Chapter 19 The Neurologic System
A. Mental Status Examination
5 What are the snouting, rooting, and sucking reflexes?
 Snouting is the labial pouting/pursing elicited by pressing a tongue blade on the patient’s lips.
Snouting is the labial pouting/pursing elicited by pressing a tongue blade on the patient’s lips.
 Rooting is the shift of the mouth toward a tactile stimulus. It can be elicited by gently stroking the lateral upper lip—or, in newborns, by touching the junction of the lips. This causes head-turning and mouth-opening, as if “rooting” toward the stroke (mom’s breast or the bottle).
Rooting is the shift of the mouth toward a tactile stimulus. It can be elicited by gently stroking the lateral upper lip—or, in newborns, by touching the junction of the lips. This causes head-turning and mouth-opening, as if “rooting” toward the stroke (mom’s breast or the bottle).
 Sucking is pouting or sucking following gentle touching of the patient’s lip. Normal in infants until weaning, it is absent in adults—except in diffuse frontal lobe injury.
Sucking is pouting or sucking following gentle touching of the patient’s lip. Normal in infants until weaning, it is absent in adults—except in diffuse frontal lobe injury.
10 What are the most important levels of consciousness? How do they deteriorate?
There are four levels of consciousness. In increasing degree of deterioration they are:
 Alertness: An awake person with normal level of consciousness (alert patient)
Alertness: An awake person with normal level of consciousness (alert patient)
 Lethargy: A sleepy patient who needs continuous stimulation to remain awake
Lethargy: A sleepy patient who needs continuous stimulation to remain awake
 Stupor: An unarousable patient who can still moan, withdraw, or roll around during exam
Stupor: An unarousable patient who can still moan, withdraw, or roll around during exam
 Coma: A patient who offers no purposeful response to stimulations of any kind
Coma: A patient who offers no purposeful response to stimulations of any kind
12 What is memory? How do you assess it?
Memory is the ability to register and recall prior sensory input. For testing purposes:
 Registration: Ask patients to name three objects and repeat them until fully learned.
Registration: Ask patients to name three objects and repeat them until fully learned.
 Recall: Distract patients for 3–5 minutes (by doing other parts of the exam, like testing attention and calculation). Then ask them to name the three objects previously learned.
Recall: Distract patients for 3–5 minutes (by doing other parts of the exam, like testing attention and calculation). Then ask them to name the three objects previously learned.
(1)Language
22 What is cerebellar speech?
Another disorder of articulation of sound, rather than ideation or perception (ataxic speech).
23 Beside cerebellar speech, what are the two most important types of dysarthria?
 Spastic dysarthria. This is due to damage of upper motor neurons (connecting the cortex to the spine), resulting in excessive and uncontrolled tone.
Spastic dysarthria. This is due to damage of upper motor neurons (connecting the cortex to the spine), resulting in excessive and uncontrolled tone.
 Flaccid dysarthria. This is due instead to damage of lower motor neurons, compromising all aspects of speech production. Lesions of individual cranial nerve(s) (brain stem stroke or peripheral facial nerve paralysis) also can cause dysarthria. For instance, Bell’s palsy may cause difficulty in saying “mo-mo-mo” (see Table 19-1).
Flaccid dysarthria. This is due instead to damage of lower motor neurons, compromising all aspects of speech production. Lesions of individual cranial nerve(s) (brain stem stroke or peripheral facial nerve paralysis) also can cause dysarthria. For instance, Bell’s palsy may cause difficulty in saying “mo-mo-mo” (see Table 19-1).
Table 19-1 Dysarthria and Possible Cranial Nerve Involvement
| Syndrome | Sounds | Possible Cranial Nerve Involved |
|---|---|---|
| Labial | “mo-mo-mo” | CN VII (facial nerve) |
| Lingual | “la-la-la-la” | CN XII (hypoglossal nerve) |
| Pharyngeal | “ka-ka-ka” | CN IX and X (glossopharyngeal nerve and vagus nerve) |
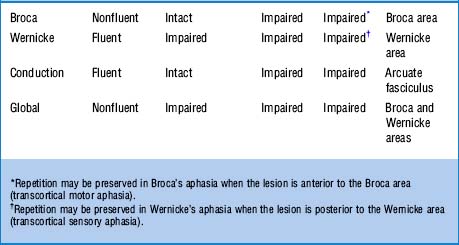
25 What are the most important defects in aphasia?
 Inability to understand language (receptive, sensory, posterior aphasia; also called fluent or Wernicke’s aphasia)
Inability to understand language (receptive, sensory, posterior aphasia; also called fluent or Wernicke’s aphasia)
 Inability to transfer signals from Wernicke to Broca (conductive aphasia)
Inability to transfer signals from Wernicke to Broca (conductive aphasia)
 Inability to properly execute speech (expressive, motor anterior aphasia; also called nonfluent or Broca’s aphasia)
Inability to properly execute speech (expressive, motor anterior aphasia; also called nonfluent or Broca’s aphasia)
Combined Broca’s and Wernicke’s aphasias constitute global aphasia.
26 What are the clinical differences between fluent and nonfluent aphasia?
 In fluent aphasia (Wernicke’s), talking is easy, but words are often jumbled and meaningless. There is difficulty in naming objects, repeating sentences, or comprehending. Speech is full of emptiness and gibberish “jargon,” even though patients seem unaware of it. In fact, they may even appear confused and almost psychotic. Reading impairment parallels the speech deficit. The responsible lesion is in the temporal or parietal lobe.
In fluent aphasia (Wernicke’s), talking is easy, but words are often jumbled and meaningless. There is difficulty in naming objects, repeating sentences, or comprehending. Speech is full of emptiness and gibberish “jargon,” even though patients seem unaware of it. In fact, they may even appear confused and almost psychotic. Reading impairment parallels the speech deficit. The responsible lesion is in the temporal or parietal lobe.
 In nonfluent aphasia (Broca’s), there is obvious struggling for words and great difficulty with speaking. Language is slow, made up of monosyllabic sentences, and full of latency. In fact, it resembles the labored use of English by tongue-tied foreigners. Although nonfluent aphasics have a hard time naming objects and repeating sentences, their comprehension of spoken and written material is often quite good. Yet, they may be dyslexic (i.e., making semantic errors and having difficulty in reading highly imaginable words). A writing deficit usually parallels the phonologic deficit. The responsible lesion is in the frontal lobe.
In nonfluent aphasia (Broca’s), there is obvious struggling for words and great difficulty with speaking. Language is slow, made up of monosyllabic sentences, and full of latency. In fact, it resembles the labored use of English by tongue-tied foreigners. Although nonfluent aphasics have a hard time naming objects and repeating sentences, their comprehension of spoken and written material is often quite good. Yet, they may be dyslexic (i.e., making semantic errors and having difficulty in reading highly imaginable words). A writing deficit usually parallels the phonologic deficit. The responsible lesion is in the frontal lobe.
31 What is cortical dementia? What is subcortical dementia?
 Cortical dementia is cortical damage resulting in aphasia, dyspraxia, agnosia.
Cortical dementia is cortical damage resulting in aphasia, dyspraxia, agnosia.
 Subcortical dementia is damage of the basal ganglia, thalamus, rostral brain stem nuclei, and frontal lobe projections. It results in bradyphrenia, a unique slowness of thought processes (such as cognition, motivation, and attention) that is absent in cortical dementia.
Subcortical dementia is damage of the basal ganglia, thalamus, rostral brain stem nuclei, and frontal lobe projections. It results in bradyphrenia, a unique slowness of thought processes (such as cognition, motivation, and attention) that is absent in cortical dementia.
B. Cranial Nerves Examination
35 How do you test CN I (olfactory nerve)?
By asking patients to close their eyes, occlude one nostril, and then smell through the open naris a distinctive scent—like cinnamon, cloves, or peppermint. Transient anosmia is common, usually resulting from simple colds or intercurrent sinus infection. Chronic anosmia (especially if congenital) is instead quite important (see Chapter 6, question 33). Note that anosmia can also be seen in frontal/temporal lobectomies or Parkinson’s disease.
36 How do you test CN II (optic nerve)?
 Visual acuity:Ask the patient to read an eye chart from a distance of 20 feet. Glasses or contacts are allowed, since the test measures the best corrected vision. A normal person reads at 20 feet letters that others also can read at 20 feet (20/20 vision). A person who reads at 20 feet letters that others can read at 40 is said to have an acuity of 20/40 (see Chapter 4, questions 1–15).
Visual acuity:Ask the patient to read an eye chart from a distance of 20 feet. Glasses or contacts are allowed, since the test measures the best corrected vision. A normal person reads at 20 feet letters that others also can read at 20 feet (20/20 vision). A person who reads at 20 feet letters that others can read at 40 is said to have an acuity of 20/40 (see Chapter 4, questions 1–15).
 Visual fields: Their assessment can localize damage anywhere from the retina to the occipital lobes, resulting in loss of vision of only a discrete area (or field). The best way to detect visual cuts is by confrontation: place yourself head-to-head and eye-to-eye with the patient, while both of you occlude the opposite eye (because while looking into each other’s eyes, both you and the patient have the same peripheral vision). To determine whether the patient can see what you see, move objects into his/her peripheral vision, starting from above, then below, then left and right. Patients should be able to see the objects at the same time you do. If they cannot, they probably have a visual cut corresponding to a particular region of peripheral vision (see Chapter 4, questions 20–35).
Visual fields: Their assessment can localize damage anywhere from the retina to the occipital lobes, resulting in loss of vision of only a discrete area (or field). The best way to detect visual cuts is by confrontation: place yourself head-to-head and eye-to-eye with the patient, while both of you occlude the opposite eye (because while looking into each other’s eyes, both you and the patient have the same peripheral vision). To determine whether the patient can see what you see, move objects into his/her peripheral vision, starting from above, then below, then left and right. Patients should be able to see the objects at the same time you do. If they cannot, they probably have a visual cut corresponding to a particular region of peripheral vision (see Chapter 4, questions 20–35).
37 How do you test CN III, IV, and VI?
Together, since oculomotor (III), trochlear (IV), and abducens (VI) work in concert to produce the various eye movements. To test them, ask patients to hold the head stationary while following your finger as it moves through the main directions of gaze: left-up, left-middle, left-down, and right-up, right-middle, and right-down. Normal eyes move symmetrically and smoothly. Any restriction or double vision (from inability of the eyes to move together) suggests damage to III, IV, or VI (see Chapter 4, questions 84–90).
38 What abnormal eye movements result from damage to CN III, IV, or VI?
 The oculomotor supplies medial, superior, and inferior rectus; inferior oblique; and levator palpebrae (which raises the eyelid). It also contains parasympathetic fibers that constrict the pupil. Hence, its lesions result in a partially abducted eye that is difficult to adduct, raise, or lower. In fact, it is frequently turned out (exotropia). There also is a drooping eyelid (ptosis) and a pupil that may be larger (mydriatic) and difficult to constrict. In more subtle cases, there may only be diplopia or blurred vision. A CN III palsy that spares the pupils (i.e., ptosis, and external rotation of the globe, but symmetric and equally reactive pupils) suggests diabetes, but also vasculitides and multiple sclerosis.
The oculomotor supplies medial, superior, and inferior rectus; inferior oblique; and levator palpebrae (which raises the eyelid). It also contains parasympathetic fibers that constrict the pupil. Hence, its lesions result in a partially abducted eye that is difficult to adduct, raise, or lower. In fact, it is frequently turned out (exotropia). There also is a drooping eyelid (ptosis) and a pupil that may be larger (mydriatic) and difficult to constrict. In more subtle cases, there may only be diplopia or blurred vision. A CN III palsy that spares the pupils (i.e., ptosis, and external rotation of the globe, but symmetric and equally reactive pupils) suggests diabetes, but also vasculitides and multiple sclerosis.
 The trochlear supplies the superior oblique muscle by extending over a trochlea, or pulley. Since this nerve allows us to view the tip of our nose, its lesion will result in an eye that cannot be depressed when adducted. Hence, whenever patients pull their eyes inward (toward the nose), they will be unable to move them downward. This is often subtle. An isolated right superior oblique paralysis results in (1) exotropia to the right (R); (2) double vision that worsens when looking to the left (L); and (3) head tilt to the right (R). The mnemonic is R, L, R (the marching rule—conversely, the rule for left superior oblique paralysis is L, R, L). This rule and the lack of ptosis and/or mydriasis differentiate the exotropia of CN IV palsy from that of CN III.
The trochlear supplies the superior oblique muscle by extending over a trochlea, or pulley. Since this nerve allows us to view the tip of our nose, its lesion will result in an eye that cannot be depressed when adducted. Hence, whenever patients pull their eyes inward (toward the nose), they will be unable to move them downward. This is often subtle. An isolated right superior oblique paralysis results in (1) exotropia to the right (R); (2) double vision that worsens when looking to the left (L); and (3) head tilt to the right (R). The mnemonic is R, L, R (the marching rule—conversely, the rule for left superior oblique paralysis is L, R, L). This rule and the lack of ptosis and/or mydriasis differentiate the exotropia of CN IV palsy from that of CN III.
 id=”u0300″/>The abducens supplies the lateral rectus. Hence, its damage prevents eye abduction to the side of the lesion. This results in double vision on horizontal gaze only (horizontal homonymous diplopia). It is often injured in patients with increased intracranial pressure.
id=”u0300″/>The abducens supplies the lateral rectus. Hence, its damage prevents eye abduction to the side of the lesion. This results in double vision on horizontal gaze only (horizontal homonymous diplopia). It is often injured in patients with increased intracranial pressure.
39 How do you test CN V (trigeminal nerve)?
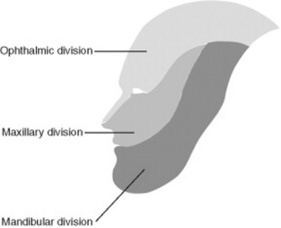
It depends on whether you are testing a motor or sensory component. The divisions of the trigeminal nerve are shown in Figure 19-1.
 The sensory component is predominant, providing pain, tactile, and thermic sensations to the face. Note that sensation to the tragus, most of the external ear, and angle of the jaw is not trigeminal and thus is preserved in diseases of the V (it is supplied instead by cervical sensory roots).
The sensory component is predominant, providing pain, tactile, and thermic sensations to the face. Note that sensation to the tragus, most of the external ear, and angle of the jaw is not trigeminal and thus is preserved in diseases of the V (it is supplied instead by cervical sensory roots).
 The motor component is smaller and primarily involved in chewing. It travels along the mandibular branch of the V and controls the masseters and lateral pterygoids. If damaged, it causes deviation of the jaw to the paralyzed side when attempting to open the mouth.
The motor component is smaller and primarily involved in chewing. It travels along the mandibular branch of the V and controls the masseters and lateral pterygoids. If damaged, it causes deviation of the jaw to the paralyzed side when attempting to open the mouth.
40 Where are the sensory and motor nuclei of the trigeminal nerve?
They are both in the pons. Yet the sensory also extends into the cervical cord.
41 How do you test the sensory function of CN V?
By pinprick or light touch over the areas of distribution of the trigeminal branches: upper (supplied by V1, or ophthalmic; forehead), mid (V2, or maxillary; cheek), and lower (V3, or mandibular; jaw). Sensory function of the ophthalmic branch is also tested by the corneal reflex (see question 58).
42 How do you test the motor function of CN V?
By feeling the masseters during teeth clinching. Contraction must be strong and symmetric.
45 What is the significance of a sensory deficit of the trigeminal nerve?
It depends on whether it involves both the face and body, or only the face:
 Isolated facial anesthesia suggests disease of the temporal bone or metastatic spread to the ipsilateral mandible and skull base. This presents with numbness to the chin and lower lip (“numb/chin syndrome”).
Isolated facial anesthesia suggests disease of the temporal bone or metastatic spread to the ipsilateral mandible and skull base. This presents with numbness to the chin and lower lip (“numb/chin syndrome”).
 Combined facial and body anesthesia suggests hemispheric and thalamic involvement, typically cerebrovascular. This presents with numbness to the same side of face and body (and contralateral to the ischemic area), plus hemiparesis and aphasia. Conversely, patients with facial numbness to one side and body numbness to the opposite have a brain stem lesion.
Combined facial and body anesthesia suggests hemispheric and thalamic involvement, typically cerebrovascular. This presents with numbness to the same side of face and body (and contralateral to the ischemic area), plus hemiparesis and aphasia. Conversely, patients with facial numbness to one side and body numbness to the opposite have a brain stem lesion.
47 What is the jaw-jerk reflex?
A reflex that tests the integrity of sensory (afferent) and motor (efferent) components of the V. To test for it, place your index finger (or tongue depressor) over the patients’ chin, while asking them to keep their mouth slightly open. Then, gently tap the index finger with your reflex hammer. Abnormal responses include jaw deviation or brisk closure. Exaggerated masseteric contraction, often with clonus, suggests upper motor neuron pathology (i.e., above the trigeminal nucleus in the mid-pons). This occurs in 70% of pseudobulbar palsy patients (see below, question 65).
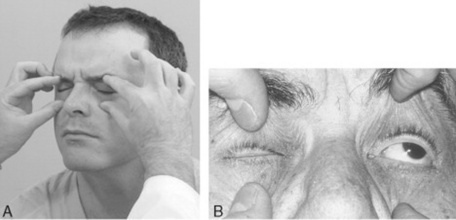
48 How do you test CN VII (facial nerve)?
Through the muscles of facial expression. Damage to CN VII causes inability to wrinkle the forehead, tightly close the eye (Fig. 19-2), or smile. It also causes facial asymmetry (i.e., ipsilateral widening of the palpebral fissure and sagging of the nasolabial fold).
60 How do you test CN VIII (acoustic/vestibular nerve)?
It depends on the function you want to test, vestibular or auditory:
 Vestibular function should be assessed by the Romberg, positional vertigo, and caloric irrigation tests only in cases of vertigo and dizziness.
Vestibular function should be assessed by the Romberg, positional vertigo, and caloric irrigation tests only in cases of vertigo and dizziness.
 Auditory function may instead be compromised in very subtle ways. Hence, the need for routine testing. This can be simply done by asking patients if they can hear whispered words, the soft noise of a ticking watch, or fingers rubbing against each other near the ear. Conductive and sensorineural hearing loss can be separated by Rinne and Weber tests (see Chapter 5, questions 59–65).
Auditory function may instead be compromised in very subtle ways. Hence, the need for routine testing. This can be simply done by asking patients if they can hear whispered words, the soft noise of a ticking watch, or fingers rubbing against each other near the ear. Conductive and sensorineural hearing loss can be separated by Rinne and Weber tests (see Chapter 5, questions 59–65).
64 What is the anatomy of CN IX (glossopharyngeal) and CN X (vagus)? How do you test them?
Axons from several brain stem nuclei mingle together to emerge from the neuraxis through two separate nerves, named by early neuroanatomists as glossopharyngeal (IX) and vagal (X) (the vagus was so termed since, as a vagabond, it wanders long distances in the body). In reality, the origin of the two nerves is essentially identical. Function also is similar: motor control of the palate and pharynx (plus, for the IX, sensory supply to the pharynx and posterior third of the tongue). Hence, their clinical testing is not entirely separable. Since the brain stem nuclei of these two nerves receive bilateral innervation from the cortex, their dysfunction results from one of three possibilities: (1) bilateral damage to the cortex or pyramidal tracts (pseudobulbar palsy), (2) brain stem disease (lateral medullary syndrome), or (3) peripheral nerve lesions (jugular foramen syndrome). You can test IX and X by asking patients to say “ahhh” or “ehhh” (see Chapter 6, questions 53 and 54) while observing whether the velum of the palate rises symmetrically. Alternatively, you can use the gag and palatal reflexes. The latter is elicited by touching the patient’s palate with a cotton swab, which causes elevation of the soft palate and ipsilateral deviation of the uvula. The gag is instead triggered by touching the posterior wall of the pharynx (or alternatively, the tonsillar area or base of the tongue). It causes tongue retraction and elevation/constriction of the pharyngeal musculature. In unilateral CN IX and X paralysis, these reflexes result in deviation of the uvula toward the normal side. Lesions of the IX also will result in loss of taste in the posterior third of the tongue, and loss of pain and touch sensations in the same area plus the soft palate and pharyngeal walls. Conversely, unilateral paralysis of CN X’s recurrent laryngeal nerve will cause hoarseness. Bilateral paralysis will cause stridor (requiring tracheostomy).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree