Patient Story
A 47-year-old man with a 40-pack-year history of smoking presents with worsening hoarseness that began approximately 6 weeks ago. He complains of globus sensation and difficulty swallowing solid foods. He denies odynophagia, otalgia, hemoptysis, and hematemesis. There is no associated cough, and he has not had any constitutional symptoms such as fevers, chills, or recent weight loss.
Hoarseness in a middle-aged man with the above symptoms is very common, and the differential diagnosis is long (all the diseases below are possibilities in this case scenario). The patient’s smoking history and duration of symptoms should raise concern for a possible laryngeal malignancy. However, there is a higher incidence of laryngopharyngeal reflux (LPR) followed by benign vocal fold (cord) lesions.
Introduction
The evaluation of hoarseness typically involves first ruling out the most serious pathologies, such as laryngeal squamous cell carcinoma, in adults or recurrent respiratory papillomatosis in children, and then proceeding with a more focused and subtle evaluation to uncover any of the many benign pathologies that affect the larynx. Treatment of these benign pathologies must take into account the patient’s lifestyle and voice needs. It also often incorporates education on vocal hygiene, which involves increasing hydration, decreasing mucus and vocal abuse, and reducing acid reflux if a factor.
Synonyms and Definitions
- Hoarseness, dysphonia, vocal strain, breathiness, raspiness.
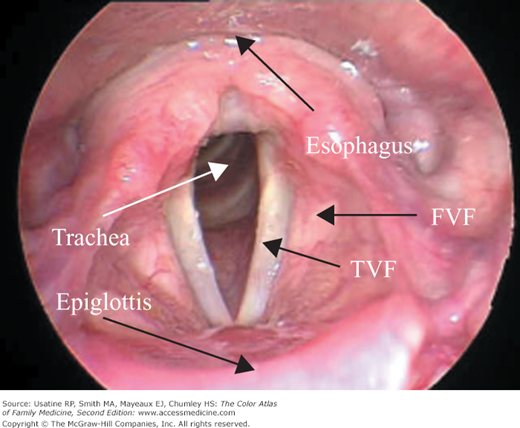
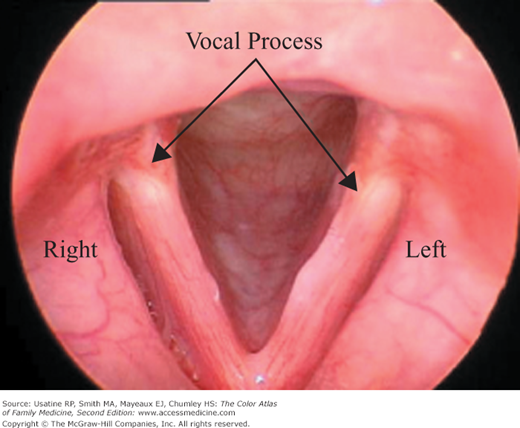
- Vocal cords, true vocal cords, true vocal folds, glottis (Figure 36-1).
- False vocal folds, false vocal cords (mucosal folds in the supraglottis, just superior to the true vocal folds and separated from the true folds by the ventricle).
- Flexible fiberoptic laryngoscopy, direct laryngoscopy, nasopharyngeal scope (NP scope), transnasal fiberoptic laryngoscopy.
- Stroboscopy, videolaryngostroboscopy (VLS), strobe exam.
Epidemiology
- The most common cause of hoarseness in adults and children overall is viral infection causing laryngitis (Figure 36-2).
- LPR disease may be present in up to 50% of patients presenting with voice and laryngeal disorders.1 It is less commonly the sole cause of hoarseness.
- Squamous cell carcinoma (SCC) accounts for 95% of laryngeal cancer. Approximately 11,000 new cases are diagnosed in the United States each year. Peak incidence is in the sixth and seventh decades of life with a strong male predominance.1
- Recurrent respiratory papillomatosis (RRP) represents the most common benign neoplasm of the larynx among children and should be considered in children with chronic hoarseness. A known risk factor for juvenile onset is the triad of a firstborn child (75%), teenage mother, and vaginal delivery. The incidence is 4.3 per 100,000 children and 1.8 per 100,000 adults.2 There is a known association between cervical human papillomavirus (HPV) infection in the mother and juvenile onset RRP, but the precise mode of transmission is unclear. The risk of a child contracting RRP after delivery from an actively infected mother with genital HPV ranges from 0.25% to 3%.3 Because cesarean section does not prevent RRP in all cases, routine prophylactic cesarean section in mothers with active condyloma acuminata is currently not recommended.
Etiology and Pathophysiology
- Laryngitis is a nonspecific term to describe inflammation of the larynx from any cause. Most commonly this is due to a viral upper respiratory infection. Compare the anatomy of the normal larynx (Figure 36-1) with that of acute laryngitis (Figure 36-2), with the primary differences being in the diffuse erythema and edema of the vocal folds and the often transient irregularities of the vocal fold medial edge as compared to the straight medial edge of the normal vocal fold. Laryngeal symptoms result from dry throat, mucous stasis, and recurrent trauma from coughing and throat clearing.
- LPR must be differentiated from gastroesophageal reflux disease (GERD), in which acid reflux is more likely to cause heartburn, indigestion, and regurgitation and does not necessarily reach the larynx or upper aerodigestive tract. LPR is more likely to present with frequent throat clearing, dry cough, hoarseness, and globus sensation, and does not include heartburn in more than 60% of patients. The larynx is highly sensitive to even small amounts of acid or pepsin. Thus, patients who do not have severe enough reflux to cause esophagitis, with its associated symptoms of GERD, may still develop symptomatic laryngeal mucosal injury, with its associated symptoms of LPR.1,4,5,8
- SCC has a multifactorial etiology, but 90% of patients have a history of heavy tobacco and/or alcohol use. These risk factors have a synergistic effect. Other independent risk factors include employment as a painter or metalworker, exposure to diesel or gasoline fumes, and exposure to therapeutic doses of radiation.
- RRP is caused by HPV-6 and HPV-11. Onset is predominantly in young children, although an adult-onset variant exists. Its course is unpredictable and highly variable. Tracheal and bronchopulmonary spread can occur, as can malignant transformation to SCC; the latter is rare. Bronchopulmonary spread is uniformly fatal as a consequence of the lack of surgical options.
- Vocal cord nodules are benign lesions arising from mechanical trauma (vocal abuse or misuse) and are often described as a “callous” of the vocal folds. Vocal cord polyps or cysts can arise from vocal abuse, a blocked mucous gland, vocal fold hemorrhage, a background of polypoid corditis (see below), or idiopathic etiologies. They are a common cause of dysphonia in singers, teachers, and other professional voice users. Vocal cord granulomas are associated with LPR and/or intubation trauma and rarely require surgery.
- Causes of vocal cord paresis or paralysis are myriad:1,6
- Iatrogenic surgical injury (anterior spine fusion, carotid endarterectomy, thyroidectomy) is most common (25%).
- Nonlaryngeal malignancy (mediastinal, bronchopulmonary, and skull base) (24%).
- No identifiable cause (idiopathic), often assumed to be viral (20%).
- Nonsurgical trauma (penetrating/blunt injury and intubation injury) (10%).
- Neurologic causes (stroke, central nervous system [CNS] tumors, multiple sclerosis [MS], and amyotrophic lateral sclerosis [ALS]) (8%).
- Inflammatory/infectious disease (2% to 5%).
- Iatrogenic surgical injury (anterior spine fusion, carotid endarterectomy, thyroidectomy) is most common (25%).
- Presbyphonia is a diagnosis of exclusion denoting vocal changes from aging of the larynx (gradually weakening voice, poor vocal projection, and vocal “roughness”). Hoarseness in patients older than 60 years of age is most commonly a result of benign vocal fold lesions followed by malignancy and vocal fold paralysis. Once a thorough evaluation has been done to rule out organic causes, presbyphonia is the cause of hoarseness in approximately 10% of elderly patients; it is characterized by atrophied vocal folds.7