Synovial Sarcoma
Cyril Fisher, MD, DSc, FRCPath
Key Facts
Terminology
Name is historical accident, as tumor does not arise from or differentiate toward synovium
Mesenchymal spindle cell tumor with variable epithelial differentiation, including gland formation
Characterized by specific chromosomal translocation t(X;18)(p11;q11)
Clinical Issues
Accounts for 5-10% of all soft tissue sarcomas
Can occur in any anatomic location
Majority in young adults 15-35 years
More frequent in males
Presence of biphasic pattern does not influence behavior
Poorly differentiated histology worsens prognosis
Image Findings
Scattered calcifications
Microscopic Pathology
Sheets of uniform small spindle cells with ovoid nuclei and scanty cytoplasm
If pleomorphic, consider other diagnoses
Focal epithelial differentiation
Glandular structures
Solid cords or nests
Never low-grade tumor
Ancillary Tests
Epithelial markers focally positive
If CD34(+), consider other diagnoses
Identification of t(X;18)(p11.q11) and SS18-SSX fusions diagnostic
TERMINOLOGY
Abbreviations
Synovial sarcoma (SS)
Synonyms
Terms no longer commonly used
Synovial cell sarcoma
Malignant synovioma
Definitions
Mesenchymal spindle cell tumor with variable epithelial differentiation, including gland formation
Characterized by specific chromosomal translocation t(X;18)(p11;q11)
Name is historical accident
Tumor does not arise from or differentiate toward synovium
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Very rare examples arise in field of prior irradiation
1 case reported at site of metal prosthetic implant
Acquired Genetic Abnormality
Translocation between chromosomes × and 18
CLINICAL ISSUES
Epidemiology
Incidence
5-10% of all soft tissue sarcomas
Can occur in any anatomic location; rare in joints
90% in extremities
Most common around knee region
In periarticular soft tissue and tendon sheaths
Subset in head and neck
Parapharynx, oral cavity, tonsil
Rare subsets
Abdominal wall
Retroperitoneum/omentum
Mediastinum
Intravascular, intraneural
Age
Majority in young adults 15-35 years
Rare over age of 50
Gender
More frequent in males
Presentation
Slow growing
Deep mass, with local pressure effects
Painful mass
> 1/2 of cases
Painless mass
< 1/2 of cases
Natural History
Can be present for long period: 2-20 years
Local recurrence frequent especially if inadequate resection
Metastasis in 45% of cases
Lung (95%)
Late metastases can appear after many years
Bone
Lymph nodes (10%)
Treatment
Options, risks, complications
Based on
Size, location of primary tumor, and stage
Adjuvant therapy
Preoperative irradiation for large or initially unresectable primary tumor
Chemotherapy for disseminated disease
Ifosfamide or doxorubicin
Combination chemotherapy
Surgical approaches
Prognosis
5-year survival (50-85%)
Presence of biphasic pattern does not influence behavior
Favorable prognostic factors
Small tumor size (< 5 cm)
Young age, especially childhood
Calcifying/ossifying variant (not in all series)
Possibly tumors with SSX2 gene rearrangement (not in all series)
Adverse prognostic factors
Age > 40 years
Large tumor size (> 5 cm)
Poorly differentiated histology
IMAGE FINDINGS
General Features
Best diagnostic clue
Scattered calcifications
Circumscribed mass
Location
1st consideration for tumors around knee
Size
Variable
Usually > 5 cm in diameter
Can be very small
Rarely > 10 cm, though up to 15 cm described
Morphology
Circumscribed
Specimen Radiographic Findings
Small scattered calcifications
MACROSCOPIC FEATURES
General Features
Circumscribed tan tumor mass
Soft cut surface
Cysts occasionally seen
Smooth walled
Contain mucoid fluid or blood
Focal necrosis and hemorrhage in poorly differentiated tumors
Sections to Be Submitted
Sample margins and representative sections of tumor
Size
Wide range from minute (< 1 cm) to 15 cm diameter
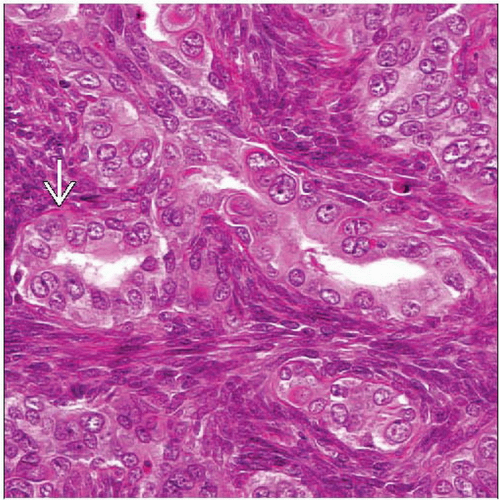
MICROSCOPIC PATHOLOGY
Histologic Features
Sheets of uniform small spindle cells with ovoid nuclei and scanty cytoplasm
Focal epithelial differentiation
Glandular structures
Solid cords or nests
Intercellular stroma minimal except in
Occasional hyalinizing monophasic SS
Calcifying variants
Recurrences after irradiation
Lymphatic/Vascular Invasion
Rarely
Margins
Infiltrative microscopically, pseudocapsule of adjacent tissue
Lymph Nodes
Metastases in up to 10% of cases
Predominant Pattern/Injury Type
Predominant Cell/Compartment Type
Spindle and epithelioid
Small round
Grade
Either grade II or III; never grade I
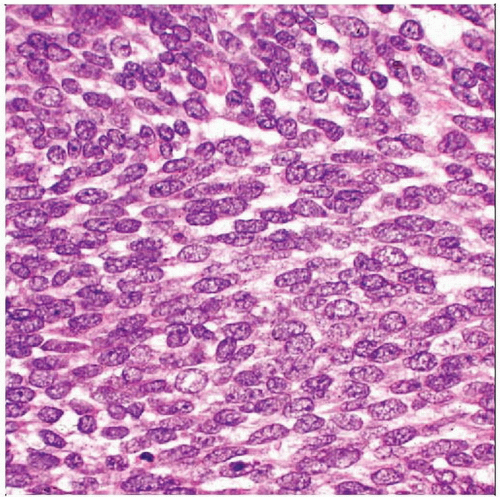
ANCILLARY TESTS
Cytology
Diagnosis can be made on cell-rich aspirates
Biphasic pattern rarely seen
Monophasic SS
Cellular clusters
Hyperchromatic, overlapping short ovoid nuclei
Inconspicuous nucleoli
Scanty cytoplasm
Mast cells, calcifications