Fig. 36.1
A large necrotic metastasis which has necessitated a nephrectomy after chemotherapy. The testis is also seen below with a much smaller mass showing teratoma
The techniques used therefore have to vary according to circumstance. Margin positivity for tumor is rare in RPLNDs but it is a poor prognostic factor [3]. Therefore, we recommend inking any specimens with enlarged lymph nodes. Sampling of the enlarged nodes should be extensive: at least 1 block/cm, as small tumor foci can be missed in large necrotic foci.
It is also very important to have adequate clinical history and the reason for the RPLND. This should include the serum markers, as fairly small tumor deposits can produce substantial amounts of β-HCG and AFP.
Metastatectomies for germ cell tumor in other organs are also increasing in frequency. Lung and liver metastases may all be resected, especially if the clinicians believe that they consist of mature teratoma. Again, close inspection, inking of margins, and generous blocking are good practice.
Microscopy of Postchemotherapy Germ Cell Tumors
In most cases the microscopic examination of most RPLNDs is relatively straightforward, as the vast majority will show either necrosis or teratoma. Below we describe the varied findings in RPLNDs.
Necrosis
Necrosis is the most frequent RPLND finding. The necrotic areas are often surrounded by a prominent infiltrate of foamy macrophages, scattered hemosiderin, and an active fibroblastic proliferation. Within the necrotic foci, pyknotic nuclei in the ghost-like outlines of tumor cells may be seen, often surrounding vessels (Fig. 36.2). These foci often retain their immunophenotype (Fig. 36.3). These semideposits or unviable deposits should not be considered evidence of persistent germ cell tumor. Only cells with intact nuclei and well-preserved chromatin pattern and cytoplasm should be considered as viable.
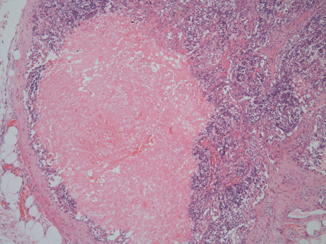
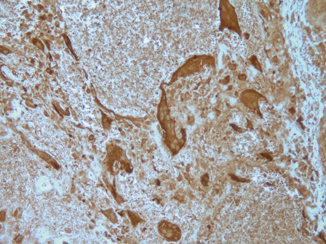
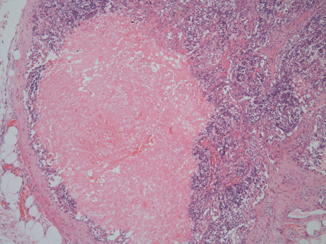
Fig. 36.2
Postchemotherapy necrosis within a lymph node. Ghost outlines of the malignant tumor are seen
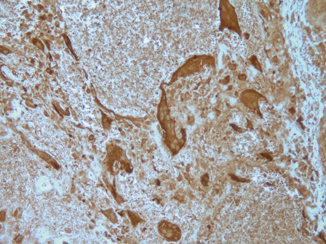
Fig. 36.3
Immunohistochemistry for β-HCG on this necrotic postchemotherapy metastasis can still highlight syncytiotrophoblastic cells
Mature Teratoma
This is the second most frequent finding at RPLND. The presence of teratoma is often expected on macroscopy as the lymph nodes are often multicystic (Fig. 36.4) and filled with clear or brown fluid. On close inspection some solid areas can have the glistening surface of cartilage.


Fig. 36.4
Macroscopic appearance of postchemotherapy retroperitoneal lymph nodes showing extreme cystic change. The lymph nodes are involved by teratoma
Microscopically, the tumor shows a typical mixed organoid pattern with epithelial and stroma elements, as seen in testicular teratoma (Fig. 36.5).
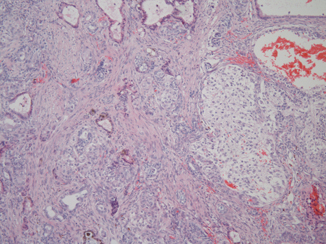
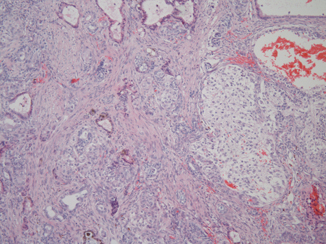
Fig. 36.5
Microscopic features of a solid area from a postchemotherapy teratoma. Note the organoid arrangement of components with many epithelial and stromal elements
Persistent teratoma often shows significant cytological atypia in both mesenchymal and epithelial components. In the absence of stromal invasion or overgrowth, with preservation of a typical organoid appearance by the teratoma the presence of cytologic atypia has no adverse significance and can be ignored [4].
Residual “Malignant” Germ Cell Tumor
This is a relatively unusual finding and is often suspected due to raised serum markers. Most cases will only have small amounts of tumor present, as cases where the serum markers are very high will not be considered for resection.
Embryonal carcinoma is similar in appearance to that seen in the testis (Fig. 36.6), though it should be noted that CD30 is often negative in these tumors after chemotherapy [5]. OCT3/4 is positive, however, and morphology should be sufficient to differentiate embryonal carcinoma from seminoma.
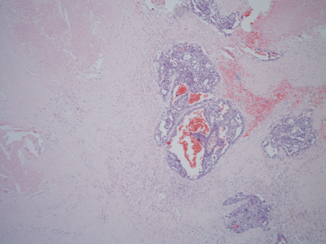
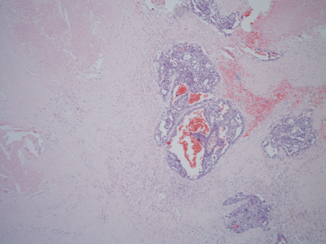
Fig. 36.6
Residual embryonal carcinoma after chemotherapy, which is here surrounded by substantial necrosis
Seminoma in RPLNDs is unusual: often seminoma is highly infiltrative in the retroperitoneum, and resection is surgically challenging, and imaging often shows tumor wrapped around major vessels. In any chemo- or radioresistant seminoma it is worth taking a second look at the tumor to exclude the possibility of a malignant Sertoli cell tumor that has been erroneously diagnosed.
Yolk sac tumor has a protean nature, and in late recurrences, it tends to show even more unusual patterns, especially the glandular form which may resemble an adenocarcinoma and lead to misdiagnosis (Fig. 36.7). As long as the pathologist is aware of a high serum AFP, this should not occur; however, the morphological appearances may be misleading and immunohistochemistry for AFP may be patchy, though glipican-3 now provides a more sensitive immunomarker [6]. The glandular type of yolk sac tumor appears to be particularly resistant to chemotherapy while the hepatoid form is more common in metastases (Fig. 36.8).
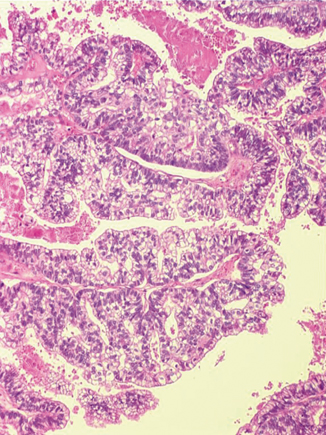
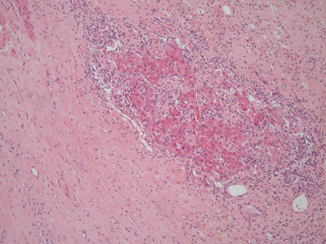
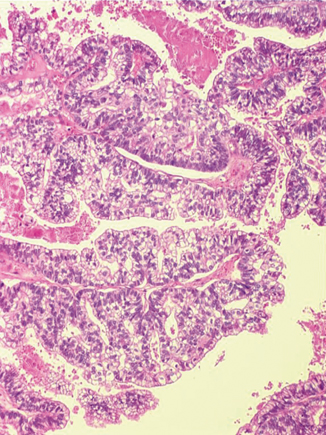
Fig. 36.7
Glandular type yolk sac tumor. This is usually seen in late recurrences and is usually chemoresistant
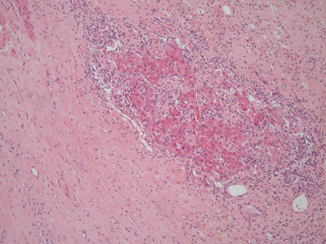
Fig. 36.8
A small amount of hepatoid type yolk sac tumor in the edge of a largely necrotic postchemotherapy germ cell tumor
Choriocarcinomas may be difficult to diagnose without knowledge of the serum markers. They may lack a well-defined biphasic pattern and mainly consist of mononucleated trophoblast cells alone. As they frequently metastasize to unusual sites, they may be seen by non-genito-urinary pathologists, and if a history is not available, misdiagnosis is not infrequent. We have seen choriocarcinoma misdiagnosed as squamous cell carcinoma on a number of occasions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


