Chapter 12 The Gastrointestinal System
1 What is the basic structure of the gastrointestinal (GI) system?
The entire GI tract has a relatively uniform structure and consists of four layers:
 Muscle layer (muscularis propria) composed predominantly of smooth muscle cells responsible for the peristaltic movement of these hollow organs
Muscle layer (muscularis propria) composed predominantly of smooth muscle cells responsible for the peristaltic movement of these hollow organs Adventitia or serosa forming the outer layer (In the esophagus, the adventitia is a connective tissue structure linking it with other thoracic organs. The external surface of the stomach and small and large intestines is covered with serosa, a layer of peritoneum continuous with the peritoneum covering the other parts of the abdominal cavity and other organs, such as the liver and the spleen.)
Adventitia or serosa forming the outer layer (In the esophagus, the adventitia is a connective tissue structure linking it with other thoracic organs. The external surface of the stomach and small and large intestines is covered with serosa, a layer of peritoneum continuous with the peritoneum covering the other parts of the abdominal cavity and other organs, such as the liver and the spleen.)2 What are the main diseases of the GI system?
 Inflammatory diseases, usually caused by infections but often of unknown etiology (e.g., inflammatory bowel disease)
Inflammatory diseases, usually caused by infections but often of unknown etiology (e.g., inflammatory bowel disease) Functional disorders affecting the digestion, absorption of nutrients, or motility of the intestines
Functional disorders affecting the digestion, absorption of nutrients, or motility of the intestines3 Discuss the possible consequences of abnormal development of the GI system
 Atresia (absence of lumen; The normal GI system is a tube that develops from cords of embryonic cells. The cells forming the central part of these cords undergo apoptosis, and a lumen is thus formed. If the centrally located cells do not undergo apoptosis, the lumen never forms, and the affected part of the GI system will be atretic, i.e., unpassable.)
Atresia (absence of lumen; The normal GI system is a tube that develops from cords of embryonic cells. The cells forming the central part of these cords undergo apoptosis, and a lumen is thus formed. If the centrally located cells do not undergo apoptosis, the lumen never forms, and the affected part of the GI system will be atretic, i.e., unpassable.) Fistula (a connection between the lumen of the GI tract and another tubular system; e.g., an esophageal–tracheal fistula)
Fistula (a connection between the lumen of the GI tract and another tubular system; e.g., an esophageal–tracheal fistula)ESOPHAGUS
4 What are the main clinical symptoms and signs of esophageal disease?
 Dysphagia: Difficulty in swallowing. It may be caused by anatomic lesions (e.g., stricture, webs, and rings), cancer, or functional disorders (e.g., achalasia and paralysis).
Dysphagia: Difficulty in swallowing. It may be caused by anatomic lesions (e.g., stricture, webs, and rings), cancer, or functional disorders (e.g., achalasia and paralysis). Odynophagia: Pain on swallowing. It is a sign of esophageal lesions, such as gastroesophageal reflux disease (GERD) and infectious esophagitis caused by viruses or fungi.
Odynophagia: Pain on swallowing. It is a sign of esophageal lesions, such as gastroesophageal reflux disease (GERD) and infectious esophagitis caused by viruses or fungi.6 What are esophageal diverticula?
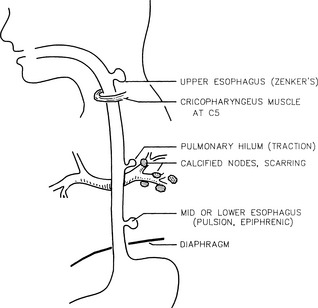
Diverticula are outpouchings of the wall of the esophagus. These outpouchings are classified on the basis of the following (Fig. 12.1):
 Location
Location Diverticula of the midportion of esophagus (traction diverticula due to mediastinal and bronchial lesions; e.g., scarring of lymph nodes in tuberculosis)
Diverticula of the midportion of esophagus (traction diverticula due to mediastinal and bronchial lesions; e.g., scarring of lymph nodes in tuberculosis)9 What is hiatal hernia?
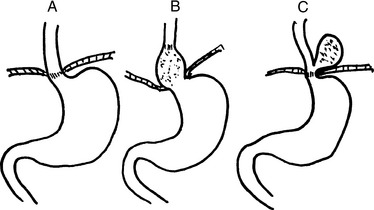
Hiatal hernia is a protrusion of the stomach above the diaphragm through a widened diaphragmatic hiatus. Hiatal hernias are quite common. Two forms are recognized (Fig. 12-2):
 Sliding hernia (90%): The gastroesophageal junction is pulled into the thorax and is found above the diaphragm. In most instances, it is asymptomatic and diagnosed accidentally during the workup of the patient for some other disease. It may be associated with GERD, heartburn, and dysphagia.
Sliding hernia (90%): The gastroesophageal junction is pulled into the thorax and is found above the diaphragm. In most instances, it is asymptomatic and diagnosed accidentally during the workup of the patient for some other disease. It may be associated with GERD, heartburn, and dysphagia. Paraesophageal hernia (10%): The gastroesophageal junction is in the normal location, but a portion of the stomach rolls up beside it into the thorax. In most instances, it is asymptomatic, but the invaginated gastric mucosa may become strangulated by the diaphragm.
Paraesophageal hernia (10%): The gastroesophageal junction is in the normal location, but a portion of the stomach rolls up beside it into the thorax. In most instances, it is asymptomatic, but the invaginated gastric mucosa may become strangulated by the diaphragm.12 Discuss the causes of GERD
 Temporary increase in intraabdominal pressure (e.g., after overeating or drinking carbonated drinks)
Temporary increase in intraabdominal pressure (e.g., after overeating or drinking carbonated drinks) Protracted LES relaxation and uncoordinated contraction due to the action of alcohol, fatty food, cigarettes, and drugs (e.g., morphine and diazepam)
Protracted LES relaxation and uncoordinated contraction due to the action of alcohol, fatty food, cigarettes, and drugs (e.g., morphine and diazepam)15 What are the causes of infectious esophagitis?
 Fungal infection: Candida albicans and other fungi may grow on the surface of the squamous epithelium, such as in the mouth or the vagina.
Fungal infection: Candida albicans and other fungi may grow on the surface of the squamous epithelium, such as in the mouth or the vagina. Viral infections: Herpes simplex virus or cytomegalovirus (CMV) infection typically occurs in immunosuppressed people.
Viral infections: Herpes simplex virus or cytomegalovirus (CMV) infection typically occurs in immunosuppressed people.16 What are the most common forms of chemical esophagitis?
 Hydrochloric acid: HCl regurgitated from the stomach is the most common cause of esophagitis in GERD.
Hydrochloric acid: HCl regurgitated from the stomach is the most common cause of esophagitis in GERD. Strong acids or lye: These chemicals cause erosive esophagitis. Children sometimes ingest these substances accidentally, and adults may drink them intentionally while trying to commit suicide.
Strong acids or lye: These chemicals cause erosive esophagitis. Children sometimes ingest these substances accidentally, and adults may drink them intentionally while trying to commit suicide. Cytotoxic drugs: Such drugs inhibit the proliferation of the esophageal epithelium and prevent or delay the repair of small ulcerations that develop during feeding. These ulcerations provide a route of entry for bacteria.
Cytotoxic drugs: Such drugs inhibit the proliferation of the esophageal epithelium and prevent or delay the repair of small ulcerations that develop during feeding. These ulcerations provide a route of entry for bacteria.21 List key facts about esophageal varices
 Dilatated veins bulge underneath the epithelium of the esophagus and can be recognized through esophagoscopy.
Dilatated veins bulge underneath the epithelium of the esophagus and can be recognized through esophagoscopy. Cirrhosis is the most common cause; thrombosis of portal vein and hepatocellular carcinoma are less common causes.
Cirrhosis is the most common cause; thrombosis of portal vein and hepatocellular carcinoma are less common causes.23 List the risk factors for esophageal cancer
 Environmental factors that could account for the higher incidence of esophageal cancer in areas of Asia and Africa (e.g., soil, tea, or food) have not been identified.
Environmental factors that could account for the higher incidence of esophageal cancer in areas of Asia and Africa (e.g., soil, tea, or food) have not been identified.STOMACH
30 Discuss why gastric erosions develop in acute gastritis
32 Describe the main forms of chronic nonerosive gastritis
 Hypertrophic gastritis (Menetrier disease; in this rare form of gastritis, the gastric mucosa has giant folds.)
Hypertrophic gastritis (Menetrier disease; in this rare form of gastritis, the gastric mucosa has giant folds.)33 Is it possible to distinguish type A and type B chronic gastritis in biopsy material examined microscopically?
34 Is it possible to clinically distinguish type A from type B chronic gastritis?
As stated previously, the histologic diagnosis of type B chronic gastritis depends primarily on finding H. pylori in the gastric biopsies. Because the gastroscopic findings are similar in both forms of gastritis and H. pylori cannot always be found in advanced stages of the disease, other tests (e.g., urea breath test or antibody test for H. pylori) must be performed. The most important aspects of type A and type B gastritis useful for distinguishing one form of gastritis from the other are listed in Table 12-1.
TABLE 12-1 Major Aspects of Type A And Type B Gastritis
| Feature | Type A Gastritis* | Type B Gastritis |
|---|---|---|
| Distribution of lesions | Fundus, diffuse | Pyloric antrum, focal |
| Gastric secretion | Reduced | Normal, +, or − |
| Antibodies to parietal cells | Yes | No |
| Other autoimmune diseases | Yes | No |
| Vitamin B12 (in serum) | Low | Normal |
| Pernicious anemia | + | − |
| Gastrin (in serum) | Increased | Normal |
| Antibodies to Helicobacter pylori | − | + |
| Incidence | Less common | More common |
| Age dependence | Yes | Yes |
| Cancer risk | Increased | Increased |
* Type A gastritis is associated with four As: autoimmune disease, antibodies to pyloric cells, anemia (pernicious), and achlorhydria (reduced hydrochloric acid secretion).
37 Which factors play a role in the development of peptic ulcers?
Peptic ulcer is a multifactorial disease, and several factors contribute to its pathogenesis:
 Infection: H. pylori is found in 90% of duodenal and 65% of gastric ulcer patients. H. pylori secretes urease, protease, and phospholipases that may cause mucosal injury and may serve as “barrier breakers,” facilitating the chemical injury of mucosal cells. Eradication of H. pylori infections contributes to the healing of peptic ulcers.
Infection: H. pylori is found in 90% of duodenal and 65% of gastric ulcer patients. H. pylori secretes urease, protease, and phospholipases that may cause mucosal injury and may serve as “barrier breakers,” facilitating the chemical injury of mucosal cells. Eradication of H. pylori infections contributes to the healing of peptic ulcers. Neuroendocrine factors: The secretion of gastric juices is under neuroendocrine control, which becomes dysregulated in peptic ulcer patients. Stress, nervous tension (type A personality), and endocrine disorders have been implicated in the pathogenesis of peptic ulcers, but the exact role of these putative insults is not known. For example, the hypersecretion of hormones such as corticosteroids and gastrin is associated with peptic ulcers in hormonal hypersecretion syndromes such as Cushing and Zollinger–Ellison syndromes, respectively. However, there is no definitive evidence that these hormones play a role in the pathogenesis of “garden variety” solitary peptic ulcers. Vagotomy (excision of the vagus nerve) is used only in the treatment of complicated persistent ulcers resistant to other treatment modalities.
Neuroendocrine factors: The secretion of gastric juices is under neuroendocrine control, which becomes dysregulated in peptic ulcer patients. Stress, nervous tension (type A personality), and endocrine disorders have been implicated in the pathogenesis of peptic ulcers, but the exact role of these putative insults is not known. For example, the hypersecretion of hormones such as corticosteroids and gastrin is associated with peptic ulcers in hormonal hypersecretion syndromes such as Cushing and Zollinger–Ellison syndromes, respectively. However, there is no definitive evidence that these hormones play a role in the pathogenesis of “garden variety” solitary peptic ulcers. Vagotomy (excision of the vagus nerve) is used only in the treatment of complicated persistent ulcers resistant to other treatment modalities. Local mucosal factors: Drugs such as NSAIDs reduce the secretion of prostaglandins and damage the mucosal barrier. Alcohol, spicy food, and substances that stimulate acid secretion may play a pathogenetic role. Antacid treatment and suppression of gastric acid with histamine-2 blockers promote healing of ulcers. There is no evidence that dietary modification is helpful in the treatment of peptic ulcer disease.
Local mucosal factors: Drugs such as NSAIDs reduce the secretion of prostaglandins and damage the mucosal barrier. Alcohol, spicy food, and substances that stimulate acid secretion may play a pathogenetic role. Antacid treatment and suppression of gastric acid with histamine-2 blockers promote healing of ulcers. There is no evidence that dietary modification is helpful in the treatment of peptic ulcer disease.38 Where are peptic ulcers most often located?
 Duodenal ulcers are more common than gastric ones (4:1) and are located in the proximal area just beyond the pylorus.
Duodenal ulcers are more common than gastric ones (4:1) and are located in the proximal area just beyond the pylorus. Gastric ulcers are located on the lesser curvature, most often at the junction of the body and pyloric antrum.
Gastric ulcers are located on the lesser curvature, most often at the junction of the body and pyloric antrum.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree