Patient Story
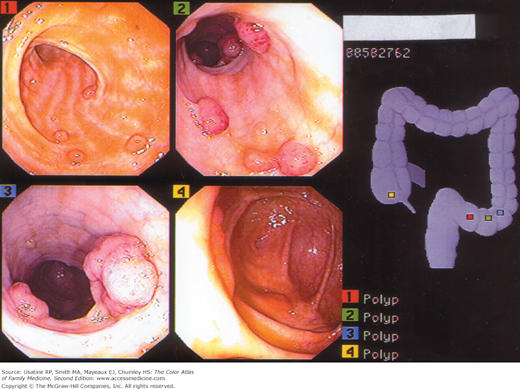
A 62-year-old woman presents to her physician for routine annual examination. She has no known family history of colon disease and is asymptomatic. Stool cards and flexible sigmoidoscopy were recommended and on flexible sigmoidoscopy a 2.4-cm polyp was noted at 35 cm. A colonoscopy was performed and additional polyps were identified in the descending colon and cecum (Figure 63-1).
Epidemiology
- More than 30% of middle-aged and elderly patients are found to have adenomatous polyps on screening and based on autopsy surveys; fewer than 1% will become malignant.1 The lifetime risk of colon cancer is 5.12%.2
- Patients with an adenomatous polyp have a 30% to 50% risk for developing another adenoma and are at higher risk for colon cancer. This risk is greatest in the first 4 years after diagnosis of the first polyp, and greater if a villous adenoma or more than 3 polyps were found.
- Familial adenomatous polyposis of the colon is a rare autosomal dominant disorder. Thousands of adenomatous polyps appear in the large colon, generally by age 25 years, and colorectal cancer develops in almost all of these patients by age 40 years.1 Other hereditary polyposis syndromes include Gardner syndrome, Turcot syndrome, Peutz-Jeghers syndrome, Cowden disease, familial juvenile polyposis, and hyperplastic polyposis.3
Etiology and Pathophysiology
- There are several types of colon polyps, including:
- Hyperplastic polyps—These contain increased numbers of glandular cells with decreased cytoplasmic mucus and an absence of nuclear hyperchromatism, stratification, or atypia. Traditionally thought to be benign, recent evidence suggests malignant potential particularly for right-sided polyps, especially proximal hyperplastic serrated polyps1 and those associated with hyperplastic polyposis syndrome (a familial disorder with multiple [>30] hyperplastic polyps proximal to the sigmoid colon with 2 or more >10 mm).3 The percentage of polyps reported to be in this category ranges from 12% to 90%.3,4
- Adenomatous polyps—These may be tubular, villous (papillary), or tubulovillous. In a case series of 582 patients who had a polyp removed, 81% were adenomatous, including 65.0% that were tubular, 25.8% tubulovillous, 7.2% villous adenomas, and 0.5% mixed adenomatous hyperplastic polyps; 12 (1.4%) were invasive carcinomas.4
- Adenomatous polyps may be pedunculated or sessile; cancers more frequently develop in sessile polyps.1
- Villous polyps can cause hypersecretory syndromes characterized by hypokalemia and profuse mucous discharge; these more frequently harbor carcinoma in situ or invasive carcinoma than other adenomas.3
- Nonneoplastic hamartoma (juvenile polyp)—These are benign cystic polyps with mucous-filled glands, most commonly found in male children, ages 2 to 5 years, and are often found as singular lesions, but additional polyps are found on panendoscopy in 40% to 50% of children. Juvenile polyps in adolescence may be associated with hereditary syndromes that carry malignant potential.5
- Hyperplastic polyps—These contain increased numbers of glandular cells with decreased cytoplasmic mucus and an absence of nuclear hyperchromatism, stratification, or atypia. Traditionally thought to be benign, recent evidence suggests malignant potential particularly for right-sided polyps, especially proximal hyperplastic serrated polyps1 and those associated with hyperplastic polyposis syndrome (a familial disorder with multiple [>30] hyperplastic polyps proximal to the sigmoid colon with 2 or more >10 mm).3 The percentage of polyps reported to be in this category ranges from 12% to 90%.3,4
- A series of genetic/molecular changes have been found that are thought to represent a multistep process from normal colon mucosa to malignant tumor.3 These include:
- Point mutations in the K-ras protooncogene leading to gene activation and deletion of DNA at the site of tumor-suppressor gene.
- This results in an altered proliferative pattern and polyp formation.
- Mutational activation of an oncogene, coupled with loss of tumor-suppressor genes, leads to malignant transformation.
- Serrated polyps, which have in the past been characterized as hyperplastic polyps, are now known to have epigenetic alterations that may develop into colon cancers by another pathway—the CpG-island-methylation-phenotype pathway.6
- Patients with familial polyposis inherit a germline alteration that leads into the above pathway.
- Point mutations in the K-ras protooncogene leading to gene activation and deletion of DNA at the site of tumor-suppressor gene.
- Insulin resistance, with increased concentrations of insulin-like growth factor type I, may also stimulate proliferation of the intestinal mucosa.
Risk Factors
- Older age—99% of cases occur in people older than age 40 years and 85% in those older than age 60 years.7
- Family history—Present in 10% to 20% of cases.7
- Diet appears to be associated with colon polyps and colon cancer. Animal fats may alter anaerobes in the gut microflora, increasing conversion of normal bile acids to carcinogens. Also, increased cholesterol is associated with an enhanced risk of development of adenomas.
- There may be an association between Helicobacter exposure and colonic polyps.8,9
Diagnosis
- Usually asymptomatic.
- Patients may experience overt or occult rectal bleeding.
- Change in bowel habits—Diarrhea or constipation can occur, often with decreased stool caliber.
- Secretory villous adenomas can occasionally manifest as a syndrome of severe diarrhea with massive fluid and electrolyte loss.3
- Cancer distribution is approximately equal between the right and left colon. Juvenile polyps are usually found in the rectosigmoid region.
- Occult blood in the stool is found in less than 5% of patients with polyps.1 Of the 2% to 4% of asymptomatic patients who have heme positive stool on screening, 20% to 30% will have polyps.1
- For patients with a family history of familial adenomatous polyposis, DNA testing may be performed to detect the adenomatous polyposis coli (APC) gene mutation; this can lead to a definitive diagnosis before the development of polyps.1 SOR C A positive test finding only indicates susceptibility, not the actual presence of a polyp.3
- Genetic testing can also be considered for patients with a family history of hereditary nonpolyposis colorectal cancer (HNPCC), which is caused by germline mutation of the DNA mismatch repair genes (hMLH1, hMSH2, hPMS1, hPMS2, hMSH6).10 SOR C
- Polyps may be identified on barium enema (Figures 63-2 and 63-3), flexible sigmoidoscopy, or colonoscopy (including virtual computer tomography colonoscopy) (Figures 63-1 and 63-4).
- A polyp is defined as grossly visible protrusion from the mucosal surface, although adenomas can also be flat or even depressed.11
- Colonoscopy must be subsequently performed to identify additional lesions and remove all lesions.
- Synchronous lesions occur in one-third of cases (Figure 63-1).