Patient Story
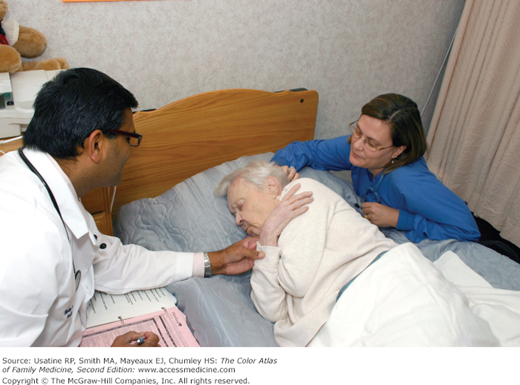
An 89-year-old frail woman presents with Alzheimer dementia, hypothyroidism, depression, congestive heart failure, and macular degeneration. Her functional status was gradually declining. It was difficult for her family to provide 24-hour care and she was admitted to a nursing facility. Her dementia worsened over a period of 2 years in the nursing facility and she became incontinent of urine and feces while developing limitations in speech and ambulation. She could not sit up without assistance and lost her ability to smile and hold her head up independently. The facility was very supportive and a hospice consult was initiated. Figure 5-1 shows Dr. Gokula along with the hospice nurse visiting the patient for admission to hospice care.
Introduction
End-of-life care is care that is delivered to patients of all ages who have a very short life expectancy. This care is focused on meeting the patient’s emotional and physical needs for symptom relief and general comfort care, and offering patient and family support.
- Respect the goals, preferences, and choices of the person.
- Look after the medical, emotional, social, and spiritual needs.
- Support the needs of family members.
- Help patients and their families access needed healthcare providers and appropriate care settings.
- Provide excellence in care at the end of life (see Figure 5-1).
- Physical and emotional symptom management.
- Support of function, autonomy, personal dignity, and self-respect.
- Advanced care planning.
- Aggressive symptom control near death.
- Patient and family satisfaction.
- Patient’s assessment of overall quality of life and well-being.
- Family burden—emotional and financial.
- Survival time.
- Provider continuity and skill.
- Bereavement services.
Epidemiology
- Approximately 25,000 children per year in the United States are born with or develop a serious or life-threatening disease such as cancer, cystic fibrosis, cerebral palsy, or muscular dystrophy.3
- According to National Health Center statistics, there were approximately 2.46 million deaths in the United States in 2010; most were attributed to cardiovascular disease and cancer.4
- Among patients ages 1 to 24 years, leading causes of death were external causes (i.e., accidents, homicide, and suicide), followed by cancer and heart disease. As age increases, there is a trend toward chronic conditions being responsible for deaths.
- The major causes of death in the population ages 25 to 44 years were accidents, cancer, heart disease, suicide, homicide, and other causes.
- For those ages 45 to 64 years, leading causes of death were cancer, heart disease, accidents, chronic respiratory diseases, and liver disease.
The common causes of death in persons older than age 65 years are heart disease, cancer, chronic lower respiratory disease, stroke, and Alzheimer disease.
- Among patients ages 1 to 24 years, leading causes of death were external causes (i.e., accidents, homicide, and suicide), followed by cancer and heart disease. As age increases, there is a trend toward chronic conditions being responsible for deaths.
- In 2009, heart disease, cancer, chronic lower respiratory diseases, stroke, and accidents accounted for almost 64% of all deaths in the United States.5
- Thirty-two percent of all deaths in the United States in 2007 were inpatient hospital deaths.6 Average hospital costs for a stay ending in death were $23,000, approximately 2.7 times higher than for a patient discharged alive.
Hospice services were involved for approximately 20% of dying patients.7 More than 70% of hospice patients had cancer and 90% of hospice patients died outside the hospital. The use of hospice and other end-of-life services varies among different racial groups in the United States:8
- Whites are more aware of advanced directives when compared to the nonwhite racial or ethnic groups.
- The use of life-sustaining treatments is more common among African Americans when compared to other racial groups.
- Cultural differences are also seen for disclosure of information about a terminal illness. Korean, Mexican, Japanese, and Native American populations are more likely to discourage discussion of terminal illness and patient prognosis and prefer families to be informed.
- The involvement of family in the decision-making process with end-of-life care was seen among all racial groups, but Asian and Hispanic Americans prefer family-centered decision making when compared to other racial and ethnic groups.
Etiology and Pathophysiology
- Tobacco use—Of all the adults in the United States, 20.6% smoke cigarettes; the highest rates are among men (23.5%) and American Indians/Alaska Natives (23.2%).9 It is estimated that nearly 1 of every 5 deaths each year in the United States is attributable to smoking.10 Smoking increases the risk of developing emphysema (10- to 13-fold), heart and cardiovascular disease (2- to 4-fold), and many cancers (1.4- to 3-fold).
- Poor diet—Diets that are high in fat (>40% of calories consumed) are associated with increased risk of breast, colon, endometrial, and prostate cancer. Diet is important in controlling diabetes, heart disease, obesity, and chronic renal disease.
- Physical inactivity—Those who exercise regularly live longer and are healthier; exercise reduces the risk of cardiovascular disease and hypertension and improves function in those with depression, osteoarthritis, and fibromyalgia. Unfortunately less than 20% of adults met the 2008 federal guidelines for aerobic activity and muscle-strengthening.11
- Alcohol consumption—Alcohol is consumed by 80% of the population, and 10% to 15% of men and 5% to 8% of women are alcohol dependent. Excess alcohol consumption (>3 drinks per day) is associated with mood disorders (10% to 40%), cirrhosis (15% to 20%), and neuropathy (5% to 15%); it increases the risk of pancreatitis (3-fold) as well as cancers of the breast (1.4-fold), esophagus (3-fold), and rectum (1.5-fold).12 In addition, based on data from 2009, an estimated 30.2 million people (12%) ages 12 years or older reported driving under the influence of alcohol at least once in the past year.13
- Injury—In 2004, 167,184 people died as a result of injury, accounting for 7% of all deaths.14 The majority of injury-related deaths are unintentional. Falls are the leading mechanism of injury-related death for elderly people, while for adults 35 to 53 years of age, poisoning is the leading mechanism of injury-related death. Motor vehicles in traffic are the leading mechanism of injury-related death for all other age groups, except for children younger than age 2 years. Many of these deaths are preventable.
- Sexual behaviors—Sexually transmitted infections (STIs) are among the most common infectious diseases and affect approximately 13 million people in the United States each year; most of these people are younger than age 25 years. Sexually transmitted diseases (STDs) are associated with increased risk of HIV/AIDS; in 2007, there were approximately 455,636 persons living with AIDS in the United States.15 Causes of death from AIDS include infections (especially pulmonary and central nervous system), cancer (especially Kaposi sarcoma and non-Hodgkin lymphoma), cardiomyopathy, and nephropathy.
- Illicit use of drugs—Drug addiction remains a major problem in the United States. According to data from the National Institute on Drug Abuse Monitoring the Future Survey of more than 46,000 eighth to 12th grade students, increases were seen in daily marijuana use (21.4% of high school seniors in the past 30 days) and lifetime ecstasy use in eighth graders (from 2.2% in 2009 to 3.3% in 2010), while decreases were noted in methamphetamine use (from 6.5% in 1999 to 2.2% in 2010) and current cocaine use (from 2.3 million in 2003 to 1.6 million in 2009).12 Cocaine is associated with death from respiratory depression, cardiac arrhythmias, and convulsions; methamphetamine use is associated with life-threatening hypertension, cardiac arrhythmia, subarachnoid and intracerebral hemorrhage, ischemic stroke, convulsions, and coma.
- Microbial agents—Microbial agents remain a major cause of death and disability with continued discovery of new agents and increasing drug resistance. Although it is difficult to ascertain whether an infectious agent caused death or was incidental to death, the expert panel of investigators in New Mexico, on the basis of autopsy data, found that 85% (106 of 125) of the deaths (late 1994 to mid-1996) were identified as infectious disease related.16
- Toxic agents—Toxic agents include poisons and environmental toxins. In the United States in 2008, there were 36,500 poisoning deaths; the vast majority were unintentional.17 Opioid pain medications were involved in more than 40%. Poisoning was the third-leading method of suicide from 2005 to 2007, with 75% a result of alcohol and/or drug overdose. The most commonly used drugs identified in drug-related suicides were prescription drugs in the opioid, benzodiazepine, and antidepressant classes.18
Diagnosis
It is estimated that approximately 70% of all deaths are preceded by a disease/condition such that it is reasonable to plan for dying in the near future.6 These diseases/conditions are as follows:
- Cancer that is widespread, aggressive, or metastatic and for patients who no longer seek curative care. Other clues include a decline in performance status and/or significant unintentional weight loss.
- Dementia with an inability to ambulate, bathe, or dress without assistance; associated urinary or fecal incontinence; inability to meaningfully communicate; or associated with life-threatening infections, multiple stage 3 or 4 skin ulcers, inability to maintain sufficient fluid and calorie intake, or failure to thrive (including a temporal decline in functional status).
- Patients confined to bed or who require assistance with all the basic activities of daily living.
- Patients with a body mass index less than 22 and/or those who refuse or do not respond to enteral or parenteral nutritional support.
- Heart disease that is poorly responsive to optimal medical treatment, New York Heart Association (NYHA) class IV, or congestive heart failure with poor ejection fraction (≤20%). Based on data from multiple studies including SUPPORT, Framingham, and IMPROVEMENT, 1-year mortality estimates are as follows: NYHA Class II (mild symptoms), 5% to 10%; Class III (moderate symptoms), 10% to 15%; Class IV (severe symptoms), 30% to 40%. Independent predictors of poor prognosis in patients with heart failure include recent cardiac hospitalization, renal insufficiency (creatinine ≥1.4 mg/dL), systolic blood pressure less than 100 mm Hg and/or pulse greater than 100 beats/min, treatment-resistant ventricular dysrhythmias, treatment resistant-anemia, hyponatremia, cachexia, reduced functional capacity, and comorbidities (e.g., diabetes).19
- HIV/AIDS with CD4 count less than 25 or persistent viral load greater than 100,000 copies/mL plus at least one of the following: wasting (loss of 33% of lean body mass); major AIDS-defining refractory infection (e.g., Cryptosporidium infection) or malignancy (e.g., central nervous system or systemic lymphoma); progressive multifocal leukoencephalopathy; renal failure; Karnofsky Performance Status (KPS) less than 50%; advanced AIDS dementia complex; or significant functional decline in the activities of daily living.
- Neurologic disease (e.g., Parkinson disease, amyotrophic lateral sclerosis, multiple sclerosis, muscular dystrophy, and myasthenia gravis) that is associated with rapid progression and/or critical nutritional state, life-threatening infections in the preceding 12 months, stage 3 or 4 skin ulcers, critically impaired breathing capacity and declined ventilator support, or life-threatening complications (e.g., recurrent aspiration, sepsis).
- Pulmonary disease, including disabling dyspnea at rest or with minimal exertion, increased emergency department visits and/or hospitalizations, hypoxemia on room air (oxygen saturation <88%), cor pulmonale, unintentional progressive weight loss, or resting tachycardia greater than 100 beats/min.
- End-stage renal disease with progressive decline in those not seeking dialysis (or not a candidate), with a calculated creatinine clearance less than 10 (<15 for patients with diabetes) or serum creatinine greater than 8 mg/dL (>6 mg/dL for patients with diabetes).
- End-stage liver disease with progressive decline in those with refractory ascites, spontaneous bacterial peritonitis, hepatorenal syndrome, hepatic encephalopathy, or recurrent variceal bleeding despite treatment.
- Stroke associated with coma in the acute phase; coma with abnormal brainstem response, absent verbal response, absent withdrawal response to pain, or serum creatinine greater than 1.5 mg/dL at day 3; dysphagia and insufficient intake of fluids and calories; poor functional status; or poststroke dementia.
- Nonspecific terminal illness characterized by a rapid decline, disease progression, or progressive weight loss; dysphasia with aspiration; increase in emergency department visits and/or hospitalizations; worsening pressure ulcers despite optimum care; or a decline in systolic blood pressure below 90 mm Hg.
Unfortunately, physicians are often reluctant to make this determination, resulting in palliative and hospice care not being offered until very late in the course of the illness. In addition, physicians often believe that they must be able to predict a life expectancy of less than 6 months with certainty to institute hospice care.
The National Hospice and Palliative Care Organization has evidence-based guidelines on determining prognosis for a number of noncancer conditions.20 This information can assist clinicians in working with patients who are at the end of life on their advanced care decisions and planning.
Two validated instruments that may help clinicians estimate prognosis are the Palliative Performance Scale (PPS) and the KPS.
- The PPS (http://meds.queensu.ca/assets/palliative-care/ppcip_resource_manual_pps_description.pdf) rates information on ambulation, activity and evidence of disease, self-care, intake, and consciousness level. In a retrospective cohort study, the PPS was found to be a strong predictor of survival when applied at admission to patients in palliative care.21 In this study, median survival time at PPS of 10% was 1 day, survival with PPS of 20% was 2 days, at PPS of 30% survival was 9 days, while at PPS of 60% median survival was 40 days.
- The KPS (http://www.hospicepatients.org/karnofsky.html) is often used to follow the course of illness and is based on performance status ranging from normal (100%) to dead (0%).
Common physical symptoms reported by dying patients:6
- Constipation (90%).
- Fatigue and weakness (90%).
- Dyspnea (75%) and other cardiopulmonary symptoms such as cough.
- Pain (36% to 90%).
- Insomnia.
- Other GI symptoms, including dry mouth, anorexia, nausea, vomiting, constipation, diarrhea, and dysphagia.
- Fecal and urinary incontinence.
- Dizziness.
- Swelling and numbness of the extremities.
Common mental and psychological symptoms reported by dying patients:6
- Depression (75% symptomatic; <25% with major depression) and feelings of hopelessness, anxiety, and/or irritability.
- Confusion and delirium (up to 85% at the end stage).
A population-based survey of family members, friends, and care givers in six U.S. communities found that:22
- Seventy-one percent of terminally ill patients had shortness of breath.
- Fifty percent had moderate to severe pain.
- Thirty-six percent were incontinent of urine or feces.
- Eighteen percent were fatigued enough to spend more than 50% of their waking hours in bed.
Management
Management often begins with communicating bad news to patients and families about likely or imminent death. This task can be extremely difficult. In cases where the patient is not deemed legally competent, make sure that the legal decision maker is present. In addition, if the patient is a non-English speaker, consider obtaining a skilled medical interpreter rather than relying on a family member. Providers may find the following P-SPIKES approach useful:23
- Preparation—Review information to be presented and practice.
- Setting—Arrange time and place, ensure privacy, and include important support persons.
- Perception of patient—Inquire about the patient’s and the family’s understanding of the illness.
- Information needs—Find out about what the patient and family need to be told and in how much detail.
- Knowledge of the condition—Provide bad news sensitively and slowly, warning them any bad news is imminent and checking to see whether there is understanding.
- Empathy and exploration—Acknowledge the feelings expressed, give the patient and family time to react, and remind them that you are not abandoning them.
- Summary/strategic planning—Discuss next steps or schedule follow-ups to do this if more time is needed.
Roles for the primary care provider include consultation, providing anticipatory guidance, providing support and comfort, and assisting with identifying and managing symptoms (including pain control) (Figure 5-2).