Chapter 21 The Musculoskeletal System
Generalities
This is a difficult area of physical exam, but one necessary in ambulatory medicine and often rewarding. One of 10 patients presenting to a primary care office will do so because of musculoskeletal complaints. Most of these can be diagnosed through a thorough exam, specific maneuvers (Table 21-1), and a proper knowledge of joints’ anatomy and physiology.
Table 21-1 Joint Diseases—Specific Maneuvers
| Joint | Problem | Maneuver |
|---|---|---|
| Shoulder | General | Painful arc sign |
| Acromioclavicular (AC) arthritis | Cross-body and cross-arm maneuvers | |
| Bicipital tendinitis | Yergason’s and Speed’s tests | |
| Rotator cuff pathology | Gerber’s lift-off test, drop arm test, empty can test | |
| Impingement | Neer (impingement) and Hawkins-Kennedy tests | |
| Anterior shoulder instability | Apprehension and Jobe’s relocation tests | |
| Inferior shoulder instability | Sulcus sign | |
| Glenoid labral tears | O’Brien’s and anterior slide tests | |
| Elbow | Cubital tunnel syndrome | Elbow flexion test |
| Wrist | Carpal tunnel syndrome | Tinel’s sign, Phalen’s sign, flick sign |
| Rheumatoid arthritis | Piano key sign | |
| De Quervain’s tendinitis | Finkelstein test (positive) | |
| Intersection syndrome | Finkelstein test (negative) | |
| Hand | Interosseous tightness versus capsular contraction | Bunnel-Littler test |
| Hip | General | FABER maneuver |
| Knee | Patellofemoral syndrome | Patellofemoral grinding test |
| Effusion | Bulge sign, patellar ballottement, fluid wave test | |
| Anterior cruciate ligament | Lachman’s test, anterior drawer test, lateral pivot shift test | |
| Posterior cruciate ligament | Posterior drawer test, tibial sag test | |
| Meniscal tears | Medial-lateral grind test, McMurray’s test, Apley’s grind and distraction test | |
| Ankle | Anterior talofibular tear | Anterior drawer test |
| Anterior talofibular/calcaneofibular tear | “Talar tilt” test | |
| Tibiofibular syndesmosis | “Squeeze” test | |
| Tarsal tunnel syndrome | Submalleolar tap |
8 What is the significance of articular warmth and erythema (calor and rubor)?
They indicate pathology, too. Normal joints should be cooler than the surroundings and not red.
A. The Shoulder
15 Describe the muscles and tendons of the shoulder
 The rotator cuff consists of four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis (mnemonic, SITS). Their tendons converge on the humerus, thus allowing for most of the joint movements (abduction of the arm and rotation of the shoulder, both internal and external). They also hold the humeral head in the glenoid cavity, thus stabilizing the joint.
The rotator cuff consists of four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis (mnemonic, SITS). Their tendons converge on the humerus, thus allowing for most of the joint movements (abduction of the arm and rotation of the shoulder, both internal and external). They also hold the humeral head in the glenoid cavity, thus stabilizing the joint.
 The deltoid is the largest and strongest muscle, responsible for the later part of abduction and flexion once the arm has been lifted by the supraspinatus. It is visible but rarely injured.
The deltoid is the largest and strongest muscle, responsible for the later part of abduction and flexion once the arm has been lifted by the supraspinatus. It is visible but rarely injured.
 The biceps has two proximal heads (hence, the name), which insert into the shoulder: (1) the long head tendon and (2) the short head of the biceps. The long head tendon lies in the bicipital groove of the humerus, between the greater and lesser tuberosities and under the transverse humeral ligament. This arrangement prevents the humeral head from sliding too far during abduction and external rotation. At the upper end of the groove, the long head of the biceps angles 90 degrees inward, crossing the humeral head and eventually inserting itself into the upper edge of the glenoid labrum and supraglenoid tubercle. The short head of the biceps connects instead on the coracoid process. Distally, the two heads of the biceps merge to form the body of the biceps brachii muscle, which inserts itself into the radius through its common distal head. The biceps is a powerful flexor and supinator of the forearm (i.e., it rotates forearm and hand so that the palm faces upward).
The biceps has two proximal heads (hence, the name), which insert into the shoulder: (1) the long head tendon and (2) the short head of the biceps. The long head tendon lies in the bicipital groove of the humerus, between the greater and lesser tuberosities and under the transverse humeral ligament. This arrangement prevents the humeral head from sliding too far during abduction and external rotation. At the upper end of the groove, the long head of the biceps angles 90 degrees inward, crossing the humeral head and eventually inserting itself into the upper edge of the glenoid labrum and supraglenoid tubercle. The short head of the biceps connects instead on the coracoid process. Distally, the two heads of the biceps merge to form the body of the biceps brachii muscle, which inserts itself into the radius through its common distal head. The biceps is a powerful flexor and supinator of the forearm (i.e., it rotates forearm and hand so that the palm faces upward).
16 What are the shoulder’s movements? How do you test its ROM?
 Abduction: Ask patients to raise the arms laterally and away from the body: first, to the level of the shoulder and with palms facing down (90 degrees of glenohumeral motion), and then above the head and with palms facing each other (another 90 degrees, of which 60 degrees are scapulothoracic motion and 30 degrees are combined glenohumeral and scapulothoracic). Normal individuals should complete a smooth 180-degree arc. Average, however, is a little less (150 degrees).
Abduction: Ask patients to raise the arms laterally and away from the body: first, to the level of the shoulder and with palms facing down (90 degrees of glenohumeral motion), and then above the head and with palms facing each other (another 90 degrees, of which 60 degrees are scapulothoracic motion and 30 degrees are combined glenohumeral and scapulothoracic). Normal individuals should complete a smooth 180-degree arc. Average, however, is a little less (150 degrees).
 Abduction and external rotation: Ask patients to place the hand behind the head, trying to reach as far down into the spine as possible. Normal individuals should reach C7. Average range of external rotation with the arm in abduction is 70–90 degrees.
Abduction and external rotation: Ask patients to place the hand behind the head, trying to reach as far down into the spine as possible. Normal individuals should reach C7. Average range of external rotation with the arm in abduction is 70–90 degrees.
 Adduction and internal rotation: Ask patients to place the hand behind the back, trying to reach with the thumb as far up into the scapula and spine as possible (Apley’s scratch test). Normal adduction is 45 degrees; normal range of internal rotation is above T8 (i.e., the lower border of the scapula and the T7 level).
Adduction and internal rotation: Ask patients to place the hand behind the back, trying to reach with the thumb as far up into the scapula and spine as possible (Apley’s scratch test). Normal adduction is 45 degrees; normal range of internal rotation is above T8 (i.e., the lower border of the scapula and the T7 level).
 Forward flexion: Ask patients to trace an arc forward while keeping the elbow straight, ultimately raising the hands above the head as in the “Heil Hitler” sign. Normal range is 0–180 degrees.
Forward flexion: Ask patients to trace an arc forward while keeping the elbow straight, ultimately raising the hands above the head as in the “Heil Hitler” sign. Normal range is 0–180 degrees.
 Extension: Ask patients to trace an arc backwards, with the elbow straight, arms at the side, and palms facing each other. Normal subjects should place the hand behind their back to 40–50 degrees.
Extension: Ask patients to trace an arc backwards, with the elbow straight, arms at the side, and palms facing each other. Normal subjects should place the hand behind their back to 40–50 degrees.
17 What areas of the shoulder girdle should be palpated?
 Acromioclavicular joint (top of shoulder, radiating toward the neck)
Acromioclavicular joint (top of shoulder, radiating toward the neck)
 Long head of the biceps tendon (anterior shoulder, in the bicipital groove)
Long head of the biceps tendon (anterior shoulder, in the bicipital groove)
 Coracoid process (anterior shoulder)
Coracoid process (anterior shoulder)
 Rotator cuff (lateral aspect of shoulder, radiating toward the deltoid insertion)
Rotator cuff (lateral aspect of shoulder, radiating toward the deltoid insertion)
19 What is the general approach to the shoulder exam?
1. Inspect for scars, color, edema, deformities, muscle atrophy, asymmetry, and guarding.
2. Palpate for pain or point tenderness (the presence of either narrows the exam):
 Bony and soft-tissue structures, such as coracoid process, acromioclavicular joint, greater tubercle
Bony and soft-tissue structures, such as coracoid process, acromioclavicular joint, greater tubercle3. Assess active and passive ROM, especially in regard to elicited pain and reduced movement.
4. Determine muscle strength. This is an essential part of the exam, and comparing side to side may help you locate the area of concern. Always carry it out with and without resistance. To isolate the various muscles, use the following maneuvers:
 Supraspinatus: arm forward 90 degrees in the scapular plane and forearm pronated (thumbs down, “empty can” maneuver). Drooping of this position suggests full-thickness rotator cuff tears.
Supraspinatus: arm forward 90 degrees in the scapular plane and forearm pronated (thumbs down, “empty can” maneuver). Drooping of this position suggests full-thickness rotator cuff tears. Subscapularis is tested by internal rotation. Arm is rotated internally with the dorsum against the buttock. Actively lift the hand from the buttocks against resistance.
Subscapularis is tested by internal rotation. Arm is rotated internally with the dorsum against the buttock. Actively lift the hand from the buttocks against resistance. External rotators, teres minor, and infraspinatus are primarily tested by external rotation (arm on the side and in 90 degrees of abduction).
External rotators, teres minor, and infraspinatus are primarily tested by external rotation (arm on the side and in 90 degrees of abduction).20 What is the shoulder pad sign?
A sign of bilateral shoulder effusions. Very typical of amyloidosis.
21 What are the most common musculoskeletal causes of shoulder pain?
 Impingement (with its complications of tendinitis and rotator cuff tears)
Impingement (with its complications of tendinitis and rotator cuff tears)
 Dislocated or unstable shoulder
Dislocated or unstable shoulder
Hence the mnemonic, “Basically I Test Religiously For Damaged Objects.”
23 In addition to history, how else do you identify referred shoulder pain?
By its being typically nondescript, poorly localized, and not reproducible on shoulder exam.
28 What are the symptoms/findings of bicipital tendinitis?
Achy anterior shoulder pain, worsened by overhead activity, lifting of heavy objects, and elevated pushing/pulling. Rest is usually beneficial, whereas flexion of the elbow against resistance is detrimental. Pain is vague, though at times it may become localized to the anterior humerus. On exam, there is point tenderness over the bicipital groove, which is the area where the long tendon is anatomically exposed. This lies 3 inches below the anterior acromion and may be best localized by holding the arm in 10 degrees of external rotation. Pain also can be elicited by passive abduction of the arm in a painful arc maneuver (see question 41), which is typical of impingement syndrome, although at times it also may be positive in patients with isolated biceps tendinitis.
29 Which specific maneuvers can reproduce the pain of bicipital tendinitis?
Maneuvers that resist the normal function of the biceps—supination and flexion of the forearm:
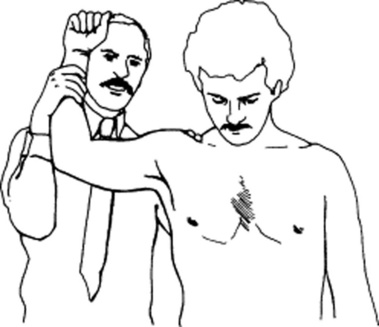
 Yergason’s test: The hand is pronated, the elbow flexed to 90 degrees, and the shoulder in adduction (i.e., arm against the body). With the patient attempting supination of the forearm (i.e., palm up), you resist with one hand while with the other you press on the bicipital tendon. The test is positive when it elicits pain and tenderness over the bicipital groove.
Yergason’s test: The hand is pronated, the elbow flexed to 90 degrees, and the shoulder in adduction (i.e., arm against the body). With the patient attempting supination of the forearm (i.e., palm up), you resist with one hand while with the other you press on the bicipital tendon. The test is positive when it elicits pain and tenderness over the bicipital groove.
 Speed’s test: Dr. Speed actually never described this maneuver. It was first reported by Crenshaw and Kilgore in 1966, quoting “personal communication” as their source. It is performed by having the patient attempt to flex the affected arm against resistance, after positioning it with elbow extended and forearm in supination (i.e., palm up). Once again, you resist with one hand while you press with the other on the bicipital tendon. The test is positive when it elicits pain over the bicipital groove. As validated by arthroscopy, it has a 14% specificity, 90% sensitivity, 23% positive predictive value, and 83% negative predictive value.
Speed’s test: Dr. Speed actually never described this maneuver. It was first reported by Crenshaw and Kilgore in 1966, quoting “personal communication” as their source. It is performed by having the patient attempt to flex the affected arm against resistance, after positioning it with elbow extended and forearm in supination (i.e., palm up). Once again, you resist with one hand while you press with the other on the bicipital tendon. The test is positive when it elicits pain over the bicipital groove. As validated by arthroscopy, it has a 14% specificity, 90% sensitivity, 23% positive predictive value, and 83% negative predictive value.
33 How do you diagnose rotator cuff tendinitis?
 The supraspinatus is the most important and most commonly damaged of the four. It links the top of the scapula to the humerus, inserting into its greater tuberosity. It is partially responsible for arm abduction (the initial 15–30 degrees are actually produced by the deltoid, the next 60 degrees by the supraspinatus, and the final 90 degrees by the deltoid again). Hence, inflammation of the supraspinatus tendon leads to pain at 30–90 degrees of abduction, as the humerus impinges the tendon against the acromion. It can be easily tested through the empty can test.
The supraspinatus is the most important and most commonly damaged of the four. It links the top of the scapula to the humerus, inserting into its greater tuberosity. It is partially responsible for arm abduction (the initial 15–30 degrees are actually produced by the deltoid, the next 60 degrees by the supraspinatus, and the final 90 degrees by the deltoid again). Hence, inflammation of the supraspinatus tendon leads to pain at 30–90 degrees of abduction, as the humerus impinges the tendon against the acromion. It can be easily tested through the empty can test.
 The infraspinatus produces external rotation of the humerus, a function assisted by the teres minor. The two also cooperate to maintain glenohumeral stability. To test external rotators (infraspinatus and teres minor): (1) have the patient abduct both shoulders to 20–30 degrees, while keeping the elbows flexed at 90 degrees; (2) instruct the patient to push the arms outward (externally rotate) against resistance. External rotation elicits pain in tendinitis and weakness in tears.
The infraspinatus produces external rotation of the humerus, a function assisted by the teres minor. The two also cooperate to maintain glenohumeral stability. To test external rotators (infraspinatus and teres minor): (1) have the patient abduct both shoulders to 20–30 degrees, while keeping the elbows flexed at 90 degrees; (2) instruct the patient to push the arms outward (externally rotate) against resistance. External rotation elicits pain in tendinitis and weakness in tears.
 The subscapularis is the only of the four rotator muscles to originate from the anterior surface of the scapula (the others arise instead in the back). It connects the scapula to the humerus, serving as humeral head depressor and, in certain shoulder positions (adduction), as internal rotator. Function is evaluated through the “Gerber’s lift-off test”: (1) have patients place the hand behind the back, with palm facing out, and (2) instruct them to lift the hand away from the back and against resistance. Internal rotation elicits pain in tendinitis and weakness in tears.
The subscapularis is the only of the four rotator muscles to originate from the anterior surface of the scapula (the others arise instead in the back). It connects the scapula to the humerus, serving as humeral head depressor and, in certain shoulder positions (adduction), as internal rotator. Function is evaluated through the “Gerber’s lift-off test”: (1) have patients place the hand behind the back, with palm facing out, and (2) instruct them to lift the hand away from the back and against resistance. Internal rotation elicits pain in tendinitis and weakness in tears.
Note that given the anatomic closeness of the long head tendon of the biceps (which passes down the bicipital groove in a fibrous sheath between the subscapularis and supraspinatus tendons), patients with rotator cuff disease also may have biceps tendinitis (see questions 27 and 28).
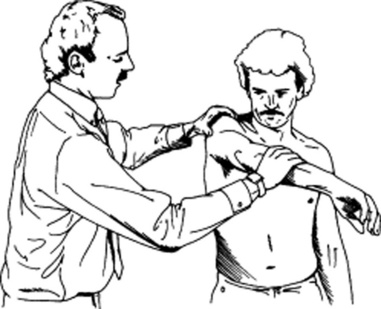
38 How do you perform the Neer (impingement) test?
The patient’s forearm is internally rotated, so that the thumb points downward. While standing behind the patient, place one hand on the patient’s scapula and with the other hand grasp the forearm and forward flex it, eventually positioning the patient’s hand over the head. Forced elevation and internal rotation of the arm cause the greater tuberosity of the humerus to compress the subacromial bursa. This, in turn, squeezes the supraspinatus tendon against the acromion, causing pain in cases of impingement. The test also can differentiate AC arthritis from subacromial bursitis (Fig. 21-1).
49 How do you test for glenohumeral instability?
It depends on the type of instability: anterior versus inferior.
50 How do you test for anterior shoulder instability?
Through the apprehension and Jobe’s relocation tests. Start with “apprehension” (Fig. 21-2). To perform it, ask patients to lie supine, with the affected shoulder just off the examining table. Grasp the elbow with one hand, and gently bring the arm to 90-degree abduction and 90-degree external rotation. Then push with your other hand on the posterior aspect of the humeral head, from back to front. Anterior shoulder instability will give a feeling that the arm is about to pop out of the joint. At the same time, patients will experience pain, apprehension, and guarding. In the original series of Rowe and Zarins, all 60 cases of anterior shoulder instability had a positive apprehension test. If the patient experiences pain and/or apprehension, move on to the second part of the maneuver: the Jobe’s relocation test. This is performed in the same position, but this time by pushing on the anterior aspect of the humeral head, from front to back, as if relocating a glenohumeral joint that had been partially dislocated by the apprehension test. Patients with primary impingement will have no change in pain, whereas those with anterior instability (subluxation) and secondary impingement will have relief of pain and/or apprehension. When relying primarily on relief of apprehension, the relocation test has sensitivity for anterior instability of 68%; specificity, 100%; positive predictive value, 100%; negative predictive value, 78%; and accuracy, 85%.
57 What is the mechanism of adhesive capsulitis?
Inflammation, which “glues” the capsule and surrounding structures into a frozen shoulder.
B. The Elbow
62 What do valgus and varus mean?
This is a very confusing terminology. In orthopedics, valgus indicates an outward angulation of the “distal segment” of a bone or joint, so that it is “twisted away” (i.e., away from the body, or midline of the limb). Conversely, varus indicates its inward angulation (so that it is now twisted toward the body, or midline of the limb). Note that both terms always refer to the direction in which the distal segment of the joint (or bone) is pointing. In fact, when referred to as a bone, the bone itself is considered to be the distal segment of the joint. Hence, a varus or valgus deformity of the forearm refers to the arm/forearm joint (the elbow) and not to the wrist. Having said that, a normal elbow is in valgus, because with the joint fully extended (and the palms facing upward) the distal segment of the forearm will point away from the body (or midline of the limb). If you think this is confusing, wait until you see how it applies to the knee exam (see question 213).
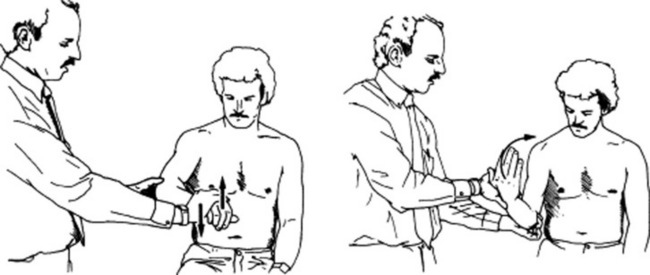
68 What is “golfer’s elbow” (medial epicondylitis)?
An overuse injury to the proximal attachment of the flexor/pronator muscles of the forearm, commonly seen in the dominant elbow of a golfer. Its mechanism is similar to that of lateral epicondylitis, but less common since wrist flexors are stronger and less likely overstressed (see Fig. 21-3).
C. The Wrist
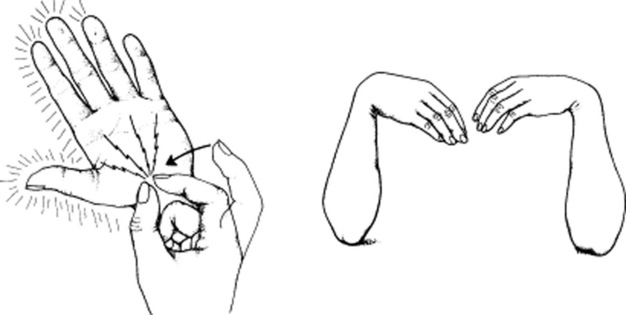
84 What is the physical exam of CTS?
Once the appropriate history is obtained, two maneuvers are typically carried out: Tinel’s sign and Phalen’s sign (first described by the American orthopedist George S. Phalen, 1911–1998) (see Fig. 21-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree