Chapter 20 After studying this chapter, the learner will be able to: • Distinguish between monopolar and bipolar electrosurgical units and applications. • List the basic elements of electrosurgical safety. • Identify three basic types of lasers. • Describe the tissue effects of the different types of laser light in vivo. • Identify potential safety hazards associated with high technology in patient care. Terms Associated with Electrosurgery Apparatus used to deliver electric current to the surgical site. Current is delivered to the surgical site and returned to the generator by forceps. One side of the forceps is active; the other side is inactive. The current passes only between the tips of the forceps. Current that divides tissue and controls some bleeding. Current that passes intense heat through the active electrode used to sear vessels and control bleeding. Flow of electrical energy. Current that arcs between tissue and the active electrode to divide tissue without coagulation. Generator, foot pedal, cords, active electrode, and inactive dispersive return electrode designed to safely deliver electric current through tissue. Machine that produces electric current by generating high-frequency radio waves. Conducting connection among the generator, the patient, and the earth. Inactive dispersive return electrode Apparatus used to return current from the patient back to the generator; also referred to as inactive electrode, return electrode, or patient plate. Current flows from the generator to the active electrode, through the patient to the inactive dispersive return electrode, and returns to the generator. Terms Associated with Laser Surgery Surgical lasers emit nonionizing radiation, heat, and debris. Acronym for light amplification by stimulated emission of radiation. Light, concentrated and focused, stimulates atoms to emit radiant energy when activated. Light beams, either pulsed or continuous, go through a medium to produce a lasing effect. The beam has three distinct characteristics: Light beams are sustained over space and time because electromagnetic waves are in the same frequency and energy phase with each other. Light beams are parallel. A light beam is one color because waves are all the same length in the electromagnetic spectrum. Carbonized cell fragments, toxic hydrocarbons, viruses, and noxious fumes can be dispersed from tissues exposed to the laser beam. Vaporization converts solid tissue to smoke and gas. This plume (smoke) is evacuated to maintain visibility and also to minimize the hazard of inhalation by personnel. Gases, synthetic crystals, glass rods, liquid dyes, free electrons, and semiconductors are used to produce the lasing effect. All lasers have a combination of duration, intensity, and output of radiation when wavelengths are activated. Power to energize the light beam may be electrical, radiofrequency, or optical. Electromagnetic waves transfer energy progressively from point to point through a medium. The wavelength is the distance traveled along the electromagnetic spectrum. Radiation penetration differs at different wavelengths. Each laser has a different wavelength and color, depending on the medium the light beam passes through. Terms Associated with Microsurgery Attachment to the microscope that splits light; one part is reflected laterally, and the other part is relayed upward to the binocular tube; the percentage can be 50/50 or 30/70. The greater portion may be directed to a camera or video system. Using two eyes to see in stereoscopic vision. The light path follows the same direction as the visual image. Series of weights used to balance some microscopes. Distance of focus. Power of the lens to assist vision by refractive correction of reflected light. Distance between the lens and the object in focus. Equipment that uses a series of lenses to magnify very small objects. Using one eye for vision. Depth of field is absent; the image is two-dimensional. Power of the lens that determines the focal distance of vision. Eyepiece lens that multiplies the basic magnification of the microscope. Measurement between the pupils of the eyes; used to position the binocular eyepieces. Vision with two eyes that enables objects to appear three-dimensional. Physical space between the objective lens of the microscope and the surgical field. To change the range of focus in continuous magnification; the change can be closer or more distant. Advances in technology have made possible the complex surgical techniques of the present. Technology may be defined as the branch of knowledge that deals with the creation and use of technical means for scientific purposes. In the context of surgery, technology refers to a system that uses devices as well as people to perform specific tasks. Continuing research will further enhance technology. New devices are usually adjuncts to or extensions of devices or techniques already in use. To enhance their use in patient care, perioperative team members constantly need to learn about new equipment and its applications. Safety points to consider when using equipment in the OR: • Has the equipment been serviced on a routine schedule? • Has the equipment had calibration testing? • Has the equipment been cleaned or processed to the degree of safety for patient use? • Are the cords and attachments connected properly? • Are foot pedals in a secure position for safe use? • Are reusable components in serviceable condition? • Are disposable components in stock in the appropriate sizes? • Are adjunct devices and machines in proper working order? • Are alarms in working order? • Are power sources available? • Is the team knowledgeable about the correct sequence for powering up and using the equipment? • Have policies and procedures for equipment use been developed and provided to the OR team? Electrosurgery differs from electrocautery. Electrocautery is the use of a unidirectional current generated by a self-contained battery-operated disposable instrument with a wire at the tip. The wire heats when activated and coagulates the tissue. The energy does not enter the patient’s body. The ESU uses an alternating current that passes through the patient’s tissues and returns to the generator. Two forms of ESU generators are commonly used in surgery: monopolar and bipolar. Each type has specific uses and considerations.10 With monopolar units the electric current flows from the generator to the active electrode, through the patient to a return electrode, and returns back to the generator (Fig. 20-1). The generator returns the current to ground. Any break in the current flow from the generator and back again causes the machine to shut down and sound an alarm as a safety feature. 1. Coagulating current. Intense heat is produced to seal small to moderate vessels on contact. The current is continuous, but diminishes for short gaps of time. 2. Cutting current. The current is a constant flow of high energy output without gaps of time. The continuous flow of current causes the tissues to separate before high levels of heat build up. 3. Blended current. Both coagulating and cutting currents are produced at the same time in modified cycles. Small vessels are sealed as the tissue divides. Settings can be selected that have varied degrees of coagulation and cutting. One form of a patient return electrode adhesive pad is placed in direct contact with skin (Fig. 20-2). The contact area must exceed 100 mm2 and have a diameter greater than 1.2 cm. The adhesive return electrodes are flexible to mold to the appropriate body surface. Electrosurgery causes more patient injuries than any other electrical device used in the OR. Most incidents are caused by personnel error.9 Regardless of which return electrode is used, the following safeguards must be followed: 1. The return electrode should be as close as possible to the site where the active electrode will be used to minimize current through the body. 2. The patient should be in the desired position before the adhesive return electrode is applied to prevent its becoming dislodged or buckled during patient positioning. Do not remove or reposition the disposable return electrode because the integrity of the adhesive will be altered. A new electrode is used each time. 3. The return electrode should never be cut to fit. 4. The return electrode should cover as large an area of the patient’s skin as possible in an area free of hair or scar tissue, both of which tend to act as insulation. An area may need to be shaved. The surface area affects heat buildup and dissipation. Avoid areas where bony prominences might result in pressure points, which in turn can cause current concentration. Place the pad on a clean, dry skin surface over or under as large a muscle mass area as possible. The gel conduction material on the pad is cold and sticky to the touch; a patient who is awake should be forewarned of its application. 5. Any area that overlies an implant is a former surgical site and is not suitable for placement of a return electrode. The return electrode should not be placed on skin over a metal implant, such as a hip prosthesis, because current could be diverted to the implant and generate excessive heat. 6. The integrity of the package of a disposable return electrode should be inspected before use. Do not use the electrode if the package is damaged or has been previously opened. 7. Special care should be taken to ensure that the cord does not become dislodged. Do not put a safety belt over the electrode or cord. The connector should not create a pressure point on the patient’s skin. 8. The connection between the return electrode and generator should be secure and made with compatible attachments. If the return circuit is faulty, the ground circuit may be completed through inadvertent contact with the metal operating bed or its attachments. This is referred to as an alternative pathway for the current. With bipolar electrosurgery the current is directed from the generator to a special forceps with one active tip and one inactive tip. The current flows from the generator to the active tip and returns to the generator through the inactive tip (Fig. 20-3). The energy does not flow through the patient’s body as in monopolar electrosurgery. No return electrode is used. Output voltage is relatively low. This provides extremely precise control of the coagulated area. Bipolar electrosurgery is safe to use in cases in which electrical current passing through the body could cause disruption in implantable devices such as pacemakers or internal defibrillators. Because the current does not pass beyond the tines of the forceps the function of peripheral devices remains uninterrupted.9 Coblators use high-frequency bipolar energy in a conductive medium to create a highly focused plasma field.10 The energy is passed through a flow of saline irrigation to cause a field of highly charged electrons to break the molecular bonds of the target tissue while preserving the integrity of surrounding healthy tissue. The saline is conductive, causing a vaporized plasma field the thickness of a sheet of paper. The temperature does not need to reach extremes of thermal effect as in other coagulation devices to separate the tissues. The average temperature is only 20° C to 40° C compared with 200° C to 400° C. The tip of the wand instrument is 1 to 2.5 mm wide with two tiny electrodes through which the saline is passed over the target area.3 Coblation was originally designed for use in arthroscopy, but later found favor with otorhinolaryngologists for nasal and tonsil procedures.8 In oral and nasal tissue procedures the greatest limitation is in sinus procedures, where a bony obstruction may be encountered.13 Plastic surgeons have been working with coblation as a tool for skin resurfacing for deep acne scars and facial wrinkles. Coblation offers an alternative to chemical peels and laser surface modifications.5 1. Electrosurgery should not be used in the mouth, trachea, around the head, or in the pleural cavity when high concentrations of oxygen or nitrous oxide are used.1 During some procedures such as eye surgery, oxygen is administered via nasal cannula or mask. Oxygen builds up under the drapes and sets the stage for a combustible situation. Flame-retardant drapes can conceal a fire in a confined space. Safety regulations for use with all inhalation anesthetic agents are followed. 2. Electrocardiogram electrodes should be placed as far away from the surgical site as possible. Burns can occur at the site of electrocardiogram electrodes and other low-impedance points from invasive monitor probes if current diverts to alternate paths of least resistance. 3. Rings and other jewelry should be removed. Metallic jewelry, including that used in body piercing, presents a potential risk of burn for the patient from diverted currents from the monopolar unit with either an isolated or ground-referenced output. 4. Flammable agents such as alcohol should be used with great care in skin preparation. If they are used, the skin surface should be completely dry before draping. Volatile fumes and vapors may collect in drapes and ignite when the electrosurgical or cautery unit is used.9 5. If another piece of electrical equipment is used in direct contact with the patient at the same time as the ESU, connect it to a different source of current if possible. The cutting current of the ESU may not work if another piece of electrical equipment is on the same circuit. The ESU may interfere with the operation of some equipment, such as older models of cardiac monitors. The isolated power system of solid-state generators may prevent these problems. 6. New models of cardiac pacemakers are unaffected by monopolar ESU generators. Check with the pacemaker manufacturer regarding compatibility. The bipolar ESU may be used, because the current does not pass through the patient’s body and return to the generator. The patient is continuously monitored. A defibrillator should be on standby in the OR. 7. Connection of a bipolar active electrode to a monopolar receptacle may activate current, causing a short circuit. Plugs on cords should be differentiated to prevent misconnections of active and inactive electrodes. 8. Secure the active electrode handle in an insulated holster/container when not in use. Do not immerse an active electrode in liquid. 9. To prevent fire, only moist sponges should be permitted on the sterile field while the ESU is in use. This includes using moist sponges during the use of battery-operated electrocautery. Dry sponges can ignite. 10. Investigate a repeated request by the surgeon for more current. The dispersive return electrode or connecting cord may be at fault and should be checked first, followed by the handpiece connection. Shock to those touching the patient may result. The patient may be burned at the dispersive return electrode site. 11. For safety of the patient and personnel, follow instructions for use and care; these appear on the machine or in the manual provided by the manufacturer that accompanies each ESU. Grasp and pull only the plugs, not cords, when disconnecting attachments from the generator or the power source. Position the power cord away from the team to avoid tripping team members. Avoid rolling equipment over the power cord. Disposable cords should not be cut with scissors. 12. Any malfunctioning ESU should be labeled with the problem and taken out of service until cleared for use by biomedical engineering department personnel. 13. The patient and personnel should be protected from inhaling plume (smoke) generated during electrosurgery. A suction evacuator device should be placed as close to the source of plume as possible to maximize evacuation of smoke and enhance visibility at the surgical site. 14. Inspect insulated instruments for breaks in the insulation covering. Current can leak from fractures in the insulation and create a thermal burn. The term laser is an acronym for light amplification by stimulated emission of radiation. Lasers may emit their energy in brief, repeating emissions that have a duration of only an extremely small fraction of a second. These are pulsed laser systems. Or they are capable of producing continuous light beams; these are continuous-wave lasers. All lasers have a combination of duration, level, and output wavelengths of radiation emitted when activated. Power density, the irradiance, is the amount of power per unit surface area during a single pulse or exposure. This is expressed as watts per centimeter squared. Regardless of beam characteristics, components of a laser system are the same (Fig. 20-4). These components include the following: • An active medium to produce a lasing effect of the stimulated emission. Gases, solid rods or crystals, liquid dyes, and free electrons are used. Each produces a different wavelength, color, and effect. • An excitation power source to create population inversion by pumping energy into the active medium. This may be electrical or radiofrequency power or an optical power source such as a xenon flash lamp or another laser. • An amplification mechanism to change random directional movement of stimulated emissions to a parallel direction. This occurs within an optical resonator or laser cavity, which is a tube with mirrors at each end. As photons traveling the length of the resonator reflect back through the medium, they stimulate more atoms to release photons, thus amplifying the lasing effect. The power density of the beam determines the laser’s capacity to cut, coagulate, or vaporize tissue. • Wave guides to aim and control the direction of the laser beam. The optical resonator has a small opening in one end that permits transmission of a small beam of laser light. The smaller the beam, the higher its power density will be. Fiberoptic wave guides or a series of rhodium reflecting mirrors then direct the beam to tissue. The wave mode may be continuous, pulsed, or a Q-switched single pulse of high energy. • Backstops to stop the laser beam from penetrating beyond the expected impact site and affecting nontargeted tissue. Quartz or titanium rods will stop the beam. The wavelength of the laser light, power density, rate of delivery of energy, and exposure time will vary the effects on tissue. Energy density is based on the laser’s wattage, beam or spot size, and time of exposure. The spot size depends on the laser fiber size and distance of the tip from tissue; it increases and becomes defocused as fiber is moved farther from tissue. Variables in tissue reaction are listed in Box 20-1.
Specialized surgical equipment
Using specialized equipment in surgery
Electrosurgery
Principles of electrosurgery
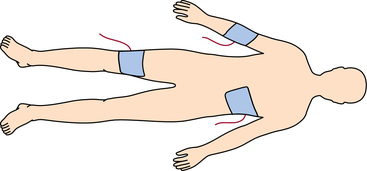
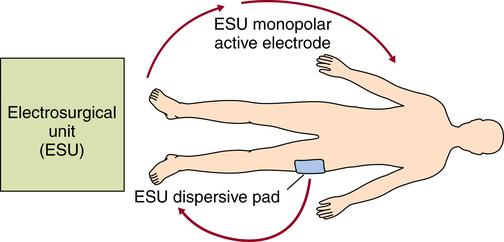
Monopolar electrosurgery
ESU generator
Patient return electrode (inactive dispersive electrode)
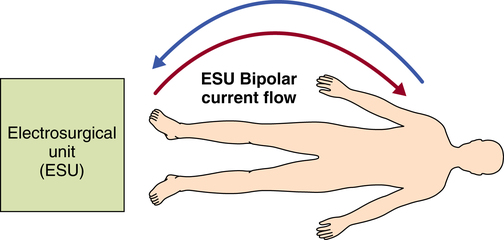
Bipolar electrosurgery
Coblation
Generalized safety factors for the use of electrosurgery
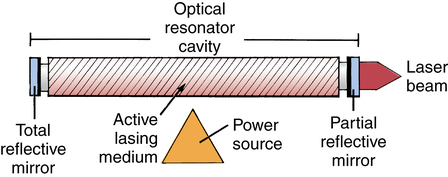
Laser surgery
Physical properties of lasers
Types of lasers
Specialized surgical equipment

 Website
Website