24
Spirochetes
CHAPTER CONTENTS
INTRODUCTION
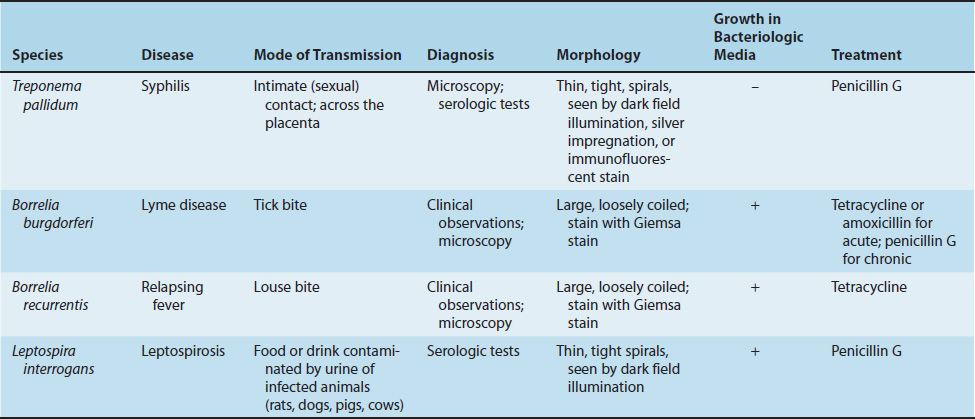
Three genera of spirochetes cause human infection: (1) Treponema, which causes syphilis and the nonvenereal treponematoses; (2) Borrelia, which causes Lyme disease and relapsing fever; and (3) Leptospira, which causes leptospirosis (Table 24–1).
Spirochetes are thin-walled, flexible, spiral rods (Figure 24–1). They are motile through the undulation of axial filaments that lie under the outer sheath. Treponemes and leptospirae are so thin that they are seen only by dark field microscopy, silver impregnation, or immunofluorescence. Borreliae are larger, accept Giemsa and other blood stains, and can be seen in the standard light microscope.

FIGURE 24–1 Treponema pallidum—dark field microscopy. The coiled form of this spirochete is in the center of the field. (Figure courtesy of Dr. Schwartz, Centers for Disease Control and Prevention.)
TREPONEMA
1. Treponema pallidum
Disease
Treponema pallidum causes syphilis.
Important Properties
T. pallidum has not been grown on bacteriologic media or in cell culture. Nonpathogenic treponemes, which are part of the normal flora of human mucous membranes, can be cultured.
T. pallidum grows very slowly. The medical importance of that fact is that antibiotics must be present at an effective level for several weeks to kill the organisms and cure the disease (see “Treatment” section later). For example, benzathine penicillin is the form of penicillin used to treat primary and secondary syphilis because the penicillin is released very slowly from this depot preparation, and bactericidal concentrations are present for weeks after administration of the antibiotic.
The antigens of T. pallidum induce specific antibodies, which can be detected by immunofluorescence or hemagglutination tests in the clinical laboratory. They also induce nonspecific antibodies (reagin),1 which can be detected by the flocculation of lipids (cardiolipin) extracted from normal mammalian tissues (e.g., beef heart).
Both specific antitreponemal antibody and nonspecific reagin are used in the serologic diagnosis of syphilis.
Transmission & Epidemiology
T. pallidum is transmitted from spirochete-containing lesions of skin or mucous membranes (e.g., genitalia, mouth, and rectum) of an infected person to other persons by intimate contact. It can also be transmitted from pregnant women to their fetuses. Rarely, blood for transfusions collected during early syphilis is also infectious. T. pallidum is a human organism only. There is no animal reservoir.
Syphilis occurs worldwide, and its incidence is increasing. It is one of the leading notifiable diseases in the United States. Many cases are believed to go unreported, which limits public health efforts. There has been a marked increase in incidence of the disease in homosexual men in recent years.
Pathogenesis & Clinical Findings
T. pallidum produces no important toxins or enzymes. The organism often infects the endothelium of small blood vessels, causing endarteritis. This occurs during all stages of syphilis but is particularly important in the pathogenesis of the brain and cardiovascular lesions seen in tertiary syphilis.
In primary syphilis, the spirochetes multiply at the site of inoculation, and a local, nontender ulcer (chancre) usually forms in 2 to 10 weeks (Figure 24–2). The ulcer heals spontaneously, but spirochetes spread widely via the bloodstream (bacteremia) to many organs.
FIGURE 24–2 Chancre of primary syphilis. Note the shallow ulcer with a rolled edge (red arrow) that is typical of a syphilitic chancre. (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
One to 3 months later, the lesions of secondary syphilis may occur. These often appear as a maculopapular rash, notably on the palms and soles (Figure 24–3), or as moist papules on skin and mucous membranes (mucous patches). Moist lesions on the genitals are called condylomata lata (Figure 24–4). These lesions are rich in spirochetes and are highly infectious, but they also heal spontaneously. Patchy alopecia also occurs. Constitutional symptoms of secondary syphilis include low-grade fever, malaise, anorexia, weight loss, headache, myalgias, and generalized lymph-adenopathy. Pharyngitis, meningitis, nephritis, and hepatitis may also occur. In some individuals, the symptoms of the primary and secondary stages may not occur, and yet the disease may progress.
FIGURE 24–3 Palmar lesions of secondary syphilis. Note the papulosquamous lesions on the right palm. Palmar lesions are typically bilateral. (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
FIGURE 24–4 Condylomata lata of secondary syphilis. Note the flat, moist perianal lesions (black arrow). (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
About one-third of these early (primary and secondary) syphilis cases will “cure” themselves, without treatment. Another third remain latent (i.e., no lesions appear, but positive serologic tests indicate continuing infection). The latent period can be divided into early and late stages. In the early latent period, which can last for 1 or 2 years after the secondary stage, the symptoms of secondary syphilis can reappear and patients can infect others. In the late latent period, which can last for many years, no symptoms occur and patients are not infectious. In the remaining one-third of people, the disease progresses to the tertiary stage. Tertiary syphilis may show granulomas (gummas), especially of skin and bones; central nervous system involvement, also known as neurosyphilis (e.g., tabes, paresis); or cardiovascular lesions (e.g., aortitis, aneurysm of the ascending aorta). In tertiary lesions, treponemes are rarely seen.
T. pallidum also causes congenital syphilis. The organism is transmitted across the placenta, typically after the third month of pregnancy, and fetal infection can occur. In the infected neonates, skin and bone lesions, such as Hutchinson’s teeth, mulberry molars, saber shins, saddle nose, rhagades, snuffles, and frontal bossing, are common. Other findings, such as hepatosplenomegaly, interstitial keratitis, and eighth nerve deafness, also occur. Fetal infection can also result in stillbirth.
Immunity to syphilis is incomplete. Antibodies to the organism are produced but do not stop the progression of the disease. Patients with early syphilis who have been treated can contract syphilis again. Patients with late syphilis are relatively resistant to reinfection.
Laboratory Diagnosis
There are three important approaches.
Microscopy
Spirochetes are demonstrated in the lesions of primary or secondary syphilis, such as chancres or condylomata lata, by dark field microscopy or by direct fluorescent antibody (DFA) test. They are not seen on a Gram-stained smear. In biopsy specimens, such as those obtained from the gummas seen in tertiary syphilis, histologic stains such as silver stain or fluorescent antibody can be used.
Nonspecific Serologic Tests
These tests involve the use of nontreponemal antigens. Extracts of normal mammalian tissues (e.g., cardiolipin from beef heart) react with antibodies in serum samples from patients with syphilis. These antibodies, which are a mixture of IgG and IgM, are called “reagin” antibodies (see above). Flocculation tests (e.g., Venereal Disease Research Laboratory [VDRL] and rapid plasma reagin [RPR] tests) detect the presence of these antibodies. These tests are positive in most cases of primary syphilis and are almost always positive in secondary syphilis. The titer of these nonspecific antibodies decreases with effective treatment, in contrast to the specific antibodies, which are positive for life (see later).
False-positive reactions occur in infections such as leprosy, hepatitis B, and infectious mononucleosis and in various autoimmune diseases. Therefore, positive results have to be confirmed by specific tests (see later). Results of nonspecific tests usually become negative after treatment and should be used to determine the response to treatment. These tests can also be falsely negative as a result of the prozone phenomenon. In the prozone phenomenon, the titer of antibody is too high (antibody excess), and no flocculation will occur. On dilution of the serum, however, the test result becomes positive (see Chapter 64). These tests are inexpensive and easy to perform and therefore are used as a method of screening the population for infection. The nonspecific tests and the specific tests (see later) are described in more detail in Chapter 9.
The laboratory diagnosis of congenital syphilis is based on the finding that the infant has a higher titer of antibody in the VDRL test than has the mother. Furthermore, if a positive VDRL test result in the infant is a false-positive one because maternal antibody has crossed the placenta, the titer will decline with time. If the infant is truly infected, the titer will remain high. However, irrespective of the VDRL test results, any infant whose mother has syphilis should be treated.
Specific Serologic Tests
These tests involve the use of treponemal antigens and therefore are more specific than those described earlier. In these tests, T. pallidum reacts in immunofluorescence (FTA-ABS)2 or hemagglutination (TPHA, MHA-TP)3 assays with specific treponemal antibodies in the patient’s serum.
These antibodies arise within 2 to 3 weeks of infection; therefore, the test results are positive in most patients with primary syphilis. These tests remain positive for life after effective treatment and cannot be used to determine the response to treatment or reinfection. They are more expensive and more difficult to perform than the nonspecific tests and therefore are not used as screening procedures.
Treatment
Penicillin is effective in the treatment of all stages of syphilis. A single injection of benzathine penicillin G (2.4 million units) can eradicate T. pallidum and cure early (primary and secondary) syphilis. Note that benzathine penicillin is used because the penicillin is released very slowly from this depot preparation. T. pallidum grows very slowly, which requires that the penicillin be present in bactericidal concentration for weeks. If the patient is allergic to penicillin, doxycycline can be used but must be given for prolonged periods to effect a cure. In neurosyphilis, high doses of aqueous penicillin G are administered because benzathine penicillin penetrates poorly into the central nervous system. No resistance to penicillin has been observed. However, strains resistant to azithromycin have emerged.
Pregnant women with syphilis should be treated promptly with the type of penicillin used for the stage of their disease. Neonates with a positive serological test should also be treated. Although it is possible that the positive test is caused by maternal antibody rather than infection of the neonate, it is prudent to treat without waiting several months to determine whether the titer of antibody declines.
More than half of patients with secondary syphilis who are treated with penicillin experience fever, chills, myalgias, and other influenzalike symptoms a few hours after receiving the antibiotic. This response, called the Jarisch-Herxheimer reaction, is attributed to the lysis of the treponemes and the release of endotoxin-like substances. Patients should be alerted to this possibility, advised that it may last for up to 24 hours, and told that symptomatic relief can be obtained with aspirin. The Jarisch-Herxheimer reaction also occurs after treatment of other spirochetal diseases such as Lyme disease, leptospirosis, and relapsing fever. Tumor necrosis factor (TNF) is an important mediator of this reaction because passive immunization with antibody against TNF can prevent its symptoms.
Prevention
Prevention depends on early diagnosis and adequate treatment, use of condoms, administration of antibiotic after suspected exposure, and serologic follow-up of infected individuals and their contacts. The presence of any sexually transmitted disease makes testing for syphilis mandatory, because several different infections are often transmitted simultaneously. There is no vaccine against syphilis.
2. Nonvenereal Treponematoses
These are infections caused by spirochetes that are virtually indistinguishable from those caused by T. pallidum. They are endemic in populations and are transmitted by direct contact. All these infections result in positive (nontreponemal and treponemal) results on serologic tests for syphilis. None of these spirochetes have been grown on bacteriologic media. The diseases include bejel in Africa, yaws (caused by T. pallidum subspecies pertenue) in many humid tropical countries, and pinta (caused by Treponema carateum) in Central and South America. All can be cured by penicillin.
BORRELIA
Borrelia species are irregular, loosely coiled spirochetes that stain readily with Giemsa and other stains. They can be cultured in bacteriologic media containing serum or tissue extracts. They are transmitted by arthropods. They cause two major diseases, Lyme disease and relapsing fever.
1. Borrelia burgdorferi
Disease
Borrelia burgdorferi causes Lyme disease (named after a town in Connecticut). Lyme disease is also known as Lyme borreliosis. Lyme disease is the most common tick-borne disease in the United States. It is also the most common vector-borne disease in the United States. Approximately 20,000 cases each year are reported to the Centers for Disease Control and Prevention, and that number is thought to be significantly less than the actual number.
Important Properties
B. burgdorferi is a flexible, motile spirochete that can be visualized by dark field microscopy and by Giemsa and silver stains. It can be grown in certain bacteriologic media, but routine cultures obtained from patients (e.g., blood, spinal fluid) are typically negative. In contrast, culture of the organism from the tick vector is usually positive.
Transmission & Epidemiology
B. burgdorferi is transmitted by tick bite (Figures 24–5 through 24–7). The tick Ixodes scapularis is the vector on the East Coast and in the Midwest; Ixodes pacificus is involved on the West Coast. The organism is found in a much higher percentage of I. scapularis (35%–50%) than I. pacificus (approximately 2%) ticks. This explains the lower incidence of disease on the West Coast. The main reservoir of the organism consists of small mammals, especially the white-footed mouse, upon which the nymphs feed.4
FIGURE 24–5 Ixodes tick. Nymph form of tick with head buried in skin surrounded by an erythematous macular rash. (Reproduced with permission from Wolff K, Johnson R. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree