Red and white pulp. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•Comprises 85% of the spleen
•Cell types: Mononuclear phagocytes
•Functions
•Clears nucleated remnants from immature RBCs
•Clears dead or damaged RBCs
•Without spleen—have Howell-Jolly bodies (nuclear remnants)
White Pulp
•Comprises 15% of the spleen
•Cell types: Lymphoid, mostly B cells
•Functions
•Clears bacteria without preexisting antibodies
•Clears poorly opsonized bacteria
•Clears foreign particles
•Clears cellular debris
What are the two types of arterial supply of the spleen?
Magistral and distributed (most common).
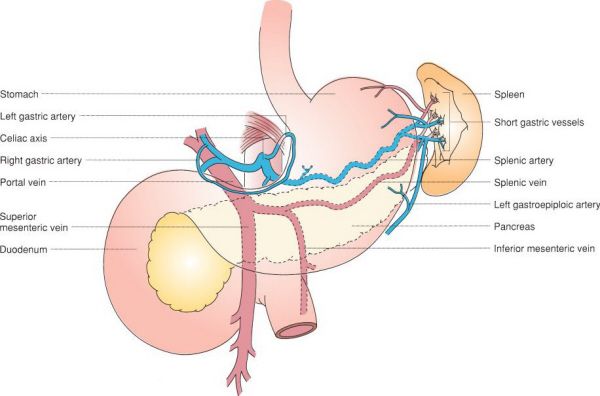
Arterial supply of the spleen. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Arterial Supply of the Spleen
•Magistral: A single arterial pedicle
•Distributed: Multiple branches enter the spleen arising from main trunks 2 to 3 cm from the hilum
A 32-year-old man who underwent a splenectomy does not have any Howell-Jolly bodies on a peripheral smear. What does this finding indicate?
The lack of Howell-Jolly bodies suggests that the patient may have unresected accessory splenic tissue or splenosis. Splenosis refers to the auto transplantation of splenic fragments.
Products Removed by the Spleen
•Howell-Jolly bodies (nuclear remnants)
•Pappenheimer bodies (iron granules)
•Heinz bodies (denatured hemoglobin)
•Target cells (deformed cells)
•Stippling (inclusions)
•Acanthocytes (spurred cells)
After splenectomy, a patient has persistent thrombocytopenia. What should you look for?
Perform imaging evaluation to see if the patient has an accessory spleen.
During a splenectomy, the tail of the pancreas was inadvertently resected with the specimen. What is the next step?
Place a surgical drain or multiple drains at the cut end of the pancreas (the pancreatic stump).
A 55-year-old male presents with a mass in the tail of the pancreas on CT scan that appears to be arising from the spleen. What is another test to evaluate the possibility an accessory spleen?
A sulfur colloid (“liver-spleen”) scan can help determine if the mass has the same consistency of the spleen.
What is the difference between splenomegaly and hypersplenism?
Splenomegaly is an enlarged spleen. Hypersplenism refers to any combination of neutropenia, anemia, or thrombocytopenia due to splenic sequestration.
A 48-year-old man with a history of cirrhosis presents with severe portal hypertension and a massive spleen. What is the best management of the splenomegaly?
Do NOT perform a splenectomy for portal-venous hypertension. Any operation in this setting carries an extremely high operative mortality. The best management is treatment of the underlying portal hypertension.
The most accepted contraindication to a splenectomy is portal hypertension.
A 59-year-old man with a history of IV drug abuse presents with a partial splenic infarction. What volume of normal splenic volume is required for full function?
Approximately 30% to 50% of the spleen’s mass can achieve most of the function of the entire spleen.
Splenic Infarction
•Rarely requires surgery
•Most resolve spontaneously
•Pain may persist for weeks
•There is no correlation between spleen infarctions and abscess formation
A 34-year-old man has a splenectomy performed for trauma. What is the most common trend in platelet count postoperatively?
The spleen normally stores approximately one-third of the body’s platelets, resulting in decreased sequestration and increased circulating platelets following a splenectomy.
Post-splenectomy Changes
•RBC increases
•WBC increases
•Platelet count increases
•Decreased antibody response to antigens (the opsonins, tuftsin, and properdin are produced in the spleen)
Against which organisms should one be vaccinated prior to splenectomy?
Encapsulated organisms: Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis.
When should the splenectomy patient be immunized?
At least 2 weeks prior to surgery is ideal so that fevers associated with the vaccine are not confused with postoperative sepsis. If the surgery is unplanned, vaccination should be delayed until the patient has regained immunocompetence. Vaccination is given prior to discharge for a poorly compliant patient.
A 48-year-old man presents with refractory bleeding varices and a long-standing history of pancreatitis. What intervention may be indicated?
Bleeding gastric varices in the setting of splenic vein thrombosis are effectively treated with splenectomy.
Splenic Vein Thrombosis
•Associated with pancreatitis because of the proximity of the vessel to the pancreas
•Can result in gastroesophageal varices
•Splenectomy is the definitive treatment for bleeding
•Prophylactic splenectomy is not indicated (less than 10% of splenic vein thromboses result in bleeding)
A 28-year-old woman presents with a new diagnosis of idiopathic thrombocytopenic purpura (ITP) by her hematologist. What is the next step in her management?
Steroids are the mainstay treatment for ITP. Surgery is reserved for refractory ITP.
Adult Immune or Idiopathic Thrombocytopenic Purpura
•Antiplatelet IgG directed at the fibrinogen receptor (IIb/IIIa) that triggers platelet destruction in the spleen
•More common in young women
•Medical treatment
•Successful in 15% of adults
•Steroids or IV gamma globulin
•Surgery
•Indicated for ITP refractory to the medical treatment above
•Successful in 85% of adults
•Transfuse platelets if necessary after the splenic artery is ligated
What is the size of a typical spleen in ITP?
Normal size; therefore, many patients are good candidates for laparoscopic splenectomy.
A 5-year-old girl presents with a new diagnosis of ITP following an upper respiratory infection. What is the likelihood that the disease will resolve without surgery?
Surgery is rarely indicated for childhood ITP. Approximately 70% of children with ITP will have complete resolution regardless of therapy.
Childhood Idiopathic Thrombocytopenic Purpura
•Occurs after viral illness
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


