Chapter 13 The Hepatobiliary System
2 What are the most common morphologic signs of liver injury?
 Vacuolar change: Affected hepatocytes are enlarged and have a swollen, clear cytoplasm. This hydropic swelling of hepatocytes is a common response to injury. It is reversible, but if intensified or prolonged, it may lead to liver cell necrosis.
Vacuolar change: Affected hepatocytes are enlarged and have a swollen, clear cytoplasm. This hydropic swelling of hepatocytes is a common response to injury. It is reversible, but if intensified or prolonged, it may lead to liver cell necrosis. Apoptosis: The hepatocytes undergoing apoptosis appear rounded and detach from the other liver cells. They have a pyknotic nucleus, which ultimately disappears, leaving the remaining cytoplasm as a “round red body,” also known as acidophilic body. Apoptosis of single hepatocytes is a typical feature of viral hepatitis, but it may be induced by other liver diseases as well.
Apoptosis: The hepatocytes undergoing apoptosis appear rounded and detach from the other liver cells. They have a pyknotic nucleus, which ultimately disappears, leaving the remaining cytoplasm as a “round red body,” also known as acidophilic body. Apoptosis of single hepatocytes is a typical feature of viral hepatitis, but it may be induced by other liver diseases as well. Necrosis: Irreversible injury of hepatocytes induced by ischemia, toxins, and viruses typically involves portions of the liver acinus. It is customary to describe necrosis as either focal (random) or zonal, if limited to one of the three zones of the liver acinus. Zone 3 necrosis (also known as centrolobular necrosis) is the most common form of necrosis and is found in ischemic liver injury (e.g., in hypotensive shock) but also in many forms of toxic liver injury.
Necrosis: Irreversible injury of hepatocytes induced by ischemia, toxins, and viruses typically involves portions of the liver acinus. It is customary to describe necrosis as either focal (random) or zonal, if limited to one of the three zones of the liver acinus. Zone 3 necrosis (also known as centrolobular necrosis) is the most common form of necrosis and is found in ischemic liver injury (e.g., in hypotensive shock) but also in many forms of toxic liver injury.3 How does the liver respond to injury?
 Inflammation: Injured liver cells must be removed. To this end, the body sends in inflammatory cells that react with injured hepatocytes. For example, hepatocytes infected with hepatitis virus elicit a T-cell response. These lymphocytes enter the liver and kill the infected hepatocytes, which are thereafter removed by macrophages.
Inflammation: Injured liver cells must be removed. To this end, the body sends in inflammatory cells that react with injured hepatocytes. For example, hepatocytes infected with hepatitis virus elicit a T-cell response. These lymphocytes enter the liver and kill the infected hepatocytes, which are thereafter removed by macrophages. Regeneration: Liver cells are stable facultative mitotic cells that can enter into the mitotic cycle on demand and by dividing replace the damaged cells. Regeneration of the liver is a major response of the liver to injury. In experimental animals, it has been shown that the liver can regenerate even after two thirds of it has been removed. Massive necrosis induced by toxins and viruses typically elicits a major regeneration wave, but in many instances, this is not sufficient to save the patient’s life. However, focal necrosis and apoptosis are easily repaired.
Regeneration: Liver cells are stable facultative mitotic cells that can enter into the mitotic cycle on demand and by dividing replace the damaged cells. Regeneration of the liver is a major response of the liver to injury. In experimental animals, it has been shown that the liver can regenerate even after two thirds of it has been removed. Massive necrosis induced by toxins and viruses typically elicits a major regeneration wave, but in many instances, this is not sufficient to save the patient’s life. However, focal necrosis and apoptosis are easily repaired. Fibrosis: Extensive necrosis, especially if accompanied by persistent inflammation or toxic influences, cannot be repaired by regeneration. Portions of the liver are replaced by connective tissue scars. Fibrosis associated with nodular regeneration of the remaining hepatocytes is typical of end-stage liver disease, known as cirrhosis.
Fibrosis: Extensive necrosis, especially if accompanied by persistent inflammation or toxic influences, cannot be repaired by regeneration. Portions of the liver are replaced by connective tissue scars. Fibrosis associated with nodular regeneration of the remaining hepatocytes is typical of end-stage liver disease, known as cirrhosis.5 Discuss the necroinflammatory indices, that is, the laboratory tests used to monitor the integrity of liver cells
6 Which tests are used to measure hepatic secretory function?
 Albumin: Normally, the blood contains 3.5 to 5.0 g/dL (35–50 g/L) albumin, the most copious plasma protein. Chronic liver injury will reduce blood concentration of albumin to less than 3 g/dL.
Albumin: Normally, the blood contains 3.5 to 5.0 g/dL (35–50 g/L) albumin, the most copious plasma protein. Chronic liver injury will reduce blood concentration of albumin to less than 3 g/dL.7 Discuss the tests used to measure biliary excretion
 Bilirubin: Bilirubin that has been conjugated in the liver to be excreted into the intestine may accumulate in the blood of patients who have bile duct obstruction.
Bilirubin: Bilirubin that has been conjugated in the liver to be excreted into the intestine may accumulate in the blood of patients who have bile duct obstruction. Alkaline phosphatase: This enzyme is found along the liver cell membrane lining the intercellular canaliculi. Obstructive jaundice interferes with the normal biliary elimination of this enzyme, which then appears in the blood. Elevated levels of alkaline phosphatase in blood are typical of obstructive jaundice.
Alkaline phosphatase: This enzyme is found along the liver cell membrane lining the intercellular canaliculi. Obstructive jaundice interferes with the normal biliary elimination of this enzyme, which then appears in the blood. Elevated levels of alkaline phosphatase in blood are typical of obstructive jaundice. Gamma-glutamyltransferase (GGT): In contrast to alkaline phosphatase, which is found in many other organs, GGT is primarily a hepatic enzyme. Elevation of GGT is a reliable sign of biliary obstruction. However, GGT is also induced in liver cells by alcohol or phenobarbital and some other drugs that stimulate the P450 system. GGT is thus a marker of liver cell injury (especially alcohol-induced injury).
Gamma-glutamyltransferase (GGT): In contrast to alkaline phosphatase, which is found in many other organs, GGT is primarily a hepatic enzyme. Elevation of GGT is a reliable sign of biliary obstruction. However, GGT is also induced in liver cells by alcohol or phenobarbital and some other drugs that stimulate the P450 system. GGT is thus a marker of liver cell injury (especially alcohol-induced injury).JAUNDICE
10 Describe how bilirubin is formed
 Inefficient hematopoiesis (i.e., heme not utilized for the synthesis of hemoglobin in nascent red blood cells in the bone marrow; 10%)
Inefficient hematopoiesis (i.e., heme not utilized for the synthesis of hemoglobin in nascent red blood cells in the bone marrow; 10%)11 How is bilirubin processed?
 Binding of bilirubin to albumin (Bilirubin bound to albumin is not water soluble and does not appear in urine. In clinical laboratories, it is measured as indirect bilirubin.)
Binding of bilirubin to albumin (Bilirubin bound to albumin is not water soluble and does not appear in urine. In clinical laboratories, it is measured as indirect bilirubin.) Transport of albumin-bound bilirubin to the liver (It is worth remembering that this bilirubin is called unconjugated or indirect bilirubin.)
Transport of albumin-bound bilirubin to the liver (It is worth remembering that this bilirubin is called unconjugated or indirect bilirubin.) Conjugation of bilirubin to glucuronic acid (This is accomplished by a microsomal hepatic enzyme, bilirubin–uridine diphosphate–glucuronyltransferase [UGT]. The bilirubin glucuronidating isoform of this enzyme is called UGT1A1.)
Conjugation of bilirubin to glucuronic acid (This is accomplished by a microsomal hepatic enzyme, bilirubin–uridine diphosphate–glucuronyltransferase [UGT]. The bilirubin glucuronidating isoform of this enzyme is called UGT1A1.) Excretion of water-soluble bilirubin glucuronides in bile (This bilirubin is called conjugated or direct bilirubin.)
Excretion of water-soluble bilirubin glucuronides in bile (This bilirubin is called conjugated or direct bilirubin.) Deconjugation of some bilirubin glucuronides by bacteria in the intestine (This process leads to the formation of colorless urobilinogen, 80% of which is excreted in feces together with the remaining conjugated bilirubin.)
Deconjugation of some bilirubin glucuronides by bacteria in the intestine (This process leads to the formation of colorless urobilinogen, 80% of which is excreted in feces together with the remaining conjugated bilirubin.)12 Why is it important to fractionate bilirubin in the serum?
According to laboratory analysis, hyperbilirubinemia can be classified as follows:
13 Describe the main forms of jaundice
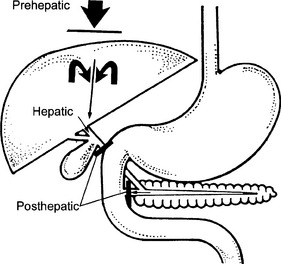
Three pathogenetic forms of jaundice are recognized clinically (Fig. 13-1):
15 What are the main causes of predominantly unconjugated hyperbilirubinemia?
 Transfusion reaction due to the hemolysis of donor red blood cells (RBCs) by recipient’s natural anti-AB antibodies
Transfusion reaction due to the hemolysis of donor red blood cells (RBCs) by recipient’s natural anti-AB antibodies Erythroblastosis fetalis (transplacental immunization of the mother to fetal RBC antigens, reacting with RBCs of the second baby and causing severe hemolysis in the fetus or neonate. This results in kernicterus, i.e., deposition of bilirubin in basal ganglia of the baby’s brain.)
Erythroblastosis fetalis (transplacental immunization of the mother to fetal RBC antigens, reacting with RBCs of the second baby and causing severe hemolysis in the fetus or neonate. This results in kernicterus, i.e., deposition of bilirubin in basal ganglia of the baby’s brain.) Resorption of bilirubin from internal hemorrhages (e.g., massive hematoma and intestinal hemorrhage)
Resorption of bilirubin from internal hemorrhages (e.g., massive hematoma and intestinal hemorrhage)17 What is the cause of jaundice in genetic diseases characterized by unconjugated hyperbilirubinemia?
21 List common causes of mixed hyperbilirubinemia
Mixed hyperbilirubinemia is a sign of “hepatic jaundice” and it is typically seen in:
HEPATIC FAILURE
28 What are the clinical features of chronic liver failure?
 Cirrhosis with changes in the shape and size of the liver best visible by computed axial tomography (CAT) scan
Cirrhosis with changes in the shape and size of the liver best visible by computed axial tomography (CAT) scanA mnemonic for the consequences of liver failure is jaundice:
30 What are the main forms of portal hypertension?
Three forms of portal hypertension are recognized depending on the site of obstruction:
 Presinusoidal: This is due to obstruction of the portal vein or its major intrahepatic branches. Typically, this occurs in portal vein thrombosis or fibrosis of bile ducts (e.g., schistosomiasis) that affects the adjacent blood vessels in the liver.
Presinusoidal: This is due to obstruction of the portal vein or its major intrahepatic branches. Typically, this occurs in portal vein thrombosis or fibrosis of bile ducts (e.g., schistosomiasis) that affects the adjacent blood vessels in the liver. Sinusoidal: This is due to intrahepatic obstruction of blood flow through the sinusoids. It accounts for 90% of all cases of portal hypertension and is typically a feature of cirrhosis.
Sinusoidal: This is due to intrahepatic obstruction of blood flow through the sinusoids. It accounts for 90% of all cases of portal hypertension and is typically a feature of cirrhosis.32 Where do portal–systemic anastomoses develop in portal hypertension?
Shunting of portal venous blood into the systemic circulation occurs at three anatomic sites:
 Esophageal and gastric veins: Esophageal varices are the most common site of massive bleeding in patients with chronic liver disease. Exsanguination from ruptured esophageal varices is a major cause of death in cirrhosis.
Esophageal and gastric veins: Esophageal varices are the most common site of massive bleeding in patients with chronic liver disease. Exsanguination from ruptured esophageal varices is a major cause of death in cirrhosis.33 Discuss the pathogenesis of ascites in cirrhosis
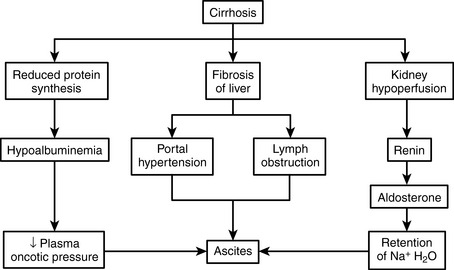
The pathogenesis of ascites is not fully understood, but it appears to be a consequence of several disturbances found in patients with cirrhosis (Fig. 13-2):
 Portal hypertension: Increased hydrostatic pressure leads to transudation of fluid into the abdominal cavity.
Portal hypertension: Increased hydrostatic pressure leads to transudation of fluid into the abdominal cavity. Hypoalbuminemia: Cirrhotic livers cannot produce albumin in adequate amounts, and hypoalbuminemia is a common finding in these patients. Hypoalbuminemia is associated with reduced oncotic pressure of the plasma and reduced reentry of fluid into the blood vessels at the venular side of the microcirculation.
Hypoalbuminemia: Cirrhotic livers cannot produce albumin in adequate amounts, and hypoalbuminemia is a common finding in these patients. Hypoalbuminemia is associated with reduced oncotic pressure of the plasma and reduced reentry of fluid into the blood vessels at the venular side of the microcirculation. Lymphatic overflow: The lymph flow through the thoracic duct in patients with cirrhosis exceeds the capacity of this duct to drain the lymph from the portal area, and it “overflows” into the abdominal cavity.
Lymphatic overflow: The lymph flow through the thoracic duct in patients with cirrhosis exceeds the capacity of this duct to drain the lymph from the portal area, and it “overflows” into the abdominal cavity. Hyperaldosteronism: The escape of fluids from blood vessels into the abdominal cavity is recognized by the volume regulatory sensors as “depletions” of circulating fluid mass, which triggers a release of aldosterone. Aldosterone acts at the level of renal tubules, conserving sodium and water, which then flows over into the abdominal cavity, further contributing to the formation of ascites.
Hyperaldosteronism: The escape of fluids from blood vessels into the abdominal cavity is recognized by the volume regulatory sensors as “depletions” of circulating fluid mass, which triggers a release of aldosterone. Aldosterone acts at the level of renal tubules, conserving sodium and water, which then flows over into the abdominal cavity, further contributing to the formation of ascites.35 Explain the pathogenesis of palmar erythema, gynecomastia, and spider angiomas in patients with cirrhosis
36 Explain the bleeding tendency commonly found in patients with cirrhosis
 Reduced concentration of coagulation factors in blood: One should remember that most of the plasma coagulation factors are produced in the liver. Loss of synthetic activity of hepatocytes results in hypofibrinogenemia and reduced levels of all other coagulation proteins. Typically PT and activated partial thromboplastin time are prolonged.
Reduced concentration of coagulation factors in blood: One should remember that most of the plasma coagulation factors are produced in the liver. Loss of synthetic activity of hepatocytes results in hypofibrinogenemia and reduced levels of all other coagulation proteins. Typically PT and activated partial thromboplastin time are prolonged. Thrombocytopenia: The low platelet count is caused by splenomegaly, which leads to a sequestration of platelets and their destruction in the spleen.
Thrombocytopenia: The low platelet count is caused by splenomegaly, which leads to a sequestration of platelets and their destruction in the spleen. Disseminated intravascular coagulation (DIC): Irregular blood flow through the liver makes the hepatocytes prone to ischemia and necrosis. Necrosis, typically precipitated by sudden onset of hepatic hypoperfusion (e.g., after massive bleeding from the esophageal varices), will result in a release of thromboplastin and activation of the coagulation cascade. Patients with cirrhosis are also prone to infections, which may potentiate DIC.
Disseminated intravascular coagulation (DIC): Irregular blood flow through the liver makes the hepatocytes prone to ischemia and necrosis. Necrosis, typically precipitated by sudden onset of hepatic hypoperfusion (e.g., after massive bleeding from the esophageal varices), will result in a release of thromboplastin and activation of the coagulation cascade. Patients with cirrhosis are also prone to infections, which may potentiate DIC.Massive uncontrollable bleeding is a major cause of death in patients with cirrhosis.
INFECTIOUS DISEASES
37 Discuss the most important infectious diseases affecting the liver
 Viral diseases: These diseases are most often caused by hepatotropic viruses (e.g., hepatitis virus A, B, and C) but also may occur in the course of other viral infections (e.g., herpes simplex and cytomegalovirus [CMV]).
Viral diseases: These diseases are most often caused by hepatotropic viruses (e.g., hepatitis virus A, B, and C) but also may occur in the course of other viral infections (e.g., herpes simplex and cytomegalovirus [CMV]). Bacterial diseases: These diseases are caused by ascending infection from the intestine or by hematogenous dissemination of bacteria from other organs.
Bacterial diseases: These diseases are caused by ascending infection from the intestine or by hematogenous dissemination of bacteria from other organs.39 Do all hepatitis viruses belong to the same group, and do they share the same structural properties?
40 Is liver biopsy useful for diagnosing acute viral hepatitis?
 The changes caused by various hepatotropic viruses are nonspecific. Microscopically, acute HAV cannot be distinguished from HBV or other hepatitides of this type.
The changes caused by various hepatotropic viruses are nonspecific. Microscopically, acute HAV cannot be distinguished from HBV or other hepatitides of this type. Serologic tests for hepatitis viruses, which are much more specific and less expensive, are the diagnostic method of choice for diagnosing viral hepatitides.
Serologic tests for hepatitis viruses, which are much more specific and less expensive, are the diagnostic method of choice for diagnosing viral hepatitides.< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree