HO is a 50-year-old, 75-kg (height = 5 ft 10 in) male renal transplant patient 2 days posttransplant surgery. The patient’s liver function tests are normal. Suggest an initial oral tacrolimus dose designed to achieve a steady-state tacrolimus trough blood concentration equal to 15 ng/mL.
1. Estimate clearance according to disease states and conditions present in the patient.
The mean tacrolimus clearance for adult patients is 0.06 L/h/kg. The tacrolimus blood clearance for this patient is expected to be 4.5 L/h: Cl = 0.06 L/h/kg • 75 kg = 4.5 L/h.
2. Compute dosage regimen.
A 12-hour dosage interval will be used for this patient. (Note: ng/mL = μg/L and this concentration was substituted for Css in the calculations so that unnecessary unit conversion was not required. Also, a conversion constant of 1000 μg/mg is used to change the dose amount to mg.) The dosage equation for oral tacrolimus is: D = (Css • Cl • τ)/F = (15 μg/L • 4.5 L/h • 12 h)/(0.25 • 1000 μg/mg) = 3.2 mg, rounded to 3 mg every 12 hours.
Tacrolimus concentrations would be obtained on a daily basis with steady-state expected to occur in about 3 days (5 half-lives = 5 • 12 h = 60 h).
Literature-Based Recommended Dosing
Because of the large amount of variability in tacrolimus pharmacokinetics, even when concurrent disease states and conditions are identified, many clinicians believe that the use of standard tacrolimus doses for various situations is warranted. Indeed, most transplant centers use doses that are determined using a tacrolimus dosage protocol. The original computation of these doses were based on the Pharmacokinetic Dosing method described in the previous section, and subsequently modified based on clinical experience. In general, the expected tacrolimus steady-state concentration used to compute these doses is dependent upon the type of transplanted tissue and the posttransplantation time line. Generally speaking, initial oral doses of 0.1-0.3 mg/kg/d given twice daily are needed to achieve therapeutic tacrolimus steady-state concentrations.1,5 Usual initial continuous infusion intravenous doses are 0.05-0.1 mg/kg/d.1,5 For patients with liver dysfunction, these doses may be reduced by 25%-50%.29,34,35 Initial doses for children undergoing liver transplantation are 0.15-0.2 mg/kg/d orally administered twice daily or 0.03-0.15 mg/kg/d by continuous intravenous infusion. If the drug is started intravenously, pediatric patients are converted to an oral doses as soon as feasible.38 To illustrate how this technique is used, the same patient examples utilized in the previous section will be repeated for this dosage approach for comparison purposes.
USE OF TACROLIMUS CONCENTRATIONS TO ALTER DOSES
Because of the large amount of pharmacokinetic variability among patients, it is likely that doses computed using patient population characteristics will not always produce tacrolimus concentrations that are expected or desirable. Because of pharmacokinetic variability, the narrow therapeutic index of tacrolimus, and the severity of tacrolimus adverse side effects, measurement of tacrolimus concentrations is mandatory for patients to ensure that therapeutic, nontoxic levels are present. In addition to tacrolimus concentrations, important patient parameters (transplanted organ function tests or biopsies, clinical signs and symptoms of graft rejection or graft-versus-host disease, potential tacrolimus side effects, etc) should be followed to confirm that the patient is responding to treatment and not developing adverse drug reactions.
For most patients, predose steady-state trough tacrolimus concentrations are typically measured. Since alternate methods to monitor cyclosporine concentrations have met with some success, investigators have begun suggesting similar methods for tacrolimus. Of these methods, estimation of tacrolimus area under the concentration-time curve (AUC) using several measured steady-state concentrations is the one that is gaining use in some transplant centers.
When tacrolimus concentrations are measured in patients and a dosage change is necessary, clinicians should seek to use the simplest, most straightforward method available to determine a dose that will provide safe and effective treatment. In most cases, a simple dosage ratio can be used to change tacrolimus doses assuming the drug follows linear pharmacokinetics. Sometimes, it is useful to compute tacrolimus pharmacokinetic constants for a patient and base dosage adjustments on these. In this case, it may be possible to calculate and use pharmacokinetic parameters to alter the tacrolimus dose. Another approach involves measuring several postdose steady-state tacrolimus concentrations to estimate the area under the concentration-time curve (AUC) and adjusting the tacrolimus dose to attain a target AUC. Finally, computerized methods that incorporate expected population pharmacokinetic characteristics (Bayesian pharmacokinetic computer programs) can be used in difficult cases where concentrations are obtained at suboptimal times or the patient was not at steady-state when concentrations were measured.
Linear Pharmacokinetics Method
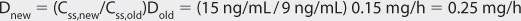
Assuming tacrolimus follows linear, dose-proportional pharmacokinetics,39 steady-state concentrations change in proportion to dose according to the following equation: Dnew/Css,new = Dold/Css,old or Dnew = (Css,new/Css,old)Dold, where D is the dose, Css is the steady-state concentration, old indicates the dose that produced the steady-state concentration that the patient is currently receiving, and new denotes the dose necessary to produce the desired steady-state concentration. The advantages of this method are that it is quick and simple. The disadvantage is steady-state concentrations are required.
Pharmacokinetic Parameter Method
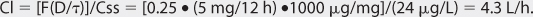
The Pharmacokinetic Parameter method of adjusting drug doses was among the first techniques available to change doses using drug concentrations. It allows the computation of an individual’s own, unique pharmacokinetic constants and uses those to calculate a dose that achieves desired tacrolimus concentrations. The pharmacokinetic parameter method requires that steady-state has been achieved and uses only a steady-state tacrolimus concentration. Tacrolimus clearance can be measured using a single steady-state tacrolimus concentration and the following formula for orally administered drug: Cl = [F(D/τ)]/Css, where Cl is tacrolimus clearance in L/h, F is the bioavailability factor for tacrolimus (F = 0.25), τ is the dosage interval in hours, and Css is the tacrolimus steady-state concentration in ng/mL, which also equals μg/L. If tacrolimus is administered intravenously, it is not necessary to take bioavailability into account: Cl = ko/Css, where Cl is tacrolimus clearance in L/h, ko is the tacrolimus infusion rate in mg/h, and Css is the tacrolimus steady-state concentration in ng/mL which also equals μg/L. Although this method does allow computation of tacrolimus clearance, it yields exactly the same tacrolimus dose as that supplied using linear pharmacokinetics. As a result, most clinicians prefer to directly calculate the new dose using the Simpler Linear Pharmacokinetics method. To demonstrate this point, the patient cases used to illustrate the Linear Pharmacokinetics method will be used as examples for the Pharmacokinetic Parameter method.
Area Under the Concentration-Time Curve Method
Some solid organ transplant centers believe that measurement or estimation of tacrolimus area under the concentration-time curve (AUC) is the best way to optimize tacrolimus therapy. While AUC can be measured using hourly postdose tacrolimus levels, studies have shown that there is a strong correlation between 3 and 4 tacrolimus concentrations and the total AUC. Based on this finding, most centers utilizing this method measure several steady-state tacrolimus concentrations and use a published regression equation determined in other patients receiving the same transplanted organ and similar drug therapy (to account for possible drug interactions) in order to convert the concentrations to an estimated AUC. Then, if necessary, adjust the tacrolimus dose using linear pharmacokinetics to achieve the target AUC: Dnew/AUCnew = Dold/AUCold or Dnew = (AUCnew/AUCold)Dold, where D is the dose, AUC is the steady-state area under the concentration-time curve, old indicates the dose that produced the steady-state area under the concentration-time curve that the patient is currently receiving, and new denotes the dose necessary to produce the desired steady-state area under the concentration-time curve.
There are many regression equations from which to choose based on the target transplant population and other concurrent therapy that may cause drug interactions with tacrolimus. The one used for the examples and problems in this book is for renal transplant patients treated with tacrolimus for at least 6 months that received other immunosuppressants (prednisone plus azathioprine).19 In this investigation, the steady-state AUC over the dosage interval [from time 0 hours (predose) to 12 hours after the dose, AUC0-12h] strongly correlated with four steady-state concentrations, and this relationship was used to adjust tacrolimus doses: AUC0-12h (in [ng • h]/mL) = 10 + (1.4 • C0h) + (0.8 • C1h) + (1.6 • C2h) + (5.5 • C4h), where C0h, C1h, C2h, C4h are steady-state tacrolimus concentrations in ng/mL obtained 0, 1, 2, and 4 hours, respectively, after a dose. The dose is then adjusted to produce a new steady-state AUC0-12h equal to 104 ± 33 (ng • h)/mL using linear pharmacokinetics.18
BAYESIAN PHARMACOKINETIC COMPUTER PROGRAMS
Computer programs are available that can assist in the computation of pharmacokinetic parameters for patients. The most reliable computer programs use a nonlinear regression algorithm that incorporates components of Bayes theorem. Nonlinear regression is a statistical technique that uses an iterative process to compute the best
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree