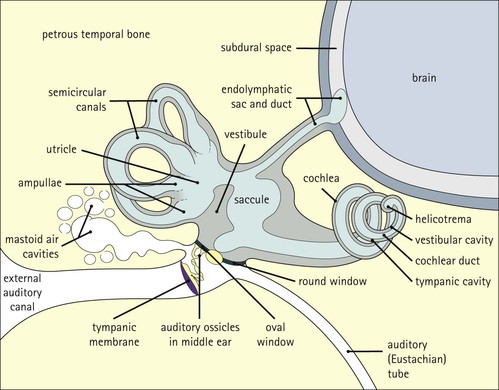
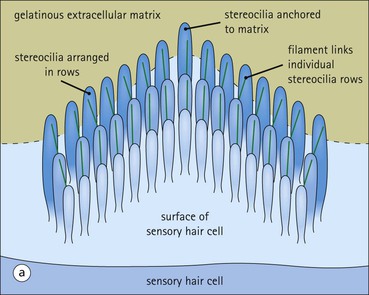
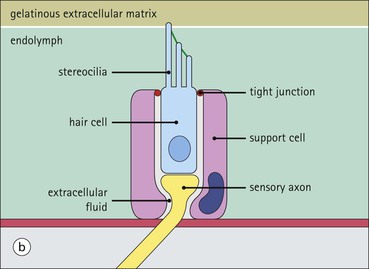
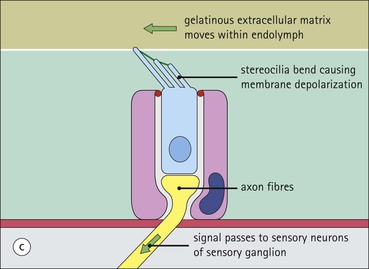
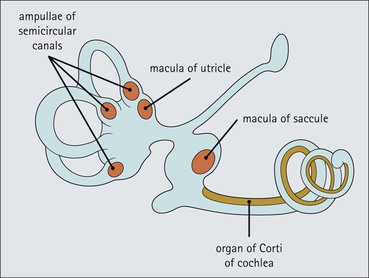
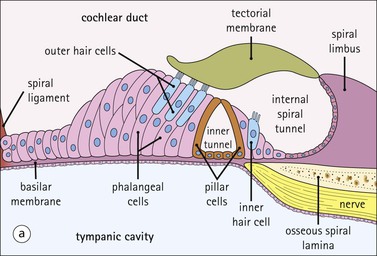
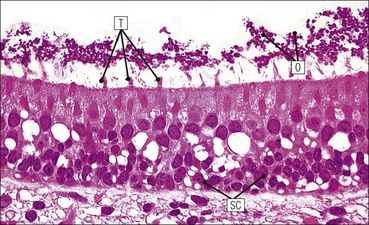
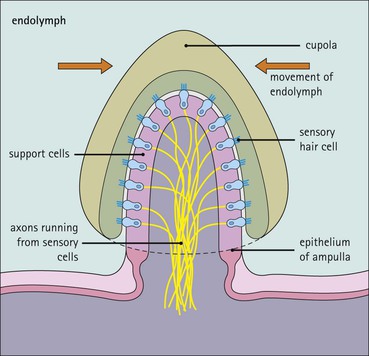
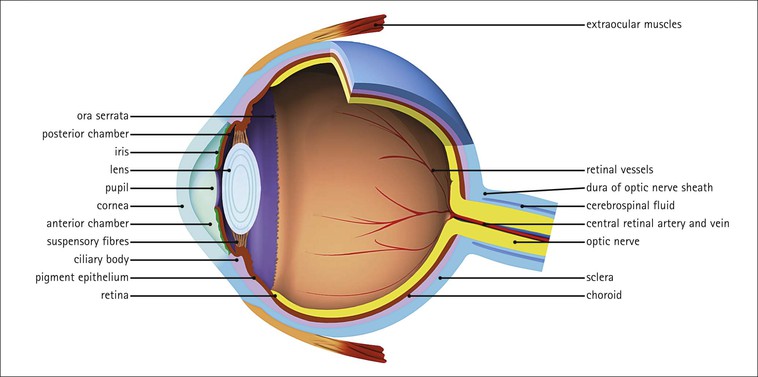
A vital function of the nervous system is the gathering of sensory information Sensory information is derived from a variety of specialized sensory nerve endings. These include: • Sensory endings in the skin to detect touch (fine touch, pressure), pain and temperature (see Chapter 18) • Tendon endings and muscle spindles to detect movement and position of the limbs • Chemoreceptive organs, such as the carotid body • Sensory endings on the tongue to detect taste In addition, information is obtained by the specialized sensory organs, the eye and the ear; the ear and the vestibular system detect sound, acceleration and position and the eye perceives light. The ear is divided into the external ear, middle ear and inner ear The external ear comprises the pinna and external auditory canal. The pinna is composed of elastic cartilage covered by hair-bearing skin. The external auditory canal is lined by hair-bearing skin. Within its subcutaneous tissues are wax-secreting ceruminous glands, which are modified sebaceous glands. The outer two-thirds of the canal is surrounded by elastic cartilage in continuity with the pinna; the inner third is surrounded by the temporal bone of the skull. The middle ear is separated from the external ear by the tympanic membrane The tympanic membrane marks the boundary between the external ear and the cavity of the middle ear, which is also termed the tympanic cavity (Fig. 19.1). The tympanic membrane is a three-layered structure: The middle ear transmits sound vibrations to the inner ear The middle ear cavity is lined by a low cuboidal epithelium and contains three auditory ossicles, the incus, malleus and stapes. These are: • Articulated by synovial joints (see Chapter 13) • Covered externally by the same low cuboidal epithelium that lines the inner ear. Two small skeletal muscles, the stapedius and the tensor tympani, are associated with the ossicles and damp motion between the bones, which occurs in response to loud noise. The middle ear cavity communicates directly with air-filled spaces in the mastoid bone (mastoid sinuses), which are lined by low cuboidal or flattened squamous epithelium. The auditory (Eustachian) tube equalizes pressure in the middle ear cavity The auditory tube extends from the middle ear cavity to the nasopharynx and is lined by ciliated epithelium similar to that of the respiratory tract. Its function is to equilibrate pressure between the middle ear cavity and the atmosphere. Normally, the auditory tube is collapsed, but it is opened by movement of muscles in the nasopharynx, such as occurs with swallowing or yawning. The inner ear is a series of fluid-filled sacs encased in bone The inner ear consists of fluid-filled sacs (membranous labyrinth) that lie in cavities in the temporal bone of the skull (bony or osseous labyrinth). The membranous labyrinth comprises the cochlear duct, the saccule, the utricle and semicircular canals and the endolymphatic sac and duct, the walls of which are composed of sheets of fibrocollagenous support tissue lined by a flat epithelium. These sacs are filled with a fluid called endolymph and have epithelial and sensory specializations to detect position and sound. The osseous labyrinth is composed of three cavities: the vestibule, the semicircular canals and the cochlea, which are lined by periosteum and filled with fluid called perilymph. Movement is detected in the inner ear by mechanoreceptors Mechanoreceptors or hair cells are specialized epithelial cells bearing a highly organized system of microvilli (stereocilia) on their apical surface. Deflection of the microvilli causes electrical depolarization of the hair cell membrane, which is transmitted to the central nervous system by the connecting axons of sensory nerve cells (Fig. 19.2). Patches of hair cells are located in three sites: • Within the vestibular apparatus in the ampullae of the semicircular canals to detect acceleration • Within the organ of Corti of the cochlea to detect sound vibration. At each site, the hair cell microvilli are embedded in a gelatinous matrix, which moves according to the stimulus it is detecting. Movement of the microvilli towards the tallest row excites (depolarizes) the hair cell membrane, whereas movement towards the shortest row inhibits (hyperpolarizes) it. Hair cells are arranged in different parts of the membranous labyrinth (Fig. 19.3) in order to sense movement generated by different causes. Support cells surround the hair cells and are anchored to them at their apex by occluding junctions. These junctions maintain ionic gradients between the endolymph and the extracellular fluid around the cells, the gradients being reversed on depolarization. Sound is detected in the inner ear by the organ of Corti in the cochlear duct The cochlear duct is a blind-ended tubular diverticulum filled with endolymph. It makes two and three-quarter turns within the spiral-shaped bony cochlea in the temporal bone, and is compressed between two other tubular spaces, the vestibular and tympanic cavities, which are filled with perilymph (Fig. 19.4). Within the cochlear duct is the organ of Corti, which is a special adaptation of the epithelial cells lining the cochlear duct and detects sound vibration (Fig. 19.5). Gravity and static position are detected by hair cells in the macula of the utricle and the macula of the saccule The macula of the utricle lies in the horizontal plane, whereas the macula of the saccule lies in the vertical plane at right-angles to the macula of the utricle (see Fig. 19.3). Each macula is histologically identical and is composed of the following three cell types (Fig. 19.6): In addition to an organ-pipe arrangement of tall microvilli stereocilia on their apical surface (see Fig. 19.2), these hair cells possess a single true cilium termed a kinocilium, which is located just behind the tallest row of stereocilia. The stereocilia and kinocilium of each new hair cell are embedded in a gelatinous plaque of extracellular matrix called the otolithic membrane, which is suspended in the endolymph. This membrane is covered by numerous small particles composed of protein and calcium carbonate, the otoconia (otoliths). The macula can detect the direction of gravity by sensing the direction of pull of the otolithic membrane and otoconia on the mass of hair cells that results from head movement either backwards and forwards (macula of utricle) or from side to side (macula of saccule). Acceleration and motion are detected by hair cells in the ampullae at the end of the semicircular canals There are three semicircular canals, which assume posterior, superior and horizontal positions. Each ampulla is a 1 mm long dilated region of the membranous labyrinth and contains a patch of hair cells arranged in a tall finger-like structure (an ampullary crista). The stereocilia of the sensory hair cells are attached to a dome-shaped gelatinous matrix termed a ‘cupola’ (Fig. 19.7). With rotary motion of the head, endolymph moves within the membranous labyrinth because of the static inertia of the fluid relative to the rest of the vestibular apparatus. Such movement causes displacement of the cupola, and the direction of this displacement is detected by the hair cells. When integrated, perception from the three semicircular canals arranged in planes perpendicular to each other provides information on the direction and rate of acceleration of head movement. The eye is designed to focus light on to specialized receptors that respond to light. It is composed of sclera, cornea, uvea and retina arranged around three chambers (Fig. 19.8). The sclera proper is the outer fibrocollagenous coat of the globe of the eye The sclera varies in thickness from 1 mm posteriorly to 0.5 mm anteriorly, and is composed of flat plates of collagen oriented in different directions, but parallel to the surface. The sclera is composed of three layers:
Special Senses
Introduction
Ear
Eye
Special Senses
Chapter 19
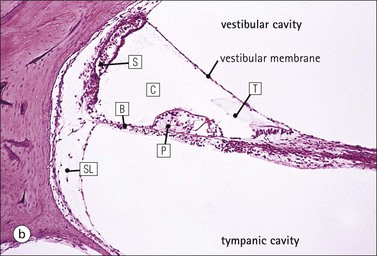
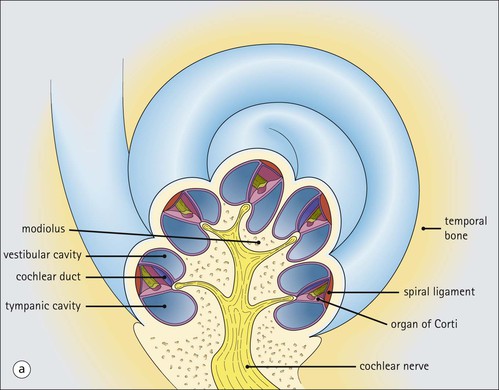
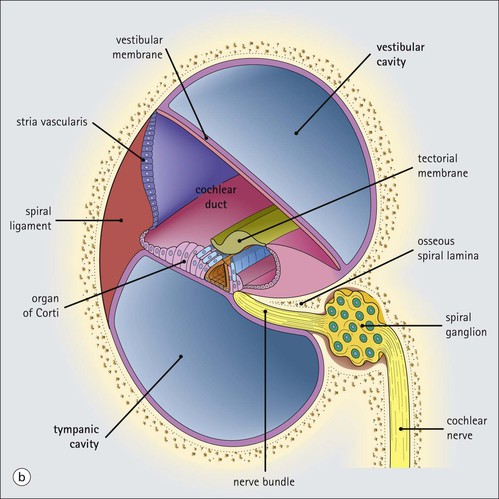
FIGURE 19.4 Cochlea. (a) The cochlea of the osseous labyrinth contains three spaces, the vestibular cavity, the cochlear duct and the tympanic cavity. These spaces are wound in a spiral within the temporal bone. The central spiral of bone within the cochlea is called the ‘modiolus’. The vestibular cavity and the tympanic cavity contain perilymph continuous with that in the vestibule (see Fig. 19.1), whereas the cochlear duct, which is continuous with and part of the membranous labyrinth, is filled with endolymph. At the apex of the cochlea, the vestibular and tympanic cavities connect at an opening termed the ‘helicotrema’. The cochlear nerve emerges from the base of the cochlea and carries signals to the brain. (b) Shown here is a section through the cochlea. The vestibular membrane (Reissner’s membrane) consists of two layers of flattened epithelium separated by a basement membrane, one cell layer being in continuity with the cells lining the vestibular cavity and the other in continuity with the cells lining the cochlear duct. The cells are held together by well-developed occluding junctions to maintain different electrolyte concentrations between the endolymph and the perilymph. The stria vascularis is a specialized area of epithelium with a rich vascular supply in the lateral wall of the cochlear duct. Many of the cells here have ultrastructural features indicating an ion transport function, and it is thought that they secrete endolymph. The basilar membrane is thicker than the vestibular membrane and consists of collagen fibres as well as a basement membrane. On one side it is covered by cells lining the tympanic cavity, and on the other by specialized cells lining the cochlear duct. Medially, the basilar membrane is continuous with the organ of Corti, which is a specialized area of support cells and sensory hair cells subserving hearing (see Fig. 19.5). The organ of Corti is supported by a spur of bone called the ‘osseous spiral lamina’. Laterally, the basilar membrane is attached to the spiral ligament, which is a mass of tissue developed from the endosteum of the surrounding bone. Neurons of the spiral ganglion are present adjacent to the osseous spiral lamina.