Surgical Anatomy of the Liver and Bile Ducts
Chung Mau Lo
Kelvin K. Ng
The Liver and Biliary Tract
Introduction
The liver is the largest internal organ in the body and accounts for about 2% of the body weight of an adult. It has a unique dual blood supply and an intimate relationship with the bile ducts. These, together with the frequent occurrence of anatomic variants and the discordance between its external morphology and internal segmentation have made understanding the surgical anatomy of the liver and bile ducts challenging. The surgical anatomy of the liver and bile ducts is based on a clear comprehension of the liver’s embryology, natural segmentation, and various congenital variants. A better understanding of the surgical anatomy has contributed to the rapid advancement in hepatobiliary surgery and vice versa. The advent of living donor liver transplantation in the last two decades, for example, has brought about a more detailed understanding of the anatomical and functional aspects of the hepatic vasculature and bile ducts and has reset the standard for the safety of liver surgery.
Despite the progress made in our knowledge in surgical anatomy of the liver and bile ducts, the terminology in many textbooks remains confusing and is a major source of challenge in surgical training. In this chapter, we try to avoid excessive review of the development of the terms used in the literature and minimize the description of classic but confusing definitions and nomenclatures. Instead, we focus on the modern concept of the surgical anatomy with a set of widely adopted standard terminology. In each section, following a description of the anatomy, the surgical relevance in the operating room will be highlighted and discussed.
The segmental anatomy of the liver and bile duct is more pertinent in liver surgery but an understanding of the surface anatomy and the relationship between the external landmarks and the internal structures remains essential. The surface of the liver is covered by a thin fibrous capsule (Glisson’s capsule), which is an extension of the visceral peritoneum. It covers the entire organ except the bare area at the back where the organ lies in contact with the inferior vena cava (IVC) and the right hemidiaphragm, and the gallbladder fossa with the liver hilum (porta hepatis) below where the capsule extends to envelope the hepatic artery, portal vein, and bile duct as these structures enter the liver. The shape of the liver is molded by the adjacent organs. When seen at laparotomy, it has three surfaces. The anterosuperior surface is smooth and covered by the peritoneum up to the attachment of the triangular ligaments and the anterior layer of the coronary ligament. It is related to the inferior surface of the diaphragmatic dome. The posterior surface, which includes the bare area, is largely retroperitoneal. It is related to the vertical part of the diaphragm, the retrohepatic part of the IVC, the right adrenal gland, and the upper pole of the right kidney. The caudate lobe projects from this surface as an appendage sitting on the surface of the IVC. The inferior or visceral surface has an irregular contour as it lies in contact with a number of organs, including the right anterior aspect of the stomach, superior part of the duodenum, head of pancreas, gallbladder, common bile duct, hepatic flexure of the colon, right kidney, and right adrenal gland.
The liver is suspended from the anterior abdominal wall and the diaphragm by four peritoneal attachments, which are commonly referred to as ligaments. The falciform ligament is a crescent-shaped fold, which runs between the anterior abdominal wall above the umbilicus and the anterior surface of the liver. It serves as the surface landmark for the border between the left medial and left lateral sections. The anterior and posterior layers of the coronary ligament mark the limit of the bare area as the peritoneum passes from the body wall to the liver surface. The right and left triangular ligaments are formed by the lateral unification of the layers of the coronary ligament on both sides. At where the bare area of the liver lies in contact with the diaphragm and the IVC, the liver is suspended by loose connective tissue and by the three hepatic veins. There are other ligamentous structures, which are attached to the liver. The round ligament (ligamentum teres) contains the obliterated left umbilical vein and runs in the free edge of the falciform ligament from the umbilicus to the termination of the left portal vein. The hepatoduodenal ligament contains the hepatic artery, portal vein, and bile duct as these structures run from the upper border of the first part of the duodenum to enter the liver hilum. The ligamentum venosum contains the obliterated ductus venosum that connects the left portal vein to the junction of the left hepatic vein and the IVC in the fetus. It lies on a groove that separates the caudate lobe of liver underneath from the left liver in front. The hepatogastric omentum (lesser omentum) comprises two layers of peritoneal reflection that connect this groove to the lesser curve of the stomach.
The term “hepatic fissures” is confusing as these fissures are based largely on their anatomical relation to the three hepatic veins, not on their external appearance. The umbilical fissure is the only fissure that can be seen on the surface. It forms a deep groove on the inferior surface between the left medial and the left lateral sections that contains the umbilical portion of the left portal vein as it runs an unusually long extrahepatic course, giving off branches to both sides and terminating blindly in the round ligament. The umbilical fissure is marked superficially by the attachment of
the falciform and round ligaments at its inferior border.
the falciform and round ligaments at its inferior border.
Traditionally, based on the external appearance and the attachment of ligaments, the liver is divided into four anatomical lobes: right, left, quadrate, and caudate. With better understanding of the segmental anatomy of the liver, however, it becomes clear that these terms have very little clinical relevance and are used in different ways by various anatomists and surgeons. Hence, further description and use of these terms except in reference to the caudate lobe should be avoided.
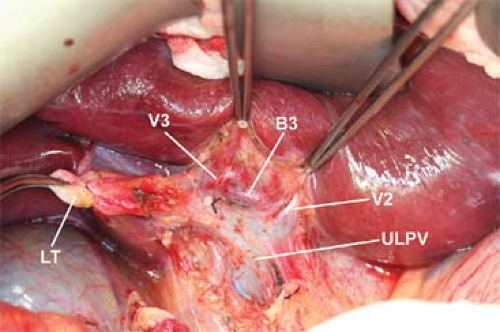
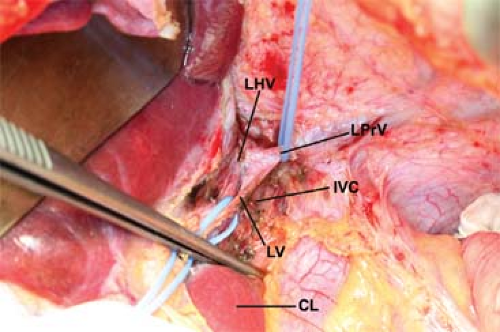
In the Operating Room
Knowledge of the surface anatomy is essential not only for hepatobiliary surgery, but also for any operation around the liver. Mobilization of either side of the liver requires division of various peritoneal attachments such as the falciform ligament, triangular ligaments, and coronary ligament, which are generally avascular. Such division can be done with diathermy except for the round ligament. In patients with portal hypertension, however, venous collaterals may form particularly at the tip of the triangular ligaments and these will have to be ligated before division. Two ligamentous structures provide landmarks for identification of vital structures in hepatobiliary surgery. The round ligament approach allows rapid access to the left portal vein and the left duct, which is a prime location for high bilioenteric anastomosis (Fig. 1). The ligamentum venosum marks the left hepatic vein and is important when extrahepatic isolation of the left hepatic vein is required when performing left hepatectomy. Identification and division of the ligamentum venosum at where it attaches to the left hepatic vein will expose the junction of the left hepatic vein with the IVC at the upper border of the caudate lobe (Fig. 2).
The division of the liver into functional units or segments according to arterial, portal venous blood supply, biliary drainage, and hepatic venous drainage forms the anatomical basis for modern hepatic surgery. Although the concepts of hepatic segmentation as described by Couinaud, Healey and Schroy, and Bismuth, respectively, are close and widely adopted, the terminology is confusing. The Brisbane 2000 Terminology of Hepatic Anatomy and Resections of the International Hepatobiliary Pancreatic Association provides a standard and has been adopted by most textbooks and journal articles.
The Brisbane 2000 Terminology is based on the anatomy of the hepatic artery and bile duct, which has a regular branching pattern, providing arterial blood to and draining the bile from eight functional zones or segments of the liver. As seen from an anterior view, the eight segments are numbered in a clockwise direction as described by Couinaud (Fig. 3).
Starting with the proper hepatic artery, the first division is the right and left hepatic arteries supplying the right and left hemilivers or livers, respectively, and there is very little overlap. The plane between the two distinct zones of blood supply extends from the gallbladder bed anteroinferiorly to the right side of the IVC posterosuperiorly and is called the mid-plane of the liver or Cantlie’s line. The middle hepatic vein lies exactly along this plane. On average, the right liver is about two-thirds of the total liver mass while the left liver comprises the other one-third. However, the ratio of the left liver volume to the total liver volume varies significantly and may range from <20% to nearly 50%.
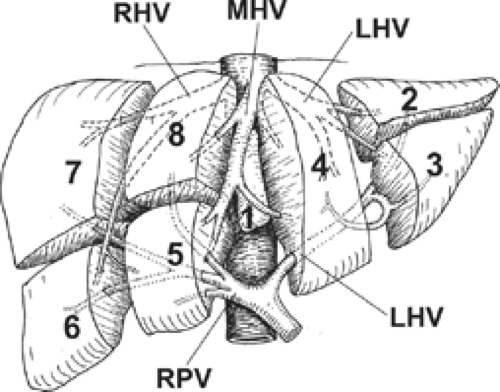 Fig. 3. Couinaud’s anatomic segments of liver (segments 1 to 8). MHV, middle hepatic vein; RHV, right hepatic vein; LHV, left hepatic vein; LPV, left portal vein; RPV, right portal vein. |
The right and left hepatic arteries then divide into four second-order sectional arteries each supplying a section of the liver. On the right side, the two sectional arteries supply the right anterior section and the right posterior section, and the plane between these sections is the right intersectional plane. There is no marking on the liver surface for this plane but the right hepatic vein serves as its internal landmark. On the left, the two sectional arteries supply the left medial section and left lateral section. The plane between these sections is the left intersectional plane and is marked by the round ligament at the umbilical fissure and the line of attachment of the falciform ligament to the anterior surface of the liver.
The four sectional arteries divide further to supply seven segments of the liver. The left lateral section consists of segments 2 and 3. The left medial section is a standalone segment 4. The right anterior section is divided into segments 5 and 8 and the right posterior section into segments 6 and 7.
The portal vein branching pattern in the right liver follows the same pattern as that of the hepatic artery and bile duct. The right portal vein divides into a right anterior section branch and a right posterior section branch, which further divide into four segmental branches. The left portal vein, however, has a different branching pattern from that of the left hepatic artery and bile duct. The left portal vein is much longer than the right portal vein and has a transverse portion of 2 to 3 cm located under segment 4 within the hilar plate that sends off only a few branches to segment 4. At the site of attachment of the ligamentum venosum, the left portal vein curves anteriorly and to the left to continue as the umbilical portion in the umbilical fissure (Fig. 1). Large branches come off both sides of the umbilical portion of the left portal vein, with multiple branches going from the right side to segment 4 and usually one large one going from the left side to segment 2 and one large one to segment 3. It then terminates as a blind end joining the round ligament anteriorly. Hence, unlike the right portal vein, the left portal vein has a very long extrahepatic course and never enters the liver substance.
Segment 1or the caudate lobe is a distinct part of the liver functionally independent of the right and left hemilivers. It is bounded posteriorly by the retrohepatic IVC, and superiorly by the left and middle hepatic veins at their origin. Its anterior border is formed by the left portal vein, the liver hilum, and the base of segment 4. The ligamentum venosum also courses along the anterior aspect of the caudate lobe from the left portal vein to the left hepatic vein. The caudate lobe is composed of three parts (Fig. 4). The caudate lobe proper (segment 1-l), or Spigelian lobe, sits on the left of the IVC and is separated from the left lateral section by the lesser omentum. The paracaval portion of the caudate lobe lies anterior to the IVC. The caudate process (segment 1-r) fuses indistinctly with segments 6 and 7 of the right liver. Since the venous drainage, arterial and portal venous blood supply, and the biliary drainage of the caudate lobe are completely different from those of the right and left livers, the anatomy of the caudate lobe will be described in a separate section at the end of this chapter.
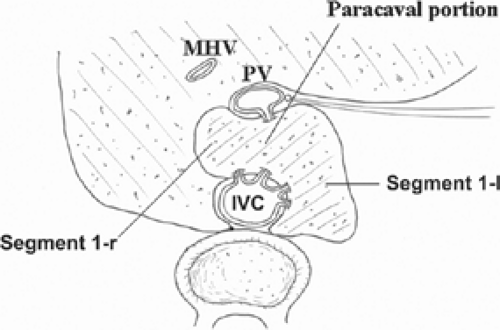 Fig. 4. Anatomy of caudate lobe. Segment 1-l, caudate lobe proper; Segment 1-r, caudate process; MHV, middle hepatic vein; PV, portal vein; IVC, inferior vena cava. |
In the Operating Room
Liver resection can be classified as “anatomical” and “nonanatomical.” Anatomical resection refers to removal of functional segments of the liver parenchyma with defined boundaries based on blood supply and biliary drainage. Resections that do not take into account the segmental anatomy of the liver are nonanatomical. Anatomical resections are generally more desirable as the parenchymal transection plane follows the relatively avascular watershed plane between segments and the vascular supply and biliary drainage of the liver remnant are less likely to be compromised. There may be a wider surgical margin with improved oncologic outcome.
The Brisbane 2000 Terminology of Hepatic Resection is based on the segmental anatomy of the liver. Resection of one side, a section or a segment of the liver is referred to as hepatectomy or hemihepatectomy, sectionectomy or segmentectomy, respectively. Hence, there are right and left hepatectomies or hemihepatectomies, and the sectionectomies are left lateral sectionectomy, left medial sectionectomy, right anterior sectionectomy, and right posterior sectionectomy. Resection of three contiguous sections is called trisectionectomy. A right trisectionectomy involves resection of the right liver together with the left medial section, and a left trisectionectomy involves resection of the left liver together with the right anterior section. The term “extended hemihepatectomy” has been used as a synonym for trisectionectomy but may be used for a hemihepatectomy that extends across the mid-plane. Hence, an extended right hemihepatectomy includes the middle hepatic vein with part of segment 4, and an extended left hemihepatectomy includes the middle hepatic vein with part of segments 5 and 8. A hemihepatectomy or trisectionectomy can be combined with resection of segment 1. While resection of a single segment is referred to as a numbered segmentectomy, more extensive resections can also be named in a similar way. A right hemihepatectomy, for example, is equivalent to resection of segments 5, 6, 7, and 8.
The total liver volume has a relatively constant relationship to the body weight. It is directly proportional to the body surface area and the ideal or standard liver volume of an individual can be estimated using published formulae such as the Urata formula. The ratio of the right or left liver to total liver volume, however, varies considerably between individuals. Hence, in major liver resections or in segmental liver transplantation such as split liver or living donor liver transplantation, preoperative estimation of segmental liver volume using computed tomography or magnetic resonance imaging volumetry is essential. When a right hepatectomy or trisectionectomy is necessary for tumor clearance in a non-cirrhotic liver and the left liver remnant is too small (<25%) on preoperative imaging, a preoperative right portal vein embolization may induce hypertrophy of the future remnant liver and improves the safety of the operation. In segmental liver transplantation, liver volumetry is important for the safety of both the donor and the recipient. In general, the type of liver graft should be chosen to ensure that ratio of the liver graft or remnant volume to the standard liver volume is >35% for the recipient and 30% for the donor. The difference in the recommended acceptable ratio in setting of living donor liver transplantation is attributed to the expected higher standard of safety in the living donor and the presence of ischemic-reperfusion injury, rejection, and presence of portal hypertension in the recipient.
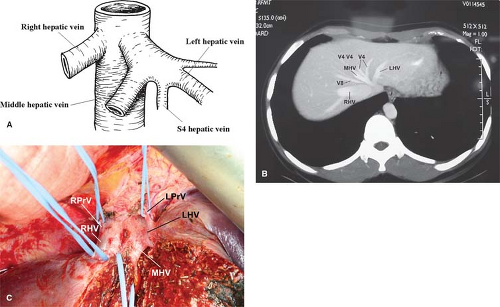
The anatomy of the hepatic veins of the liver is closely related to its segmental anatomy as the three major hepatic veins run in the intersectional planes between the four different sections and serve as important landmarks within the liver parenchyma for defining the boundaries between different segments. The venous blood from both the right and the left lobes of liver is collected by the branches of the three main hepatic veins (right, left, and middle), which drain into the suprahepatic part of the IVC below the diaphragm (Fig. 5). The middle hepatic vein joins the left hepatic vein to form a common trunk of about 1 cm long in 85% of cases before draining into the suprahepatic IVC. Occasionally, the two veins drain separately into the IVC. The right hepatic vein joins the right side of the IVC at a level slightly below that of the common trunk of the middle and left hepatic veins. There are multiple phrenic veins from both sides of the diaphragm, which drain into the lateral edge of the IVC close to or via the right and left hepatic veins. The suprahepatic IVC with the roots of the three main hepatic veins and its junctions with the phrenic veins are enclosed in a thick fibrous sheath, which is a direct extension of the diaphragm. On the posterior aspect of the retrohepatic IVC at the level of the junction with the right hepatic vein, a fibrous band called the IVC ligament (Makuuchi ligament) courses between the dorsal edge of the left side of the caudate lobe and the right liver. This ligament sometimes contains a bridge of thick liver tissue in which case the retrohepatic IVC will appear to pass through a tunnel in the liver.
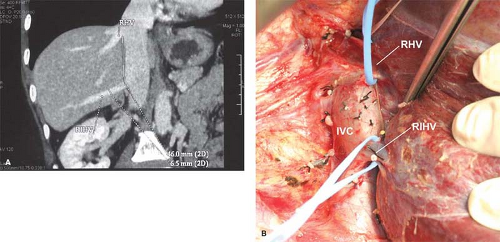
The right hepatic vein courses in the right intersectional plane between the right anterior and posterior sections. It is the longest vein in the liver and is single in >90% of cases. The main trunk of the right hepatic vein is formed by the convergence of an anterior trunk, which mainly drains segments 5 and 6, and a posterior trunk that chiefly drains segment 7. Over 60% of individuals have one or more right inferior hepatic veins present, which separately drain segment 6 or 7, or even the whole right posterior section directly into the IVC (Fig. 6). Under such circumstances, the right hepatic vein itself may be rather small.
The middle hepatic vein lies in the mid-plane between the right and left livers and provides venous drainage for both the right anterior section (segments 5 and 8) and the left medial section (segment 4). The main stem of the middle hepatic vein originates in three different ways: from the confluence of two equally sized branches from segments 5 and 4, as a main stem receiving multiple small branches from the same segments, and as a main stem from segments 5 and 6. The main stem invariably receives multiple branches from segments 8 and 4 as well. About 60% of the venous branches that drain segment 8 terminate in the middle hepatic vein. The middle hepatic vein provides venous drainage for <30%, or as high as 50%, of the right liver.
The left hepatic vein arises from a transverse branch, which drains segment 2, and a sagittal branch draining segment 3. In about 10% of cases, the segment-3 vein drains directly into the IVC; occasionally, it drains into the middle hepatic vein. The left hepatic vein runs in the plane between segments 2 and 3 and enters the left intersectional plane about 1 cm from its termination in the IVC where it may receive a venous branch from segment 4. This segment-4 hepatic vein is frequently named “umbilical vein” (simply because of its close location to the umbilical fissure), which is a misnomer easily confused with the umbilical vein in the fetus (remnant in the round ligament) or the umbilical portion of the portal vein and should be avoided. Venous branches from segment 4 may also drain predominantly into the middle hepatic vein or there may be a mixed pattern.
In the Operating Room
Unlike portal vein branches, which are covered by an extension of the Glissonian sheath, hepatic veins have a thin wall with no capsular covering and are hence a common source of major bleeding during liver surgery. Bleeding from hepatic veins is largely related to the central venous pressure and cannot be effectively controlled by inflow occlusion. Many surgeons regard hepatic veins as a source of trouble and try to deviate away from it during liver transection. Without any anatomical landmark, these surgeons can frequently get lost within the core of the liver parenchyma with the possibility of encountering multiple vascular and biliary branches. In practice, hepatic veins serve as landmarks for intersectional planes within the liver parenchyma to guide true anatomical resections. By identifying and following the course of the main stem of the middle hepatic vein in right hepatectomy (Fig. 7), for example, the surgeon would have a guide to a precise and relatively avascular transection plane for bisecting the liver. By taking the segment-5 and segment-8 hepatic vein branches at their junction with the main stem of the middle hepatic vein, the number of venous branches encountered and the amount of bleeding can be minimized. It is important to note that the right liver is, in fact, anatomically right posterior and the left liver left anterior, and the mid-plane is slanting in a right anterior to left posterior direction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree