Chapter 16
The musculoskeletal system
The musculoskeletal system consists of the bones of the skeleton, their joints and the skeletal (voluntary) muscles that move the body. The characteristics and properties of joints, and of bone and muscle tissue, are discussed in this chapter. The effects of ageing on the musculoskeletal system are listed, and the illnesses section at the end of the chapter describes some disorders of bone, muscle and joints.
Bone
Although bones are often thought to be static or permanent, they are highly vascular living structures that are continuously being remodelled.
Functions of bones
The functions of bones include:
• providing the body framework
• giving attachment to muscles and tendons
• haemopoiesis, the production of blood cells in red bone marrow (p. 64)
Types of bones
Bones are classified as long, short, irregular, flat and sesamoid.
Long bones.
These consist of a shaft and two extremities. As the name suggests, these bones are longer than they are wide. Most long bones are found in the limbs; examples include the femur, tibia and fibula.
Short, irregular, flat and sesamoid bones.
These have no shafts or extremities and are diverse in shape and size. Examples include:
• short bones – carpals (wrist)
• irregular bones – vertebrae and some skull bones
• flat bones – sternum, ribs and most skull bones
Bone structure
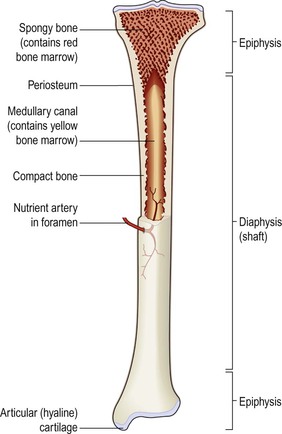
Long bones
These have a diaphysis (shaft) and two epiphyses (extremities) (Fig. 16.1). The diaphysis is composed mainly of compact bone with a central medullary canal, containing fatty yellow bone marrow. The epiphyses consist of an outer covering of compact bone with spongy (cancellous) bone inside. The diaphysis and epiphyses are separated by epiphyseal cartilages, which ossify when growth is complete.
Long bones are almost completely covered by a vascular membrane, the periosteum, which has two layers. The outer layer is tough and fibrous, and protects the bone underneath. The inner layer contains osteoblasts and osteoclasts, the cells responsible for bone production and breakdown (see below), and is important in repair and remodelling of the bone. The periosteum covers the whole bone except within joint cavities, allows attachments of tendons and is continuous with the joint capsule. Hyaline cartilage replaces periosteum on bone surfaces that form joints. Thickening of a bone occurs by the deposition of new bone tissue under the periosteum.
Blood and nerve supply
One or more nutrient arteries supply the bone shaft; the epiphyses have their own blood supply, although in the mature bone the capillary networks arising from the two are heavily interconnected. The sensory nerve supply usually enters the bone at the same site as the nutrient artery, and branches extensively throughout the bone. Bone injury is, therefore, usually very painful.
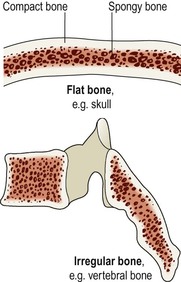
Short, irregular, flat and sesamoid bones
These have a relatively thin outer layer of compact bone, with spongy bone inside containing red bone marrow (Fig. 16.2). They are enclosed by periosteum except the inner layer of the cranial bones where it is replaced by dura mater.
Microscopic structure of bone
Bone is a strong and durable type of connective tissue. Its major constituent (65%) is a mixture of calcium salts, mainly calcium phosphate. This inorganic matrix gives bone great hardness, but on its own would be brittle and prone to shattering. The remaining third is organic material, called osteoid, which is composed mainly of collagen. Collagen is very strong and gives bone slight flexibility. The cellular component of bone contributes less than 2% of bone mass.
Bone cells
There are three types of bone cell:
Osteoblasts
These bone-forming cells are responsible for the deposition of both inorganic salts and osteoid in bone tissue. They are therefore present at sites where bone is growing, repairing or remodelling, e.g.:
• in the deeper layers of periosteum
• in the centres of ossification of immature bone
• at the ends of the diaphysis adjacent to the epiphyseal cartilages of long bones
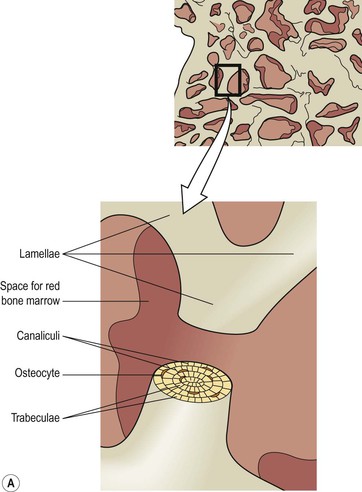
As they deposit new bone tissue around themselves, they eventually become trapped in tiny pockets (lacunae, Fig. 16.3) in the growing bone, and differentiate into osteocytes.
Osteocytes
These are mature bone cells that monitor and maintain bone tissue, and are nourished by tissue fluid in the canaliculi that radiate from the central canals.
Osteoclasts
These cells break down bone, releasing calcium and phosphate. They are very large cells with up to 50 nuclei, which have formed from the fusion of many monocytes (p. 69). The continuous remodelling of healthy bone tissue is the result of balanced activity of the bone’s osteoblast and osteoclast populations. Osteoclasts are found in areas of the bone where there is active growth, repair or remodelling, e.g.:
• under the periosteum, maintaining bone shape during growth and to remove excess callus formed during healing of fractures (p. 394)
• round the walls of the medullary canal during growth and to canalise callus during healing.
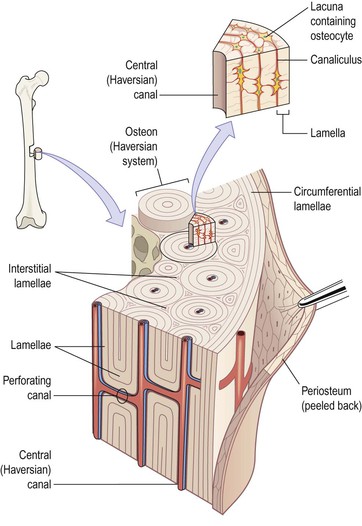
Compact (cortical) bone
Compact bone makes up about 80% of the body bone mass. It is made up of a large number of parallel tube-shaped units called osteons (Haversian systems), each of which is made up of a central canal surrounded by a series of expanding rings, similar to the growth rings of a tree (Fig. 16.3). Osteons tend to be aligned the same way that force is applied to the bone, so for example in the femur (thigh bone), they run from one epiphysis to the other. This gives the bone great strength.
The central canal contains nerves, lymphatics and blood vessels, and each central canal is linked with neighbouring canals by tunnels running at right angles between them, called perforating canals. The series of cylindrical plates of bone arranged around each central canal are called lamellae. Between the adjacent lamellae of the osteon are strings of little cavities called lacunae, in each of which sits an osteocyte. Lacunae communicate with each other through a series of tiny channels called canaliculi, which allows the circulation of interstitial fluid through the bone, and direct contact between the osteocytes, which extend fine processes into them (Fig. 16.4).
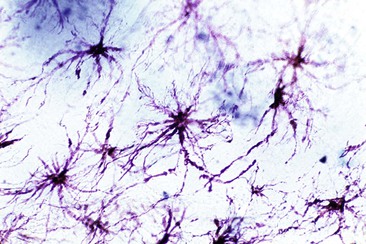
Figure 16.4 Light micrograph of osteocytes, showing the multiple fine processes that extend through bone canaliculi and allow each cell to communicate directly with its neighbours.
Between the osteons are interstitial lamellae, the remnants of older systems partially broken down during remodelling or growth of bone.
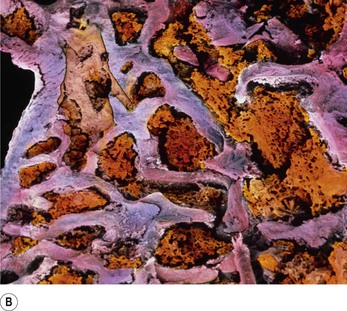
Spongy (cancellous, trabecular) bone
To the naked eye, spongy bone looks like a honeycomb. Microscopic examination reveals a framework formed from trabeculae (meaning ‘little beams’), which consist of a few lamellae and osteocytes interconnected by canaliculi (Fig. 16.5). Osteocytes are nourished by interstitial fluid diffusing into the bone through the tiny canaliculi. The spaces between the trabeculae contain red bone marrow. In addition, spongy bone is lighter than compact bone, reducing the weight of the skeleton.
Development of bone tissue  16.1
16.1
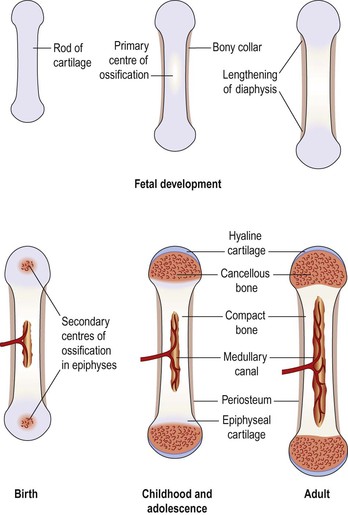
Also called osteogenesis or ossification, this begins before birth and is not complete until about the 21st year of life. Long, short and irregular bones develop in the fetus from rods of cartilage, cartilage models. Flat bones develop from membrane models and sesamoid bones from tendon models.
In mature bone, a fine balance of osteoblast and osteoclast activity maintains normal bone structure. If osteoclast activity exceeds osteoblast activity, the bone becomes weaker. On the other hand, if osteoblast activity outstrips osteoclast activity, the bone becomes stronger and heavier.
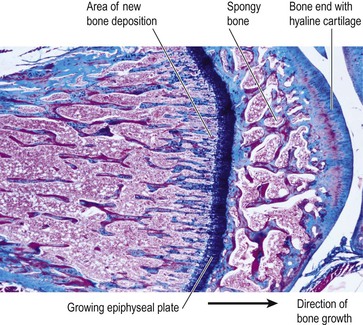
Development of long bones
In long bones the focal points from which ossification begins are small areas of osteogenic cells, or centres of ossification in the cartilage model (Fig. 16.6). This is accompanied by development of a bone collar at about 8 weeks of gestation. Later the blood supply develops and bone tissue replaces cartilage as osteoblasts secrete osteoid in the shaft. The bone lengthens as ossification continues and spreads to the epiphyses. Around birth, secondary centres of ossification develop in the epiphyses, and the medullary canal forms when osteoclasts break down the central bone tissue in the middle of the shaft. During childhood, long bones continue to lengthen because the epiphyseal plate at each end of the bone, which is made of cartilage, continues to produce new cartilage on its diaphyseal surface (the surface facing the shaft of the bone, Fig. 16.7). This cartilage is then turned to bone. As long as cartilage production matches the rate of ossification, the bone continues to lengthen. At puberty, under the influence of sex hormones, the epiphyseal plate growth slows down, and is overtaken by bone deposition. Once the whole epiphyseal plate is turned to bone, no further lengthening of the bone is possible.
Hormonal regulation of bone growth
Hormones (see Ch. 9) that regulate the growth, size and shape of bones include the following.
• Growth hormone and the thyroid hormones, thyroxine and tri-iodothyronine, are especially important during infancy and childhood; deficient or excessive secretion of these results in abnormal development of the skeleton (p. 223).
• Testosterone and oestrogens influence the physical changes that occur at puberty and help maintain bone structure throughout life. Rising levels of these hormones are responsible for the growth spurt of puberty, but later stimulate closure of the epiphyseal plates (Fig. 16.7), so that bone growth lengthways stops (although bones can grow in thickness throughout life). Average adult male height is usually greater than female, because male puberty tends to occur at a later age than female puberty, giving a male child’s bones longer to keep growing. Oestrogens are responsible for the wider female pelvis that develops during puberty, and for maintaining bone mass in the adult female. Falling oestrogen levels after menopause can put postmenopausal women at higher risk of bone fracture (osteoporosis, p. 431).
• Calcitonin and parathyroid hormone (p. 224) control blood levels of calcium by regulating its uptake into and release from bone. Calcitonin increases calcium uptake into bone (reducing blood calcium), and parathormone decreases it (increasing blood calcium).
Although the length and shape of bones does not normally change after ossification is complete, bone tissue is continually being remodelled and replaced when damaged. Osteoblasts continue to lay down osteoid and osteoclasts reabsorb it. The rate in different bones varies, e.g. the distal part of the femur is replaced over a period of 5 to 6 months.
Exercise and bone
Although bone growth lengthways permanently ceases once the epiphyseal plates have ossified, thickening of bone is possible throughout life. This involves the laying down of new osteons at the periphery of the bone through the action of osteoblasts in the inner layer of the periosteum. Weight-bearing exercise stimulates thickening of bone, strengthening it and making it less liable to fracture. Lack of exercise reverses these changes, leading to lighter, weaker bones.
Diet and bone
Healthy bone tissue requires adequate dietary calcium and vitamins A, C and D. Calcium, and smaller amounts of other minerals such as phosphate, iron and manganese, is essential for adequate mineralisation of bone. Vitamin A is needed for osteoblast activity. Vitamin C is used in collagen synthesis, and vitamin D is required for calcium and phosphate absorption from the intestinal tract.
Bone markings
Most bones have rough surfaces, raised protuberances and ridges that give attachment to muscle tendons and ligaments. These are not included in the following descriptions of individual bones unless they are of particular note, but many are marked on illustrations. Bone markings and related terminology are defined in Table 16.1.
Table 16.1
Anatomical terminology related to bones
| Term | Meaning |
| Articulating surface | The part of the bone that enters into the formation of a joint |
| Articulation | A joint between two or more bones |
| Bony sinus | A hollow cavity within a bone |
| Border | A ridge of bone separating two surfaces |
| Condyle | A smooth rounded projection of bone that forms part of a joint |
| Facet | A small, generally rather flat, articulating surface |
| Fissure or cleft | A narrow slit |
| Foramen (plural: foramina) | A hole in a structure |
| Fossa (plural: fossae) | A hollow or depression |
| Meatus | A tube-shaped cavity within a bone |
| Septum | A partition separating two cavities |
| Spine, spinous process or crest | A sharp ridge of bone |
| Styloid process | A sharp downward projection of bone that gives attachment to muscles and ligaments |
| Suture | An immovable joint, e.g. between the bones of the skull |
| Trochanter, tuberosity or tubercle | Roughened bony projections, usually for attachment of muscles or ligaments. The different names are used according to the size of the projection. Trochanters are the largest and tubercles the smallest |
Healing of bone  16.2
16.2
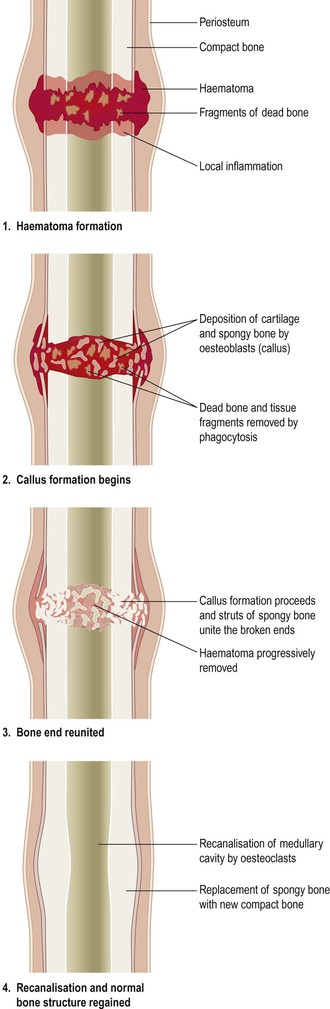
There are a number of terms used to classify bone fractures, including:
• simple: the bone ends do not protrude through the skin
• compound: the bone ends protrude through the skin
Following a fracture, the broken ends of bone are joined by the deposition of new bone. This occurs in several stages (Fig. 16.8).
2. There follows development of acute inflammation and accumulation of inflammatory exudate, containing macrophages that phagocytose the haematoma and small dead fragments of bone (this takes about 5 days). Fibroblasts migrate to the site; granulation tissue and new capillaries develop.
4. Reshaping of the bone continues and gradually the medullary canal is reopened through the callus (in weeks or months). In time the bone heals completely with the callus tissue completely replaced with mature compact bone. Often the bone is thicker and stronger at the repair site than originally, and a second fracture is more likely to occur at a different site.
Factors that delay healing of fractures
Tissue fragments between bone ends.
Splinters of dead bone (sequestrae) and soft tissue fragments not removed by phagocytosis delay healing.
Deficient blood supply.
This delays growth of granulation tissue and new blood vessels. Hypoxia also reduces the number of osteoblasts and increases the number of chondrocytes that develop from their common parent cells. This may lead to cartilaginous union of the fracture, which results in a weaker repair. The most vulnerable sites, because of their normally poor blood supply, are the neck of femur, the scaphoid and the shaft of tibia.
Poor alignment of bone ends.
This may result in the formation of a large and irregular callus that heals slowly and often results in permanent disability.
Continued mobility of bone ends.
Continuous movement results in fibrosis of the granulation tissue followed by fibrous union of the fracture.
Miscellaneous.
These include infection (see below), systemic illness, malnutrition, drugs, e.g. corticosteroids and ageing.
Complications of fractures
Infection (osteomyelitis, p. 432).
Pathogens enter through broken skin, although they may occasionally be blood-borne. Healing will not occur until the infection resolves.
Fat embolism.
Emboli consisting of fat from the bone marrow in the medullary canal may enter the circulation through torn veins. They are most likely to lodge in the lungs and block blood flow through the pulmonary capillaries.
Axial skeleton
The bones of the skeleton are divided into two groups: the axial skeleton and the appendicular skeleton (Fig. 16.9).
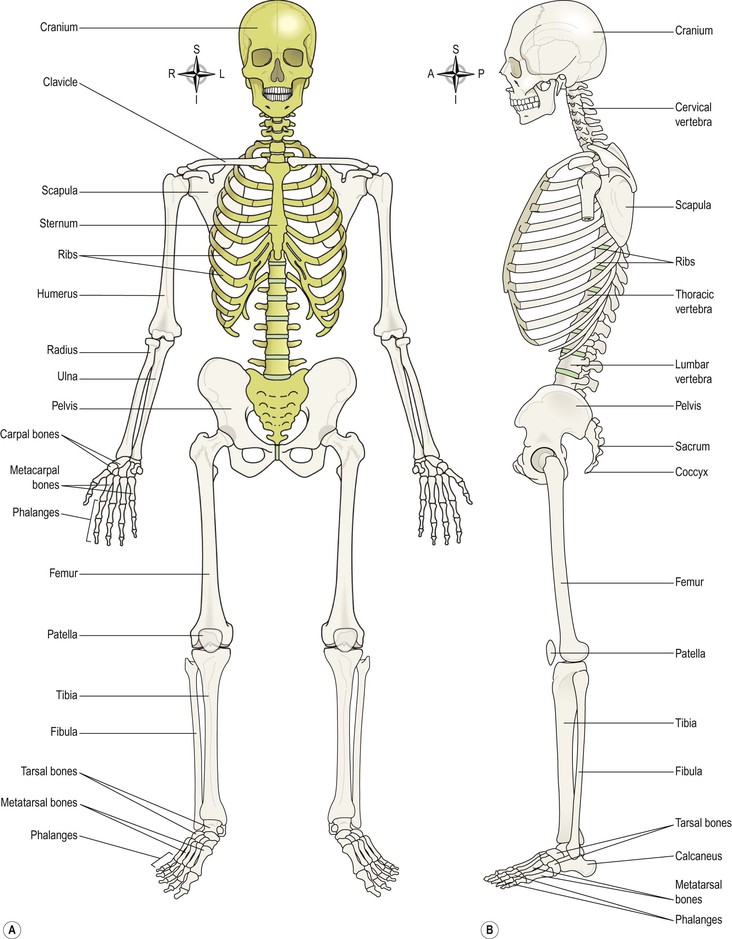
Figure 16.9 The skeleton. Axial skeleton in gold, appendicular skeleton in brown. A. Anterior view. B. Lateral view.
The axial skeleton consists of the skull, vertebral column, ribs and sternum. Together the bones forming these structures constitute the central bony core of the body, the axis. The appendicular skeleton consists of the shoulder and pelvic girdles and the limb bones.
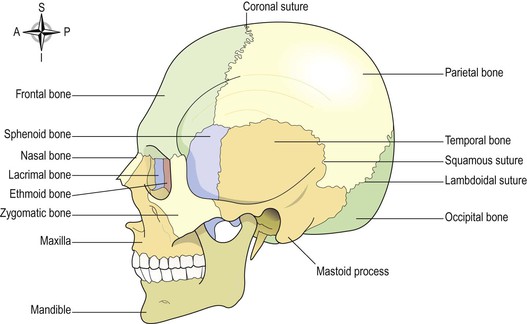
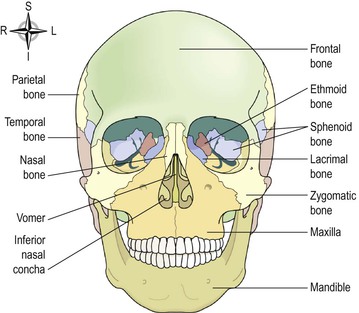
Skull (Figs 16.10 and 16.11)
The skull rests on the upper end of the vertebral column and its bony structure is divided into two parts: the cranium and the face.
Sinuses
Sinuses containing air are present in the sphenoid, ethmoid, maxillary and frontal bones. They all communicate with the nasal cavity and are lined with ciliated mucous membrane. They give resonance to the voice and reduce the weight of the skull, making it easier to carry.
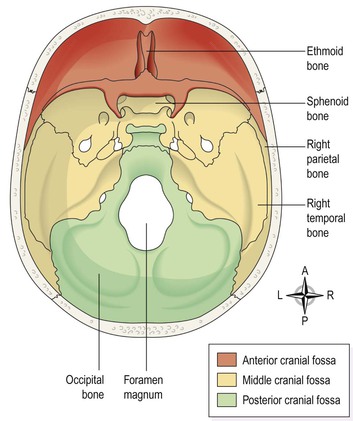
Cranium
The cranium is formed by a number of flat and irregular bones that protect the brain. It has a base upon which the brain rests and a vault that surrounds and covers it. The periosteum lining the inner surface of the skull bones forms the outer layer of dura mater (p. 152). In the mature skull the joints (sutures) between the bones are immovable. The bones have numerous perforations (e.g. foramina, fissures) through which nerves, blood and lymph vessels pass. The bones of the cranium are:
Frontal bone
This is the bone of the forehead. It forms part of the orbital cavities (eye sockets) and the prominent ridges above the eyes, the supraorbital margins. Just above the supraorbital margins, within the bone, are two air-filled cavities or sinuses lined with ciliated mucous membrane, which open into the nasal cavity.
The coronal suture joins the frontal and parietal bones and other sutures are formed with the sphenoid, zygomatic, lacrimal, nasal and ethmoid bones. The frontal bone originates in two parts joined in the midline by the frontal suture (see Fig. 16.18).
Parietal bones
These bones form the sides and roof of the skull. They articulate with each other at the sagittal suture, with the frontal bone at the coronal suture, with the occipital bone at the lambdoidal suture and with the temporal bones at the squamous sutures. The inner surface is concave and is grooved to accommodate the brain and blood vessels.
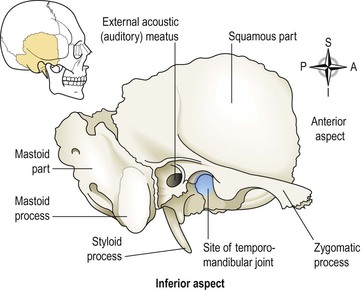
Temporal bones (Fig. 16.12)
These bones lie one on each side of the head and form sutures with the parietal, occipital, sphenoid and zygomatic bones. The squamous part is the thin fan-shaped area that articulates with the parietal bone. The zygomatic process articulates with the zygomatic bone to form the zygomatic arch (cheekbone).
The mastoid part contains the mastoid process, a thickened region easily felt behind the ear. It contains a large number of very small air sinuses that communicate with the middle ear and are lined with squamous epithelium.
The petrous portion forms part of the base of the skull and contains the organs of hearing (the spiral organ) and balance.
The temporal bone articulates with the mandible at the temporomandibular joint, the only movable joint of the skull. Immediately behind this articulating surface is the external acoustic meatus (auditory canal), which passes inwards towards the petrous portion of the bone.
The styloid process projects from the lower process of the temporal bone, and supports the hyoid bone and muscles associated with the tongue and pharynx.
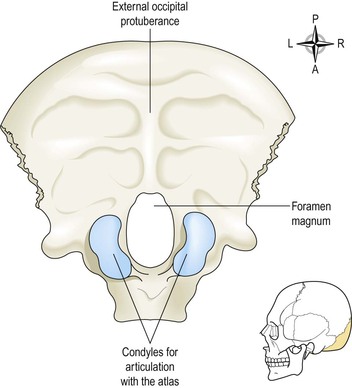
Occipital bone (Fig. 16.13)
This bone forms the back of the head and part of the base of the skull. It forms sutures with the parietal, temporal and sphenoid bones. Its inner surface is deeply concave and the concavity is occupied by the occipital lobes of the cerebrum and by the cerebellum. The occiput has two articular condyles that form condyloid joints (p. 414) with the first bone of the vertebral column, the atlas. This joint permits nodding movements of the head. Between the condyles is the foramen magnum (meaning ‘large hole’) through which the spinal cord passes into the cranial cavity.
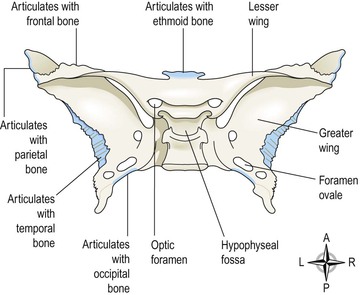
Sphenoid bone (Fig. 16.14)
This bone occupies the middle portion of the base of the skull and it articulates with the occipital, temporal, parietal and frontal bones (Fig. 16.11). It links the cranial and facial bones, and cross-braces the skull. On the superior surface in the middle of the bone is a little saddle-shaped depression, the hypophyseal fossa (sella turcica) in which the pituitary gland rests. The body of the bone contains some fairly large air sinuses lined with ciliated mucous membrane with openings into the nasal cavity. The optic nerves pass through the optic foramina on their way to the brain.
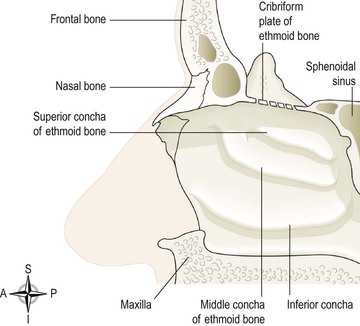
Ethmoid bone (Fig. 16.15)
The ethmoid bone occupies the anterior part of the base of the skull and helps to form the orbital cavity, the nasal septum and the lateral walls of the nasal cavity. On each side are two projections into the nasal cavity, the superior and middle conchae or turbinated processes. It is a very delicate bone containing many air sinuses lined with ciliated epithelium and with openings into the nasal cavity. The horizontal flattened part, the cribriform plate, forms the roof of the nasal cavity and has numerous small foramina through which nerve fibres of the olfactory nerve (sense of smell) pass upwards from the nasal cavity to the brain. There is also a very fine perpendicular plate of bone that forms the upper part of the nasal septum.
Face
The skeleton of the face is formed by 13 bones in addition to the frontal bone already described. Figure 16.16 shows the relationships between the bones:
Zygomatic (cheek) bones
The zygomatic bone originates as two bones that fuse before birth. They form the prominences of the cheeks and part of the floor and lateral walls of the orbital cavities.
Maxilla (upper jaw bone)
This originates as two bones that fuse before birth. The maxilla forms the upper jaw, the anterior part of the roof of the mouth, the lateral walls of the nasal cavity and part of the floor of the orbital cavities. The alveolar ridge, or process, projects downwards and carries the upper teeth. On each side is a large air sinus, the maxillary sinus, lined with ciliated mucous membrane and with openings into the nasal cavity.
Nasal bones
These are two small flat bones that form the greater part of the lateral and superior surfaces of the bridge of the nose.
Lacrimal bones
These two small bones are posterior and lateral to the nasal bones and form part of the medial walls of the orbital cavities. Each is pierced by a foramen for the passage of the nasolacrimal duct that carries the tears from the medial canthus of the eye to the nasal cavity.
Vomer
The vomer is a thin flat bone that extends upwards from the middle of the hard palate to form most of the inferior part of the nasal septum. Superiorly it articulates with the perpendicular plate of the ethmoid bone.
Palatine bones
These are two small L-shaped bones. The horizontal parts unite to form the posterior part of the hard palate and the perpendicular parts project upwards to form part of the lateral walls of the nasal cavity. At their upper extremities they form part of the orbital cavities.
Inferior conchae
Each concha is a scroll-shaped bone, which forms part of the lateral wall of the nasal cavity and projects into it below the middle concha. The superior and middle conchae are parts of the ethmoid bone. The conchae collectively increase the surface area in the nasal cavity, allowing inspired air to be warmed and humidified more effectively.
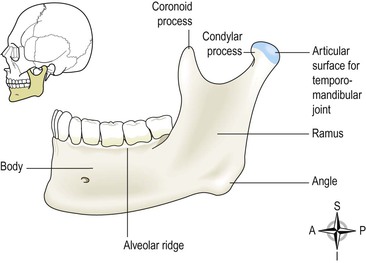
Mandible (lower jaw bone, Fig. 16.17)
This is the lower jaw, the only movable bone of the skull. It originates as two parts that unite at the midline. Each half consists of two main parts: a curved body with the alveolar ridge containing the lower teeth and a ramus, which projects upwards almost at right angles to the posterior end of the body.
At the upper end the ramus divides into the condylar process which articulates with the temporal bone to form the temporomandibular joint (see Fig. 16.12) and the coronoid process, which gives attachment to muscles and ligaments that close the jaw. The point where the ramus joins the body is the angle of the jaw.
Hyoid bone
This is an isolated horseshoe-shaped bone lying in the soft tissues of the neck just above the larynx and below the mandible (see Fig. 10.4). It does not articulate with any other bone, but is attached to the styloid process of the temporal bone by ligaments. It supports the larynx and gives attachment to the base of the tongue.
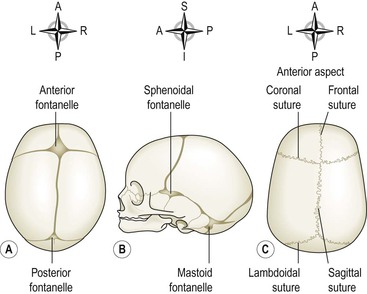
Fontanelles of the skull (Fig. 16.18)
At birth, ossification of the cranial sutures is incomplete. The skull bones do not fuse earlier to allow for moulding of the baby’s head during childbirth. Where three or more bones meet there are distinct membranous areas, or fontanelles. The two largest are the anterior fontanelle, not fully ossified until the child is between 12 and 18 months old, and the posterior fontanelle, usually ossified 2–3 months after birth.
Functions of the skull
The various parts of the skull have specific and different functions:
• the cranium protects the brain
• the bony eye sockets protect the eyes and give attachment to the muscles that move them
• the temporal bone protects the delicate structures of the inner ear
• the sinuses in some face and skull bones give resonance to the voice
• the maxilla and the mandible provide alveolar ridges in which the teeth are embedded
• the mandible, controlled by muscles of the lower face, allows chewing.
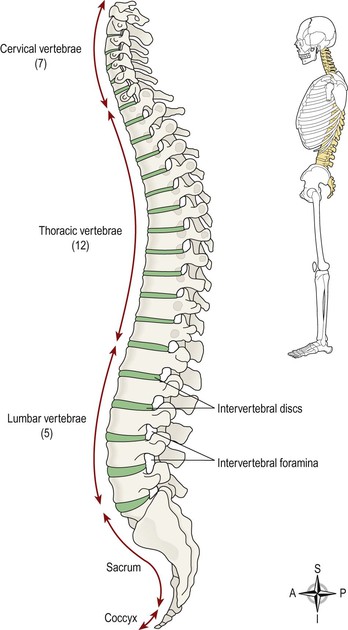
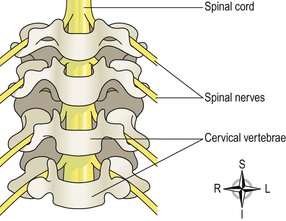
Vertebral column (Fig. 16.19)  16.3
16.3
There are 26 bones in the vertebral column. Twenty-four separate vertebrae extend downwards from the occipital bone of the skull; then there is the sacrum, formed from five fused vertebrae, and lastly the coccyx, or tail, which is formed from between three and five small fused vertebrae. The vertebral column is divided into different regions. The first seven vertebrae, in the neck, form the cervical spine; the next 12 vertebrae are the thoracic spine, and the next five the lumbar spine, the lowest vertebra of which articulates with the sacrum. Each vertebra is identified by the first letter of its region in the spine, followed by a number indicating its position. For example, the topmost vertebra is C1, and the third lumbar vertebra is L3.
The movable vertebrae have many characteristics in common, but some groups have distinguishing features.
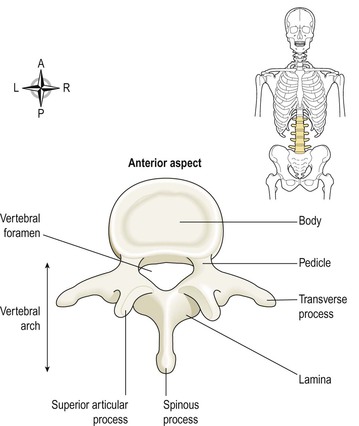
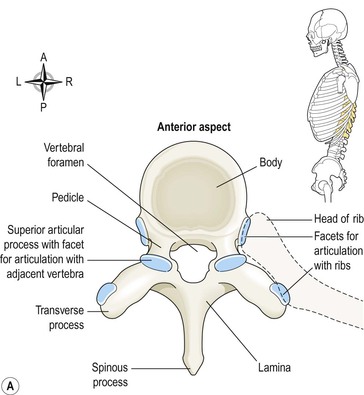
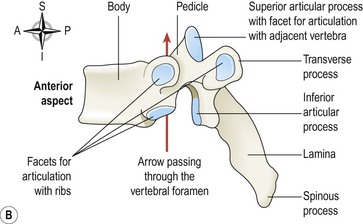
Characteristics of a typical vertebra (Fig. 16.20)
The body.
This is the broad, flattened, largest part of the vertebra. When the vertebrae are stacked together in the vertebral column, it is the flattened surfaces of the body of each vertebra that articulate with the corresponding surfaces of adjacent vertebrae. However, there is no direct bone-to-bone contact since between each pair of bones is a tough pad of fibrocartilage called the intervertebral disc. The bodies of the vertebrae lie to the front of the vertebral column, increasing greatly in size towards the base of the spine, as the lower spine has to support much more weight than the upper regions.
The vertebral (neural) arch.
This encloses a large vertebral foramen. It lies behind the body, and forms the posterior and lateral walls of the vertebral foramen. The lateral walls are formed from plates of bone called pedicles, and the posterior walls are formed from laminae. Projecting from the regions where the pedicle meets the lamina is a lateral prominence, the transverse process, and where the two laminae meet at the back is a process called the spinous process. These bony prominences can be felt through the skin along the length of the spine. The vertebral arch has four articular surfaces: two articulate with the vertebra above and two with the one below. The vertebral foramina form the vertebral (neural) canal that contains the spinal cord.
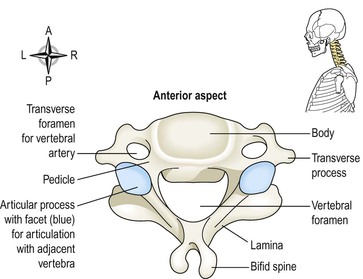
Region-specific vertebral characteristics
Cervical vertebrae (Fig. 16.21)
These are the smallest vertebrae. The transverse processes have a foramen through which a vertebral artery passes upwards to the brain. The first two cervical vertebrae, the atlas and the axis, are atypical.
The first cervical vertebra (C1), the atlas, is the bone on which the skull rests. Below the atlas is the axis, the second cervical vertebra (C2).
The atlas (Fig. 16.22A) is essentially a ring of bone, with no distinct body or spinous process, although it has two short transverse processes. It possesses two flattened facets that articulate with the occipital bone; these are condyloid joints (p. 414) and they permit nodding of the head.
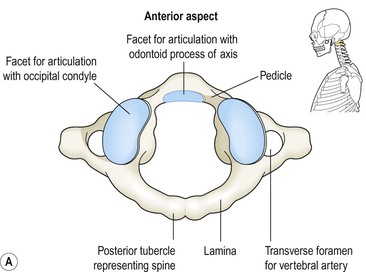
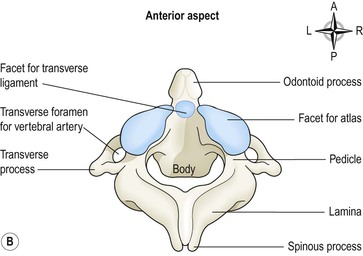
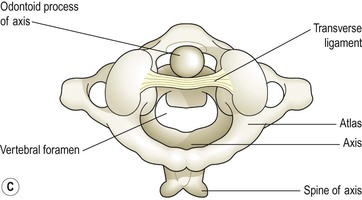
Figure 16.22 The upper cervical vertebrae. Viewed from above. A. The atlas. B. The axis. C. The atlas and axis in position showing the transverse ligament.
The axis (Fig. 16.22B) sits below the atlas, and has a small body with a small superior projection called the odontoid process (also called the dens, meaning tooth). This occupies part of the posterior foramen of the atlas above, and is held securely within it by the transverse ligament (Fig. 16.22C). The head pivots (i.e. turns from side to side) on this joint.
The 7th cervical vertebra, C7, is also known as the vertebra prominens. It possesses a long spinous prominence terminating in a swollen tubercle, which is easily felt at the base of the neck.
Thoracic vertebrae (Fig. 16.23)
The 12 thoracic vertebrae are larger than the cervical vertebrae because this section of the vertebral column has to support more body weight. The bodies and transverse processes have facets for articulation with the ribs.
Lumbar vertebrae (Fig. 16.20)
These are the largest of the vertebrae because they have to support the weight of the upper body. They have substantial spinous processes for attachment of the muscles of the lower back.
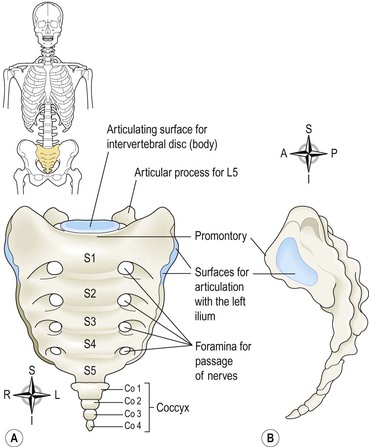
Sacrum (Fig. 16.24)
This consists of five rudimentary vertebrae fused to form a triangular or wedge-shaped bone with a concave anterior surface. The upper part, or base, articulates with the 5th lumbar vertebra. On each side it articulates with the ilium to form a sacroiliac joint, and at its inferior tip it articulates with the coccyx. The anterior edge of the base, the promontory, protrudes into the pelvic cavity. The vertebral foramina are present, and on each side of the bone there is a series of foramina for the passage of nerves.
Coccyx (Fig. 16.24)
This consists of the four terminal vertebrae fused to form a very small triangular bone, the broad base of which articulates with the tip of the sacrum.
Features of the vertebral column
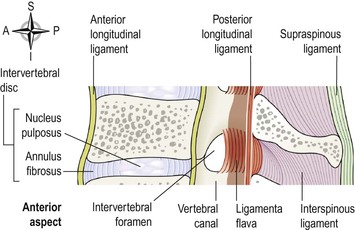
Intervertebral discs
The bodies of adjacent vertebrae are separated by intervertebral discs, consisting of an outer rim of fibrocartilage (annulus fibrosus) and a central core of soft gelatinous material (nucleus pulposus) (Fig. 16.25). They are thinnest in the cervical region and become progressively thicker towards the lumbar region, as spinal loading increases. The posterior longitudinal ligament in the vertebral canal helps to keep them in place. They have a shock-absorbing function and the cartilaginous joints they form contribute to the flexibility of the vertebral column as a whole.
Intervertebral foramina
When two adjacent vertebrae are viewed from the side, a foramen formed by a gap between adjacent vertebral pedicles can be seen.
Throughout the length of the column there is an intervertebral foramen on each side between every pair of vertebrae, through which the spinal nerves, blood vessels and lymph vessels pass (Fig. 16.26).
Ligaments of the vertebral column (Fig. 16.25)
These ligaments hold the vertebrae together and keep the intervertebral discs in position.
The transverse ligament holds the odontoid process of the axis in the correct position in relation to the atlas (Fig. 16.22C).
The anterior longitudinal ligament extends the whole length of the column and lies in front of the vertebral bodies.
The posterior longitudinal ligament lies inside the vertebral canal and extends the whole length of the vertebral column in close contact with the posterior surface of the bodies of the bones.
The ligamenta flava connect the laminae of adjacent vertebrae.
The ligamentum nuchae and the supraspinous ligament connect the spinous processes, extending from the occiput to the sacrum.
Curves of the vertebral column (Fig. 16.27)
When viewed from the side, the vertebral column presents four curves: two primary and two secondary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree