Techniques for Imaging-Guided Needle Core Biopsy
D. David Dershaw
Various techniques for imaging-guided needle core biopsy are available, and others are in development that make it possible to remove varying amounts of breast tissue percutaneously under imaging guidance. The menu of procedures from which the biopsy technique is chosen in any individual case is best understood by separating the imaging modality used to guide the biopsy probe into the lesion from the actual biopsy instrument used to retrieve tissue from the breast. For the pathologist, only the latter half of this process, the biopsy probe technology, may be evident. However, constraints dictated by the patient or by lesion configuration and conspicuity under varying imaging technologies can influence the physician’s selection of the biopsy probe, and thereby the character of the specimen which is obtained.
Before a decision is made to perform a biopsy, a complete imaging workup of nonpalpable lesions should be undertaken (1). It should not be the role of the biopsy procedure to replace such a workup. If a lesion presents as a palpable mass, the algorithm of the workup is modified by findings on physical examination. Because the development of a new, palpable breast mass is indicative of lesion growth, biopsy is often indicated for these lesions, unless it can be demonstrated that the mass is a cyst.
IMAGING TECHNOLOGIES FOR BREAST BIOPSY
Stereotactic Imaging
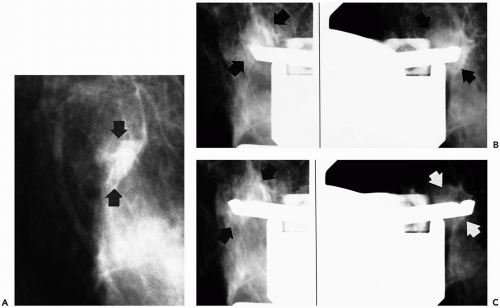
Stereotactic imaging uses radiographic (mammographic) imaging to triangulate the location of a lesion within the breast. Equipment is designed to obtain equally angled radiographic views of the suspected lesion (Fig. 30.1). When the lesion is located on these images, its depth from the skin surface can be calculated based on the following formula:
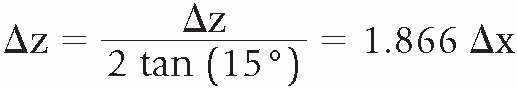
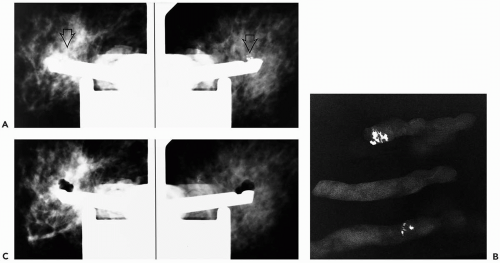
As the x-ray beam is angled along the x-axis, or horizontal axis, there will be increasing change in the position of the lesion as it is located more deeply in the breast. Fifteen degrees is the standard angulation of the x-ray beam, although some manufacturers have altered this, and, for equipment in which the x-ray tube is angled more steeply, the denominator of the formula is altered appropriately. Based on this formula, the z-axis, or depth of the lesion within the breast, is calculated (2). The vertical location of lesion, or y-axis, as well as the location of the lesion on the horizontal axis or x-axis, is evident on the nonoblique (0° angulation) scout view of the breast. This view is also needed to determine whether the lesion is in the field of view of the stereotactic unit. Calculation of the position of lesion in the x-, y-, and z-axes is accomplished by feeding the location of the site, at which the biopsy probe is to be positioned on the equally angled oblique or stereotactic views, into a computer incorporated into the biopsy unit (Fig. 30.2).
Because the images for stereotactically guided biopsy are obtained with x-rays, as are mammograms, any lesion seen mammographically can potentially be sampled with stereotactic technique. Calcifications, which are not reliably seen with sonography or other imaging modalities, are
readily imaged with stereotaxis. Abnormalities that are characterized by calcifications on the mammogram should therefore be sampled using this technology (3). Lesions that are seen with only sonography or magnetic resonance (MR) imaging cannot be sampled stereotactically with current technology.
readily imaged with stereotaxis. Abnormalities that are characterized by calcifications on the mammogram should therefore be sampled using this technology (3). Lesions that are seen with only sonography or magnetic resonance (MR) imaging cannot be sampled stereotactically with current technology.
 Figure 30.2 Stage of the stereotactic table positions the needle accurately within the breast. The gun is attached to the upper portion of this device, and the biopsy probe can be positioned manually or automatically at the desired x-, y-, and z-axes, as shown in Figure 30.4. This stage is positioned between the x-ray tube and the breast, which is compressed against the imaging receptor. |
Although mammographic abnormalities can be imaged with stereotaxis, in some situations, these may not be easily appreciated during the biopsy procedure. The field of view during the procedure can be as small as 4 × 5 cm; in most units with digital imaging, the field of view is 5 × 5 cm. This sometimes limits the ability of the physician to easily correlate the lesion seen during the biopsy with that found when the full breast is imaged with x-rays for a mammogram. On occasion, biopsy of the wrong lesion can result from this limited field of view. Areas of asymmetric tissue are particularly difficult to localize in this setting. Architectural distortion can also be very difficult to localize. In some situations, it may be desirable to sample these lesions with preoperative needle localization rather than stereotactically guided core technique.
Digital Imaging
The use of digital imaging can influence the ability to localize areas during stereotactic biopsy. With digital imaging, information in the image can be collected and stored electronically, so that it is not necessary to rely on film development. The x-ray image of the breast is therefore more rapidly available and can be viewed in as little as 3 seconds rather than the 3 to 5 minutes required with film (4). One obvious advantage of this is that the patient is less likely to move during the procedure, so that the initial calculation of the lesion location in the field of view remains accurate. Patient tolerance is increased with shorter duration of the procedure.
Digital imaging also enables the image to be windowed and leveled, with adjustment of brightness and darkness, as well as the amount of contrast in the picture. Although some lesions become more conspicuous with such manipulation, others can become more difficult to differentiate from background breast tissue. Although this situation should be unusual, it can result in biopsy of the wrong breast lesion. Digital imaging technology also sacrifices some image resolution. For this reason, some fine detail readily appreciated with film mammography can be difficult or impossible to appreciate digitally. This issue becomes important when faint microcalcifications are the biopsy target and the ability to localize these lesions accurately is limited.
CALCIFICATIONS
When calcifications are sampled under stereotactic imaging, confirmation that they have been sampled should be obtained with specimen radiography. This is comparable to documenting removal of a lesion during a needle-localized breast biopsy procedure. If calcifications are not present in the initial cores removed from the breast, it is routine to continue sampling the breast until calcifications are obtained (Fig. 30.3). However, prolongation of the biopsy procedure can be limited by patient tolerance. Also, if calcifications are not present in the initial 5 to 10 specimens, it is unlikely that continued attempts to obtain calcifications will be successful, particularly with gun-needle biopsy probes. This is because progressive destruction of breast architecture and hemorrhage into the area resulting from repeated passage of the core needle through a small volume of tissue decreases the ability to retrieve a cohesive piece of tissue from a site within the breast. The failure to obtain calcifications in lesions in which they have been characterized mammographically can considerably diminish the likelihood of making a diagnosis. In the assessment of any single core, this has been shown to decrease the ability to make a diagnosis based on that core from 82% to 40% (5). The significance of retrieval of calcification in core biopsy specimens appears to be an indicator that the correct site
within the breast has been sampled, even though the abnormality containing the lesion can be uncalcified. Failure to retrieve calcifications strongly suggests that the correct site in the breast has not been sampled.
within the breast has been sampled, even though the abnormality containing the lesion can be uncalcified. Failure to retrieve calcifications strongly suggests that the correct site in the breast has not been sampled.
It is reasonable for the pathologist to expect that the physician performing the biopsy will communicate whether the lesion in question contained calcifications and whether calcifications were obtained at the time of biopsy. If desired, it should be possible for cores containing calcification to be submitted separately from those without calcium. As with specimens obtained at surgical biopsy, it is possible to obtain x-ray images of the paraffin block if calcifications are not appreciated on routine sectioning. This can be done to guide the pathologist in obtaining further sections for microscopic examination. It is not routine for specimen radiography of uncalcified lesions to be performed, as it is in surgical biopsy. Successful biopsy of these lesions is documented by imaging the location of the needle and its relationship to the breast mass after tissue has been obtained. X-ray imaging of the paraffin block to localize the area of interest within the fixed cores also has not been reported. Of course, the final determination of the success of the biopsy for any type of lesion awaits histopathologic interpretation.
UPRIGHT VERSUS PRONE DEDICATED STEREOTACTIC UNITS
Current equipment design offers two major configurations of stereotactic biopsy units. In one of these, the add-on or upright unit, a stereotactic device attaches to a mammographic unit, and the patient is sitting during the biopsy procedure. In some instances, this equipment can also be used to biopsy the patient while she is lying in a decubitus position. In the other type of equipment, the dedicated stereotactic biopsy table, the patient lies prone on a table under which a mammographic unit is located; this type is designed exclusively to perform breast biopsies.
Upright equipment is designed to be attached to a mammographic unit, modifying it so that it can be used to perform stereotactic biopsies (6). This equipment is removable, so that the unit can be used for regular mammography. With this equipment design, a room need not be dedicated to the performance of stereotactic breast biopsies. Upright equipment design makes it possible to obtain biopsy specimens of certain lesions located in the posterior breast near the chest wall or in the axilla, areas that are sometimes inaccessible when tables and the prone position are used. The price of this equipment is considerably less than that of the dedicated table, about $35,000 versus $140,000, so that facilities with a limited budget or space can more readily perform stereotactic biopsies with this equipment than with tables (7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree