Chapter 14 The Pancreas
DEVELOPMENTAL DISORDERS
INFLAMMATION
5 What is acute pancreatitis?
 Interstitial or edematous pancreatitis: This mild inflammation is characterized by edema and widening of interstitial spaces that contain scattered inflammatory cells. There is no or only minor necrosis of acinar cells. Interstitial pancreatitis occurs relatively often in severely sick people, in various forms of shock, and after prolonged operations. It may be recognized by mild elevation of pancreatic enzymes in blood. It requires no treatment and heals spontaneously.
Interstitial or edematous pancreatitis: This mild inflammation is characterized by edema and widening of interstitial spaces that contain scattered inflammatory cells. There is no or only minor necrosis of acinar cells. Interstitial pancreatitis occurs relatively often in severely sick people, in various forms of shock, and after prolonged operations. It may be recognized by mild elevation of pancreatic enzymes in blood. It requires no treatment and heals spontaneously.7 Describe the sequence of a hypothetical event leading to acute pancreatitis
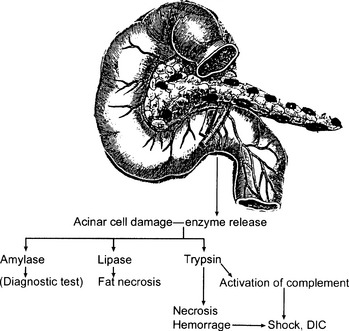
The inappropriate activation of enzymes inside the pancreas leading to autodigestion is thought to occur in the following sequence (Fig. 14-1):
 Increased pressure inside the excretory portion of the pancreas that reverses the flow of bicarbonate-rich pancreatic juices backward into the acini
Increased pressure inside the excretory portion of the pancreas that reverses the flow of bicarbonate-rich pancreatic juices backward into the acini Rupture of damaged acinar cells leading to a release of digestive enzymes into the interstitial spaces and peripancreatic tissue
Rupture of damaged acinar cells leading to a release of digestive enzymes into the interstitial spaces and peripancreatic tissue Autodigestion of proteins, lipids, and carbohydrate moieties of cells forming the pancreas, peripancreatic fat tissue, and blood vessels
Autodigestion of proteins, lipids, and carbohydrate moieties of cells forming the pancreas, peripancreatic fat tissue, and blood vessels9 List other exogenous causes of acute pancreatitis
 Drugs (More than 100 drugs are known to cause pancreatitis, but most often it occurs in patients taking azathioprine and mercaptopurine (2% of patients may have mild pancreatitis). Corticosteroids and high doses of estrogens are also associated with higher incidence of pancreatitis.)
Drugs (More than 100 drugs are known to cause pancreatitis, but most often it occurs in patients taking azathioprine and mercaptopurine (2% of patients may have mild pancreatitis). Corticosteroids and high doses of estrogens are also associated with higher incidence of pancreatitis.) Surgery (Surgeons refrain from operating on or palpating the pancreas unless it is essential for the treatment.)
Surgery (Surgeons refrain from operating on or palpating the pancreas unless it is essential for the treatment.) Diagnostic procedures (Endoscopic retrograde cholangiopancreatography [ERCP] used to visualize pancreatic ducts and obtain cytologic samples may damage the pancreas. Note that it is not advisable to perform diagnostic fine needle aspiration biopsies of the pancreas.)
Diagnostic procedures (Endoscopic retrograde cholangiopancreatography [ERCP] used to visualize pancreatic ducts and obtain cytologic samples may damage the pancreas. Note that it is not advisable to perform diagnostic fine needle aspiration biopsies of the pancreas.)10 List endogenous causes of acute pancreatitis
 Hyperlipidemia: Obesity is a known risk factor, but the exact mechanism of pancreatic injury is not completely understood. It is thought that fatty acids may injure acinar cells. Endogenous hyperlipidemia (especially type V) is also associated with an increased incidence of acute pancreatitis.
Hyperlipidemia: Obesity is a known risk factor, but the exact mechanism of pancreatic injury is not completely understood. It is thought that fatty acids may injure acinar cells. Endogenous hyperlipidemia (especially type V) is also associated with an increased incidence of acute pancreatitis.11 What are the gross pathologic features of acute hemorrhagic pancreatitis?
 Necrosis of fat tissue around the pancreas or omentum: Fat necrosis leads to the formation of fat soaps. These foci appear white, resembling chalk.
Necrosis of fat tissue around the pancreas or omentum: Fat necrosis leads to the formation of fat soaps. These foci appear white, resembling chalk.12 Describe the histologic findings in acute pancreatitis
 Necrosis of pancreatic acini, ducts, and blood vessels: In these anatomic sites, the component cells lose their outlines and nuclei.
Necrosis of pancreatic acini, ducts, and blood vessels: In these anatomic sites, the component cells lose their outlines and nuclei. Fat necrosis: Fat cells become indistinct and lose their internal structure. The entire field appears bluish because of the deposition of calcium salts. Specks of calcium soaps appear like dark blue aggregates or amorphous material.
Fat necrosis: Fat cells become indistinct and lose their internal structure. The entire field appears bluish because of the deposition of calcium salts. Specks of calcium soaps appear like dark blue aggregates or amorphous material.13 What are the most important local complications of acute hemorrhagic pancreatitis?
 Pseudocyst: Massive necrosis leads to liquefactive necrosis of the tissue, which becomes enclosed by granulation tissue. The granulation tissue transforms into a fibrous scar that contains the fluid full of pancreatic enzymes.
Pseudocyst: Massive necrosis leads to liquefactive necrosis of the tissue, which becomes enclosed by granulation tissue. The granulation tissue transforms into a fibrous scar that contains the fluid full of pancreatic enzymes. Abscess: Infection superimposed on pancreatic necrosis leads to abscess formation. It is associated with high mortality.
Abscess: Infection superimposed on pancreatic necrosis leads to abscess formation. It is associated with high mortality.14 What are the systemic (distant) complications of acute hemorrhagic pancreatitis?
 Shock: It is multifactorial but mostly due to increased vascular permeability caused by the action of pancreatic enzyme.
Shock: It is multifactorial but mostly due to increased vascular permeability caused by the action of pancreatic enzyme. Disseminated intravascular coagulation: Endothelial injury caused by pancreatic enzymes in circulation leads to the formation of platelet and fibrin thrombi in small vessels.
Disseminated intravascular coagulation: Endothelial injury caused by pancreatic enzymes in circulation leads to the formation of platelet and fibrin thrombi in small vessels. Adult respiratory distress syndrome: It is a manifestation of shock, but it also evolves because of enzymatic injury of the alveolar–capillary units in the lungs. Alveolar–capillary injury is accompanied by facilitated passage of fluids into the alveoli (pulmonary edema) and the formation of hyaline membranes.
Adult respiratory distress syndrome: It is a manifestation of shock, but it also evolves because of enzymatic injury of the alveolar–capillary units in the lungs. Alveolar–capillary injury is accompanied by facilitated passage of fluids into the alveoli (pulmonary edema) and the formation of hyaline membranes.16 Which enzymes appear in high concentration in blood during an attack of acute hemorrhagic pancreatitis?
 Amylase: It is a sensitive marker of acute pancreatitis, especially if the elevation is 4 times above normal values. Amylase appears in blood within hours of the onset of pancreatic injury. However, hyperamylasemia is not specific for acute pancreatitis, and it may be of extrapancreatic origin. For example, after cardiac surgery 30% of patients have hyperamylasemia, 50% of which is of salivary gland origin. The fallopian tubes also contain amylase, and it may be elevated in extrauterine pregnancy.
Amylase: It is a sensitive marker of acute pancreatitis, especially if the elevation is 4 times above normal values. Amylase appears in blood within hours of the onset of pancreatic injury. However, hyperamylasemia is not specific for acute pancreatitis, and it may be of extrapancreatic origin. For example, after cardiac surgery 30% of patients have hyperamylasemia, 50% of which is of salivary gland origin. The fallopian tubes also contain amylase, and it may be elevated in extrauterine pregnancy.17 Which other tests give abnormal results in acute pancreatitis?
 Leukocytosis: This is self-evident because pancreatitis is associated with a mobilization of neutrophils that infiltrate the necrotic tissue.
Leukocytosis: This is self-evident because pancreatitis is associated with a mobilization of neutrophils that infiltrate the necrotic tissue.Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree