologic replacement doses (58). Rates of use among individuals in fitness centers are also much higher (~ 12.5%) than the general population (59).
In the world of professional weight lifting and bodybuilding, AAS are used in three basic patterns: “stacking,” “pyramiding,” and “cycling.” Stacking is the practice of using multiple products at the same time. Users believe that the beneficial effects of one drug will complement those of another and that they will only achieve real benefits through a specific combination. There are now animal data to support the notion that stacking AAS can result in an altered pharmacologic response. Wesson and McGinnis administered a number of combinations of testosterone, stanozolol, and nandrolone to adolescent male rats and found that behavioral and endocrine effects were altered. Furthermore, this simulated “stacking” procedure revealed that the level of androgen receptor occupation did not directly correlate with the effects of the combined agents (60). A pyramid plan involves starting with a low dose and then gradually increasing the dose until peak levels are achieved a number of weeks before competition. The individual then slowly decreases or tapers the drug dose down, and, because the beneficial effects of AAS persist long after their use has been discontinued, the athlete will be primed for the competitive event. Cycling refers to the practice of using different combinations over a period to avoid the development of tolerance or loss of effectiveness. Thus, different combinations of drugs are used over a 6- to 12-week period, after which another drug or combination is substituted.
A rather poignant example of how extensive the use pattern can be is provided in Table IV of the review by Graham et al. (11). This table details a 16-week profile of stacking, pyramiding, and cycling of 19 different drugs from a half-dozen different pharmacologic classes by a current UK bodybuilding champion. The breadth of combinations, patterns, and huge doses is quite extensive, and while this pattern appears to be on one end of the spectrum, this practice is widespread, and the clinician will find it necessary to become familiar with a number of different drugs (like diuretics, thyroid hormone, and insulin) as a reminder that few individuals abuse a single agent and that other medications are used to either “boost” or facilitate the elimination of target drugs.
When prescriptions for AAS cannot be obtained, individuals may sometimes turn to veterinary products (as noted above). It is an interesting paradox when young bodybuilders profess to be on strict diets and use only the purest of vitamin and dietary supplements, yet they will self-administer drugs for which use in humans has not been approved. Products that are not approved for use in the United States typically are obtained by mail order from abroad. Because the testing of these products in some other countries is not as stringent as that in the United States, patients should be cautioned about using such products. Finally, there is an extensive black market of AAS that supports a rather large percentage of inactive products that are falsely advertised as containing anabolic steroids.
Aesthetes
Another group of users is composed of young boys and girls who use these drugs primarily to increase their weight or to improve their physical appearance (61–64). This desire for weight gain among a group of adolescent boys who are not yet taking AAS may place them at risk for initiating use (63). This trend is disturbing because these authors noted that a significant number of the boys were unaware of the most dangerous risks associated with AAS use. A recent study of the prevalence of AAS use among 6th to 12th grade Canadians revealed that 2.8% of the respondents had used these drugs over the past year (65). A disturbing trend was that 29.4% of these students reported that they injected the drugs and 29.2% of these reported that they shared needles with friends. Young AAS users are also likely to use other drugs such as marijuana, smokeless tobacco, and cocaine (66). These authors also reported a high percentage of needle-sharing behavior among adolescents.
In general, the doses used by adolescents and others who want to improve their appearance are substantially lower than those used by adult athletes (67). Further, the pattern of lower doses and intermittent cycles of use is likely to obviate the development of major side effects. However, because young boys are often still in transition because of hormonal changes associated with puberty, these drugs can have other significant effects. For example, the epiphyseal plate of the femur can close prematurely and actually stunt a boy’s growth (68), which is contrary to what a significant number of adolescents believe. More importantly, these young users may be particularly sensitive to the increased aggressive effects resulting from their use (67).
Apparently, a substantial proportion of these adolescents are also unaware of the side effects of AAS. Although educational programs have been slow to incorporate these drugs in the lesson plans, the real reason that the public is so unaware of the risks is that these drugs are probably not a severe health hazard when taken intermittently and in low to moderate doses (67). Because programs that simply emphasize the negative aspects of drugs of abuse are ineffectual at curtailing use (69), the health professional should balance the discussion about AAS abuse with the straight facts and not try to overstate the degree of harm. Such actions will only alienate the patient. Unfortunately, these young people know that only a small percentage of users actually experience very serious and deadly outcomes and that it will not happen to them. For the others, the side effects (except for some effects in women) are largely reversible.
Fighting Elite
Very little is known about this population of AAS users. This profile was originally described by Brower (55) and includes individuals who seek to increase their strength in order to perform their job. Another desired effect is the increase in aggressiveness that may also help them with their jobs. Thus, bouncers at bars, security personnel, and even law enforcement officers (70,71) have been reported to take these drugs.
Personality Profiles
A study of the personalities of AAS abusers by Cooper et al. (72) identified a high rate of abnormal personality traits in a sample of 12 bodybuilders who used AAS compared with a matched group who did not. Along with being heavier than the controls, the users were more likely to score higher on measures of paranoia, schizoid, antisocial, borderline, histrionic, narcissistic, and passive–aggressive personality profiles. Further, the incidence of abnormal personality traits before AAS use began was not different from the control group, suggesting that such disturbances are secondary to their use. Users also reported that they believe that AAS not only enhance physical strength and athletic ability but increase confidence, assertiveness, feelings of sexuality, and optimism (73). There appears to be both a pathologic perception of body image and a very narrow (stereotypic) view of what a male body should look like among AAS users (74). The term reverse anorexia nervosa has been coined by this group to describe symptoms association with muscle dysmorphia or a pathologic preoccupation with muscularity (e.g., not willing to let their bodies be seen in public). This particular form of body dysmorphic disorder may be associated with psychopathology as evidenced by a greater incidence of suicide attempts, higher frequency of substance abuse, and poorer quality of life (75).
ADVERSE EFFECTS
A great deal is known about the side effect and toxic profile of these drugs, and in the last few years, an even better appreciation for the risks of using these drugs has occurred. Much of the recent literature has focused on the short-term toxicity of these agents, particularly on cardiovascular and hepatic function. However, since AAS abusers rarely seek treatment for their “abuse” of these drugs, they will present with just the side effects and may not reveal their history of high-dose AAS use. One important consequence to consider is that as AAS users age, their use may subside, but potentially long-lasting organ damage may have occurred that may accelerate the deterioration that occurs during the normal aging process. As AAS abuse peaked in the 1980s, there is likely a generation of older men who may begin to experience the consequences of their past use.
Side effects are generally reversible, but more serious medical consequences and even toxic reactions appear to involve primarily blood chemistry, endocrine function, liver, the cardiovascular system, and the nervous system. Reports that excessive amounts of these drugs lead to certain types of malignant cancers have not been substantiated. Overall, even the more serious side effects have disappeared within 3 months of discontinuing their use, yet benefits such as increases in lean body mass and increased diameter of muscle fibers remain (76). Although the side effect profile of AAS has been well documented in adults, less is known about how chronic use of high doses of AAS will affect adolescent users.
Administration of the 17-alkylated androgens can cause a dramatic reduction in high-density lipoprotein (HDL) cholesterol, but because there is a nearly equal increase in low-density lipoprotein (LDL) cholesterol, there is no net change in total cholesterol levels (77). Other agents such as nandrolone and testosterone esters fail to produce this profile (77,78). Although the long-term detrimental effects of altered HDL/LDL ratios are known to predispose humans to atherosclerosis, documented morbidity and mortality as a result of AAS use have been rare (79,80). The lack of direct correlations may also be due to the fact that different steroids have varied effects on lipid dynamics (78). Thus, although users stack different drugs to improve the beneficial effects, this practice may actually afford some protection against these side effects. Further, the relative paucity of coronary vascular disease in athletes who use these drugs may also be due to the fact that other risk factors (e.g., diet, exercise, low body fat) compensate for any negative contribution afforded by the HDL/LDL profile. Such protection, however, may not be present in individuals who use AAS just to improve their appearance and do not engage in athletic activity. Platelet aggregation (81) and increased red blood cell production and slight increases in systolic blood pressure have been suggested to be important factors that increase an individual’s risk for thrombo-embolic disorders (1,82).
Because testosterone exerts an inhibitory action on the hypothalamic–pituitary axis, administration of natural or synthetic analogues of testosterone decreases testicular size and sperm count (83,84). Residual amounts of active metabolites may keep the levels of follicle-stimulating hormone and luteinizing hormone low, and coupled with the relatively long cycle to produce sperm, the recovery is likely to be slow but often is complete. Aromatization is the process by which steroid hormones are interconverted. For example, testosterone is converted to estradiol and estrone, and high-dose male AAS users can have circulating estrogen levels of normally cycling women (1). These circulating estrogens exert the usual feminizing effects, such as gynecomastia. Compounds that resist aromatization (e.g., fluoxymesterone, mesterolone, stanozolol) may not result in the feminizing effects (85).
Although a wide variety of medical disorders (and even exercise) can increase the amount of liver enzymes in the blood, this response is primarily limited to the use of oral, 17-alkylated AAS. The relationship between these drugs and elevated enzyme levels exists because these orally effective drugs are metabolized by the liver, the first-pass effect delivers an exceptionally large percentage of the dose to the liver, and abusers typically take excessive doses that further stress liver function. This profile often results in cholecystic jaundice (86), but because inflammation and necrosis are not present, the symptoms are limited to an accumulation of bile, which spills over into the blood. Interestingly, many bodybuilders use this side effect as a metric of their dosing regimen and titrate themselves to levels that just precipitate jaundice (87).
Peliosis hepatitis is a disorder characterized by blood-filled cysts scattered throughout the liver; a detailed description of the history of this disorder and its relationship to AAS abuse is presented elsewhere (88). It has been associated with the 17-alkylated androgens, rarely results in symptoms, and likely resolves with discontinuation (89).
The evidence linking 17-alkylated androgens with hepatic tumors is well established. Except for the fact that the androgen-related adenomas are typically larger, the profile resembles that of women who take birth control pills. The risk for developing hepatocellular adenomas ranges from 1% to 3% of users (77), and as with peliosis hepatitis, these adenomas rarely result in symptoms and are often not documented until a routine autopsy is performed.
A better appreciation for the mechanism of hepatic toxicity is now apparent as prolonged AAS use appears to increase lysosomal hydrolase activity and decrease some components of the microsomal drug-metabolizing system (90). These macroscopic changes may very well lead to the inflammatory or degenerative lesions in centrilobular hepatocytes, ultrastructural alterations in canaliculi, and degenerative changes in mitochondria and lysosomes. Stanozolol, along with the other orally administered AAS, is known to induce these effects. Moreover, it is clear that chronic AAS use may negatively impact immune function by overactivating immune cell function while dampening immunologic responses (91). Testosterone, at higher concentrations, reduces extra- and intracellular superoxide and increases phagocytosis, indicating that the oxidative capacity of neutrophils has decreased.
AAS affect the cardiovascular system via their effects on HDL/LDL ratios and other blood products. However, there are reports that these drugs can directly affect myocardial tissue. The majority of the evidence comes from animal studies in which high doses of methandrostenolone result in myocyte necrosis, cellular edema, and mitochondrial swelling (92,93). Because these changes cannot be duplicated by exercise alone, it is likely that these effects were responsible for the clinical case report of an AAS user who suddenly died of cardiac arrest (94). Recent preclinical studies suggest that the combination of vigorous exercise along with AAS use may precipitate myocardial injury that is manifested by myocardial disarray, contraction band necrosis, interstitial fibrosis, and apoptosis (95). These direct cardiotoxic effects can result in hypertrophy, electrical and structural remodeling, and contractile dysfunction that can lead to increased risk of ventricular arrhythmias and sudden cardiac death (96). A 2013 clinical report supports the notion that AAS use (possibly in combination with cannabis) can contribute to ischemic stroke in adolescents (97), and a recent review of the extant clinical literature revealed a high incidence of cardiac toxicity associated with chronic use (98). Angell et al. (99) present two case studies (a 25-year-old bodybuilder and a 27-year-old professional skater) that highlight the impact that performance-enhancing drugs have on cardiovascular function, especially in athletes.
An adverse effect of AAS use during high-intensity training periods that is not well documented is the incidence of injury that may occur as a direct result of their use. A clinical case of bilateral quadriceps rupture profiles the risks involved (100). Although it might seem that the fact that users can train with these drugs well beyond what they would be able to tolerate without the drugs is responsible for injuries of this type, it is possible that the growth of muscle mass is not paralleled by an increase in ligament support, which can result in such failures.
Controversy remains over the degree and extent of the severity of AAS-induced extreme psychiatric effects often referred to as “roid rage.” These eruptions of frenzied violent behavior during a cycle of high-dose AAS have been described in a few case reports, but no laboratory studies verifying such reactions have been published. More frequently, cases in which psychiatric effects appear associated with drug use have been reported (101–105). The constellation of symptoms appears to most closely resemble those of hypomania or mania. The energized user of AAS talks faster, has more energy, sleeps less, and is be more impulsive, even to the extent of purchasing expensive cars (104). At the far end of the spectrum, mania may lead to delusions and even hallucinations. Interestingly, many individuals with body dysmorphic disorder present with delusions as well (106). Two studies (107,108) attempted to standardize the collection of these data and found that using structured interviews, the incidence of a full affective syndrome was present in 22% of a population of 41 bodybuilders (108). Another 12% displayed psychotic symptoms that clearly emerged during AAS use. The cohort of 20 weight lifters who used AAS experienced more somatic, depressive, anxious, hostile, and paranoid complaints than those who did not use these drugs (107). A 2012 survey (109) revealed that, compared to nonusers, AAS-dependent users had a 25.9% incidence of any psychiatric illness, with the majority of the issues being anxiety disorder (16.1%) and major depression (15.2%), which were statistically elevated.
Empirical evidence of drug effects on aggressive behavior has been obtained using the Karolinska Scale of Personality (110) and a human laboratory model of aggression, the Point Subtraction Aggression Paradigm (111). More recently, psychiatric side effects after supraphysiologic doses of combinations of AAS were reported to correlate with severity of abuse (112). Results from the personality scale indicate that a cohort of AAS users exhibits significantly more verbal aggression, impulsiveness, and indirect aggression. Yates et al. (113) reported that three measures of the Buss-Durkee Hostility Inventory (114), assault, indirect aggression, and verbal aggression, were elevated in a group of current or recent AAS users. The Point Subtraction Aggression Paradigm directly measures the amount of provoked aggressive behavior in the laboratory by ostensibly taking away points (that are worth money) from an individual who believes he is playing against another person. In reality, the subject plays against a computer program, and the experimenter actually controls the rate of provocation. Both aggressive and nonaggressive behaviors are recorded, so the effects of various drugs on responding per se can be viewed independent from aggressive responding. Using this model, moderately high doses of testosterone cypionate (600 mg, intramuscularly, once per week) can increase aggressive responding in individuals who had not used steroids before (115). Interestingly, animal models have confirmed that AAS administration increases aggressive behavior (116). As weight lifters and bodybuilders have reportedly used weekly doses that exceed three times that used in research studies, it is reasonable to suspect that aggressive behavior can result from these training programs.
Collectively, it appears that AAS use can result in hypomania and even psychotic symptoms, whereas depression may ensue during withdrawal. The lack of well-controlled prospective studies has prevented a more definitive association between AAS use and psychiatric disorders. It is unlikely that such data will become available in the near future because ethical constraints will preclude the conduct of any double-blind assessments of supraphysiologic doses of these drugs.
ADDICTION LIABILITY
AAS abuse includes a variety of social and psychologic components that are not easy to imitate either in animal models or in currently validated methods of assessing abuse liability in human volunteers. The concepts of perception, motivation, and expectation play a more pivotal role in the initial use and subsequent abuse of these compounds. Because the anabolic effects of AAS can be profound but slow to develop, it has been difficult to separate these “desired” muscle-building effects from direct reinforcement. Demonstrating tolerance and physical dependence on these agents has also proved to be elusive because there are limitations in the doses that can be given to human subjects.
Reward
Although the anabolic steroid addiction hypothesis was proposed nearly 20 years ago (117), few empirical studies have been conducted to actually test it. In the last 8 years, animal models of conditioned place preference and self-administration have been employed, and evidence is mounting that AAS may possess some weak reinforcing effects that are not related to athletic performance. In the one study by Su et al. (118) healthy non-AAS users described feeling euphoric, full of energy, and having increased sexual arousal after an acute dose of methyltestosterone. Although the magnitude of the response was modest, the results were consistent but have not been replicated.
Perhaps the most important concept to understand about AAS abuse is that these agents are not used in the typical patterns that are observed with traditional drugs of abuse such as cocaine, heroin, alcohol, nicotine, and marijuana. Indeed, AAS are often taken or injected once per week as part of an exercise program. It is well known that if the subjective effects of a psychoactive drug are sufficiently delayed after self-administration, then the drug’s reinforcing efficacy decreases and drug-seeking behavior is reduced (119). Although there are a few scattered anecdotal reports that high doses of AAS can elevate mood, no controlled studies have demonstrated that these drugs produce immediate positive mood effects or euphoria. AAS can act within minutes to hours on cell membrane receptor sites, but the real beneficial effects of such action (e.g., protein synthesis) take more time. So, because of the difficulties of conducting such studies with humans, animal models have proven to be most valuable in discerning the nature of the reinforcing effects of these compounds.
Testosterone was shown to be self-administered as hamsters preferred aqueous solutions of the steroid versus water (120). The rewarding effects of testosterone using conditioned place preference were described (121) but appeared to be dependent on the environmental cues as conditioned stimuli. A recent study in male rats demonstrated that these drugs may alter the sensitivity of brain reward systems (122). In that study, a 2-week treatment with methandrostenolone alone had no effect on brain reward systems, but a 15-week treatment with a cocktail of three different AAS resulted in a shift in the response patterns to brain electrical reward and amphetamine. In a related study, dopamine receptor density in nucleus accumbens was altered by supraphysiologic doses of testosterone in male rats, suggesting that dopamine levels are increased after AAS (123). This action was verified using positron emission tomography and found that chronic AAS treatment caused an up-regulation of the binding potential of dopamine in rat striatum (124).
Another potential link to drugs of abuse is that AAS share brain sites of action and neurotransmitter systems with opioids. In humans, AAS abuse is often associated with prescription opioid use, and in animals, AAS overdose produces symptoms resembling opioid overdose (125). This study also demonstrated that AAS modifies the activity of the endogenous opioid system.
The pharmacologic profile of the AAS is thought to be due to androgen binding to intracellular androgen receptors. This process takes about 30 minutes and ultimately alters gene expression, but it is now believed that AAS possess a nongenomic action that can be mobilized in seconds or minutes (126). There have been some recent advances in the understanding of how testosterone metabolites interact with the γ-aminobutyric acid (GABAA)/benzodiazepine receptor complex or dopaminergic neurons in nucleus accumbens to mediate testosterone’s hedonic effects (127).
The absence of a well-defined pattern of self-administration in animals is confirmed by the finding that humans cannot tell whether they have been given an active AAS or placebo (128). Marginal discriminations were made in two studies but only after a period of extended testing had been employed (53,129). However, it is likely that it was the side effects of these drugs that were detected, rather than any positive reinforcing effects. Because the latter are thought to regulate drug-taking behavior in both humans and animals, the question that remains is “why do humans use and abuse AAS?”
Collectively, these data from animal models suggest that AAS may very well be reinforcing, but the magnitude and strength of the direct rewarding effects of these agents are modest at best and do not appear to approach that of the more classic drugs of abuse such as heroin, cocaine, or nicotine. Because of testosterone’s role in a number of socially labile situations, it may be that it intensifies the rewarding aspects of these other behaviors and that is what contributes to the persistent use by a small fraction of the population.
Tolerance
The evidence supporting tolerance development is not strong, although there is a belief among users that cycling is a necessary practice to avoid its development. Twenty percent of a sample of weight lifters believes that tolerance develops, but more than 80% believe that dependence develops. Nevertheless, such concerns over lost efficacy with time appear to be without hard empirical evidence. As such, it must be assumed that the escalating doses that elite athletes use are not taken because tolerance develops to their effects but to increase the magnitude of the desired effects. The doses are increased slowly to minimize the side effects or to allow time to acclimate to them. When presented with this fact, some users are likely to confuse their behavior with tolerance.
Dependence
Although evidence of physical dependence on AAS has not been widespread, there are a few detailed reports of clear signs of withdrawal when their use was abruptly stopped (130–132). In a study of 49 male weight lifters (132), 84% reported experiencing withdrawal effects, and the most frequently reported symptoms were craving for more steroids (52%), fatigue (43%), depressed mood state (41%), restlessness (29%), anorexia (24%), insomnia (20%), decreased libido (20%), and headaches (20%). Interestingly, 42% of these subjects were dissatisfied with their body image during withdrawal as well. Those who reported being dependent on AAS generally took higher doses, completed more cycles of use, and reported more aggressive symptoms than those who did not report being dependent. However, the extent of dependence on AAS in the larger population of users may be considerably smaller as there have been no reported cases of withdrawal effects in female athletes or among patients who have been prescribed high doses for legitimate medical purposes.
AAS in fact can increase muscle mass and body weight, especially when used along with a regular training program. However, many of the “black market” AAS preparations sold during the late 1980s actually were devoid of any active ingredients, including AAS. In spite of the spread of these counterfeit drugs, users claimed to have experienced improvements in their performance. Herein lies the real difficulty in assessing the abuse liability of these compounds. They are not expected to have immediate beneficial effects, and so the delay in any improvement does not raise suspicion that the preparation may be inert. Nevertheless, whether these drugs actually increase muscle mass, improve performance, or increase endurance is really not the question that confronts the addiction medicine specialist. The fact that AAS-seeking behavior exists and that extremely high doses are used over relatively long periods suggests that there is a problem and should trigger further inquiry and subsequent treatment.
Physical dependence on AAS may be more insidious than with other drugs. It is quite likely that the initial involvement with AAS is related to the anticipated increased physical strength and body mass. Brower proposed a two-stage model of AAS dependence that incorporated the anabolic benefits early on but that physical dependence ensues after prolonged use of extremely high doses (133).
Thus, although physical dependence on AAS may be more rare than dependence on other drugs of abuse, the prudent clinician will be ever vigilant to identify the constellation of signs and symptoms that may signify dependence. Attempts to label the withdrawal signs and symptoms as opiate-like or ethanol-like may complicate the issue only because such an effort may conceal a real dependence on these other drugs. Thus, when obvious signs of distress are observed during periods of forced abstinence, it is worthwhile to consider the possibility that the individual may, in fact, be dependent on other drugs. There have been a few reports of opioid dependence in bodybuilders (134,135), and these individuals clearly met criteria for dependence on both drug classes. Thus, the possibility of polydrug abuse should always be considered when dealing with AAS abusers. Interestingly, according to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fourth Edition (DSM-IV) (136), the diagnosis of polysubstance dependence cannot be made if the individual meets criteria for dependence on one of the substances; the criteria for poly-drug abuse appear to be geared toward identifying individuals who experiment with a number of different drugs. As noted earlier, AAS users will rarely seek treatment for their abuse. Now that we have a better understanding of the constellation of issues that are present, current recommendations for treatment include a three-pronged approach (137): (a) address the body image disorder, (b) address the depression due to the hypogonadism during withdrawal, and (c) address the hedonic effects via pharmacologic and psychosocial treatments.
Diagnostic Classifications
AAS users will meet criteria for dependence via DSM-IV by having three or more of the following: (a) use continues over longer periods than desired; (b) attempts to stop are unsuccessful; (c) substantial time is spent obtaining, using, or recovering from their use; (d) use continues despite knowledge of their harmful effects; (e) physical signs of withdrawal appear upon cessation of use; (f) they are taken to relieve the withdrawal symptoms; and (g) a need to increase the dose to achieve the desired effect or that a markedly diminished effect occurred with continued use of the same dose. This latter criterion was added after some consideration over the behavior that many abusers exert in order to obtain these drugs. Importantly, more specific AAS criteria for classifying dependence have been proposed to be included in DSM-5 (138), which have been validated in the laboratory (139).
There is another factor that must be considered when attempting to diagnosis AAS abuse. In a study of 108 bodybuilders, Pope et al. (140) noted a rather high percentage of anorexia nervosa and uncovered a body image disorder that they labeled reverse anorexia. This condition shares many signs and symptoms of body dysmorphic syndrome (141). The profile of the former is that they view themselves as being too small and weak, when they are quite large and strong. The incidence of this disorder was 8% among AAS users and was not observed in any of the nonusers. The authors postulate that these body image disorders may have some influence on an individual’s decision to use anabolic– androgenic steroids. Because the perceived size, shape, and attractiveness of one’s body are likely tied to self-esteem (142) and, in general, men want to be 3 pounds heavier, taller, and have wider shoulders (143), AAS use may be viewed as a way of speeding up the process to attain physical attractiveness. This similarity in profiles between body image disorders and drug use might suggest that AAS abusers who present with a profile of body image disturbance may respond to the same treatments that have been used for body dysmorphic syndrome. Serotonin reuptake blockers have been marginally successful in treating body dysmorphic disorder (144), and although there have been no published studies to this effect with AAS users, fluoxetine has been marginally successful in a small sample of bodybuilders who presented with depression during withdrawal from AAS use (145).
ABSORPTION AND METABOLISM
Historically, AAS have been taken either orally or injected deep into the muscle as there are no intravenous formulations or smokable products. More recently, testosterone gel and patches for topical administration have been released on the market and offer another route to consider. By far, the greatest influence on subsequent development of toxic side effects is the route of administration. About half of an oral dose of testosterone is metabolized via the first-pass effect, so very large doses are needed. Some 17α-alkylated analogues of testosterone such as methyltestosterone resist such metabolism and so can be given orally in smaller doses. The oral route gives rise to a number of 17-alkylated metabolites, which are formed in the liver. This overload, not only of the metabolizing enzymes but also because the doses taken are so high, causes significant stress on this organ.
Testosterone is metabolized to 5α-dihydrotestosterone in certain tissues such as prostate gland, seminal vesicles, and pubic skin. Because 5α-dihydrotestosterone has two to three times the affinity for the androgen receptor as the parent hormone, the effects of testosterone are enhanced in these tissues. One of the more interesting aspects of testosterone’s metabolic pathway is that it is converted to estradiol in tissues that contain an aromatase enzyme (146). The biologic significance of circulating estrogens in males is unknown, but they may be involved with sex hormone– binding globulin and lipoproteins. Further, the estrogen that results from this metabolic process may interact with estrogen receptors to produce an anabolic effect (116,147). The 17α-alkylated analogues discussed above are not metabolized to either 5α-dihydrotestosterone or estrogen. Instead, they interact with the androgen receptor (1,148). Thus, the overall profile of relative anabolic to androgenic effects is not only due to the parent compound but to the profile of metabolites that result. With the advent of widespread use of these drugs during athletic competition, a number of analytic laboratories have been set up to detect either the parent drug or its metabolites (149,150). In addition to providing quantitative analyses of the various synthetic analogues, most labs measure the testosterone/epitestosterone ratio (the T/E ratio) as a metric of exogenous testosterone administration (151); the threshold for an acceptable (i.e., passing) ratio was originally set at 6:1 but has been lowered to 4:1, which has caused some controversy. This strategy of testing both the parent hormone testosterone with its major metabolite has provided a more reliable method of detecting illicit use of a hormone that is normally found in the body.
Another important advancement in detecting illicit testosterone use capitalizes on the natural abundance of 13C and its dissociation from the abundance of 12C in biologic systems (152), and the 13C/12C ratio should reflect that of the ingested carbon sources. Pharmaceutical grade testosterone is made from soya bean stigmasterol, which by its nature has a lower 13C content. Using GC combustion isotope ratio mass spectrometry, these differences can be detected and used to identify the “source” of the testosterone that is present in a biologic sample.
MECHANISMS OF ACTION
About 95% of the testosterone in males is synthesized in the testes, whereas the remaining 5% comes from the adrenals. The cholesterol used in the synthetic pathway comes from acetate that is stored in the testes and not from circulating blood levels. AAS have long been thought to exert their effects in the periphery, primarily by increasing the rate of RNA transcription (7,153). About half of the circulating testosterone is tightly bound to sex hormone–binding globulin, and the other half is lightly bound to albumin, from which it freely dissociates and from whence it can diffuse passively into target cells. After attaching to a steroid receptor in the cytoplasm, the hormone-receptor complex moves into the nucleus where it binds to sites on the chromatin, resulting in new mRNA. If the target tissue is skeletal muscle, then new myofilaments are formed, which causes myofibrils to divide (1,154). Because it is not completely understood whether this activity occurs at the supraphysiologic doses typically taken by AAS abusers, another mechanism was sought. It has been suggested that high doses of AAS cross-react with glucocorticoid receptors that control the catabolic rates of protein (1,155,156). The significance of the anticatabolic effect of these drugs is often ignored in lieu of the more direct effect of these steroids on protein synthesis. It is also possible that the stress of strenuous workouts is not felt by athletes taking AAS because the stress-induced increase in cortisol is blocked. This action would also permit the workouts to be longer and more vigorous, further improving performance.
It is possible that the physical changes attributed to a direct effect of AAS on protein synthesis may actually be mediated via a direct effect on the central nervous system. Such effects might result in increased motivation and intensity of training to a degree that performance is improved. Increased aggressive behavior may also play a role in the training process. It is likely that the use of supraphysiologic doses of these drugs can have both a direct effect on muscle tissue and an indirect effect by altering emotions such as motivation and drive such that the training periods are longer and more productive, resulting in improved performance.
The pharmacologic profile of the AAS is thought to be due to androgen binding to intracellular androgen receptors. This process takes about 30 minutes and ultimately alters gene expression, but it is now believed that AAS possess a nongenomic action that can be mobilized in seconds or minutes (126). There have been some recent advances in the understanding of how testosterone metabolites interact with the GABAA/benzodiazepine receptor complex or dopaminergic neurons in nucleus accumbens to mediate testosterone’s hedonic effects (127). The concept that AAS interact directly with peripheral benzodiazepine receptors in rat brain was explored over a decade ago (157). These receptors are mitochondrial proteins that are involved with regulating steroid synthesis and transport, so it seems plausible that their activation via exogenous AAS could have an impact on behavior that is mediated by these receptors.
The increase in body weight, especially during the first weeks of use, is almost certainly attributed to the stimulation of mineralocorticoid receptors, resulting in sodium and, ultimately, water retention as well as increasing amounts of circulating estrogen that has been aromatized from testosterone. This effect gives the muscles, particularly the deltoid, a “puffy” appearance. The increase in red blood cell production is probably the major reason that long-distance runners may use these drugs because endurance, rather than bulk muscle mass, is an asset in this sport. Blood volume probably increases as a result of erythropoietin synthesis. This effect is due to direct action on bone marrow and easily leads to a rise in hematocrit (158).
FUTURE VISTAS
Although AAS are not specifically mentioned in the Healthy People 2010 initiative, the federal government has set a national goal to increase the “proportion of adolescents not using alcohol or any illicit drugs during the past 30 days” (159). These drugs continue to be used and abused by individuals for a wide range of reasons. Further, as former heavy users of anabolic–androgenic steroids enter middle age, it remains to be seen whether there are psychiatric of other medical consequences of this form of drug abuse (160), an issue that the clinician may need to address when presented with organ diseases in individuals who, upon initial presentation, exercised regularly, ate balanced meals, and did not smoke for the past 30 years. The addiction liability of AAS may have a central nervous system mechanism that complements the anabolic effects. As quantitative methods for detecting AAS have become more sophisticated and specific, individuals have switched to using nutritional supplements, endogenous peptides such as growth hormone and epoetin. Recent attempts to determine reference ranges for urinary steroid “profiles” (161) represent a movement that has long been awaited and may help to better define when illicit use has occurred. Although the anabolic effects of many of these supplements are not well documented, side effects can still occur and remain a concern. Selective androgen receptor modulators, capable of increasing muscle mass with little androgenic effects (and have already been banned from the Olympics), will join the ranks of the designer AAS like tetrahydrogestrinone and desoxymethyltestosterone as the performance-enhancing substances of the future. While the designer drugs and novel peptides can now be detected, the way has been paved for an emerging biotechnique that implements recombinant DNA such that manipulated genes can be inserted into mammalian cells. This practice, called gene doping or performance-enhancing genetics, has been defined by the World Anti-Doping Agency as “the non-therapeutic use of genes, genetic elements and/or cells that have the capacity to enhance athletic performance” (162). This commission is unique in that human gene doping has not yet occurred, but World Anti-Doping Agency has taken the initiative to set standards for future events. Conceptually, gene doping would involve using scientific techniques to manipulate DNA in a manner that would improve athletic performance (163,164). Finally, the medical community needs to appreciate the fact that few AAS abusers will seek drug abuse treatment, but as they age, the medical consequences of years of using excessive doses of these agents will take its toll on body organs and may present the clinician with conditions that will not have an obvious cause.

INTRODUCTION
One of the challenging aspects of teenage drug abuse is the fact that the trends and types of drugs that are being abused are constantly changing. New substances are available which may pose a great danger to teenagers. New agents include “Bath Salts,” synthetic cathinones, which are derivatives of cathinone, a naturally occurring amphetamine analogue found in the leaves of the Catha edulis plant, and synthetic marijuana such as Spice and K-2, herbal mixtures that typically contain some amount of Cannabinoid 1/Cannabinoid 2 receptor agonists are being used and promoted on the internet (1,2).
New, synthetic drugs of abuse have increased at an alarming rate over the past several years. While “classic” drugs of abuse, such as cocaine, heroin and alcohol were traditionally agents of concern for abuse in society, newer novel psychoactive substances “designer” drugs are being created by clandestine laboratories have been on the rise since the late 1970s. Typically these drugs are designed to mimic already existing illegal substances such as marijuana and amphetamines. Promoted as “legal highs” these substances are easily accessible in gas stations, convenience stores, internets and head shops (3). These substances are particular a concern for teens and young adults in that they are easily affordable, packaged in colorful wrappings that do not appear dangerous and are typically given fun, catchy names which draw attention (3). Use is not detected in standard toxicology screens, which is another draw for users who believe their use of drugs will not be discovered. Designer drugs of abuse have become a major public health concern and safety risk.
Designer drugs are typically created when clandestine chemists modify the structure of an existing drug, for example adding a methyl group to the compound, thereby creating an analog drug with similar properties (4). The new chemical is made to be sufficiently different from its parent compound and therefore not covered by existing drug laws (4). Different chemical structures ultimately mean potential different physiologic effects, and a resulting clinical picture that often times cannot be predicted based on presentation. Additionally, since there is no regulation of the production of these substances, the composition and dose of the active ingredients may vary substantially between drugs, even those under the same label, leading to challenges among clinicians attempting to diagnose and treat, in addition to added risk of exposure to the user (5). While new legislation has been introduced to attempt to make these lines of drugs illegal (6), drug creators are typically far ahead of the law, designing new drugs that escape current regulation.
Currently, the majority of new substances available can be characterized as synthetic cannabinoids, opioid-like substances, amphetamine-like substances or hallucinogens (7). However, these new substances are very concerning as the have been associated with significant life-threatening adverse events, and have been implicated as the cause for numerous violent acts (2,3,7,8). This presents a remarkable challenge to the primary care clinicians, who need to be able to both recognize and be able to treat patients that are exposed to these substances. There are several sources available for information for the clinician in need of medical information.
POISON CONTROL CENTERS
The United States has 57 Poison Control Centers who serve the United States as a resource for expertise in medical toxicology. The national phone number, (800) 222-1222 puts callers directly in-touch with their regional center. Medical professionals that are specialists in toxicology answer the phones and are available for all types of consultations and questions. Physician coverage is available 24 hours a day, 7 days a week. Discussions with the poison control center are confidential, and serve as a resource for information on a variety of topics, including drugs of abuse, and serve to both identify and guide management for patients exposed to drugs. The Poison Centers also provide national surveillance for drug exposures. The American Association of Poison Control Centers, an organization that supports the individual centers, has information about the clinical symptoms expected with exposure to some agents available on their Web site (Table 17-1 ).
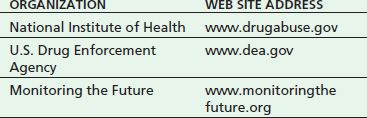
TABLE 17-1 WEB SITE ADDRESSES FOR SOURCES CONTAINING INFORMATION ON EMERGING DRUGS OF ABUSE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


