| Neurotoxin | Dilution (U/ml saline) | Maximum dose |
|---|---|---|
| OnabotulinumtoxinA | 25–100 | 400 U/limb; 600 U/session |
| AbobotulinumtoxinA | 200–500 | 1500 U/upper limb; 2000 U/lower limb; 2000 U/session |
| RimabotulinumtoxinB | Pre-diluted | 10 000 U/upper limb; 17 500 U/session |
| IncobotulinumtoxinAa | 25–100 | 400 U/limb; 495 U/session |
Maximum doses
Although there are no absolutes, the usual dose maximums found in literature for a single injection session are also presented in Table 14.1. Higher doses in a single session may increase the risk of both local and diffuse side effects and adverse reactions (Francisco, 2004). However, studies in large series of patients receiving onabotulinumtoxinA and incobotulinumtoxinA did not reveal systemic adverse effects (Dressler and Adib Saberi, 2006). In patients treated with BoNT serotype B, systemic autonomic adverse effects may occur at intermediate doses (Dressler and Benecke, 2003).
Individual muscle doses
The dose of BoNT for individual muscles depends mainly on their size and the degree of spastic contraction. Consideration must also be given to the total number of muscles to be injected and the maximum recommended dose per injection session of the particular BoNT preparation used. Based on these considerations, Table 14.2 gives the dose ranges usually employed for individual muscles in clinical practice. Spasticity trials using incobotulinumtoxinA have, to date, employed published dosing guidelines for the onabotulinumtoxinA preparation, and a 1:1 dosing ratio for these two preparations is used in general practice (Dressler et al., 2012).
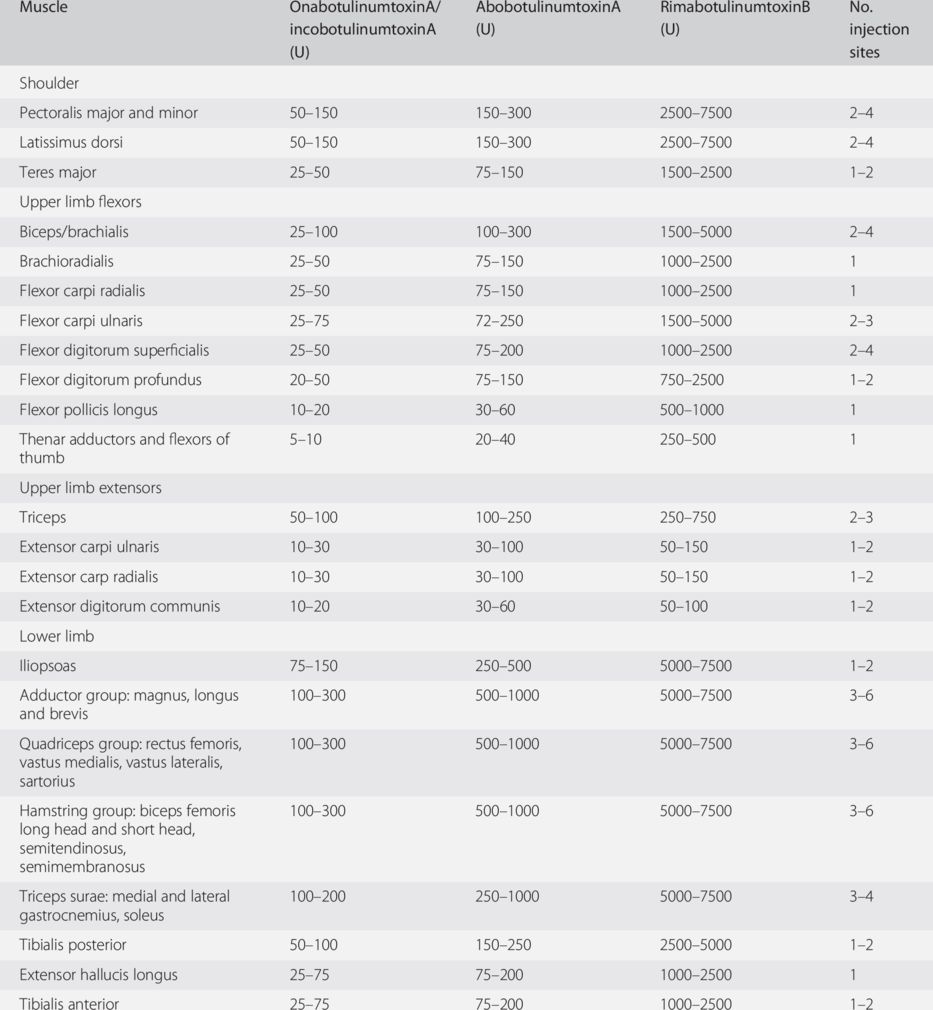
a The majority of the dosing recommendations in this table were formed as a consensus among members of the WE MOVE Spasticity Study Group (2005a,b) and may be accessed online. These consensus recommendations have been supplemented with additional muscles and doses based on Pathak et al. (2006), Kaňovský et al. (2009) and Barnes et al. (2010).
Guidance techniques
Palpation and anatomical landmarks may be used to place injections. However, the use of various guidance techniques increases precision and may improve safety, decrease side effects and possibly increase efficacy (O’Brien, 1997; Traba Lopez and Esteban, 2001; Childers, 2003; Monnier et al., 2003). Guidance is recommended for injecting cervical muscles and deep pelvic or small limb muscles; it is optional for larger easily palpated muscles. The principal guidance techniques are electromyography (EMG), electrical stimulation, ultrasound and fluoroscopy.
In EMG guidance, injections are made through a cannulized, Teflon-coated monopolar hypodermic needle attached to an EMG machine. If able, the patient is asked to voluntarily contract the target muscle. When the bare needle tip is within the target muscle belly, the crisp staccato of motor units firing close to the tip should be heard, and sharp motor units with short rise times are seen on the video monitor. If the needle tip is outside the muscle or in a tendinous portion, only a distant rumbling will be heard, and dull indistinct motor units seen. Tapping the tendon or passively moving the joint may elicit motor units in paralyzed patients.
In patients who are either paralyzed or unable to follow commands, low-amperage electrical stimulation directly through the bare tip of the insulated hypodermic needle may be used to produce visible contraction in the target muscle (O’Brien, 1997; Childers, 2003; Chin et al., 2005). The needle is repositioned until contractions may be reproduced by the lowest stimulation intensities.
Ultrasonography has been used to guide injections in the urinary system and salivary glands and is becoming more popular for skeletal muscles (Berweck et al., 2002; Westhoff et al., 2003). Fluoroscopy is utilized mainly for injection of deep pelvic girdle muscles in nerve entrapment and pain syndromes (Raj, 2004).
Injection placement
Smaller muscles generally require only one injection site anywhere within the muscle belly. Larger, longer or wider muscles are best injected at two to four sites. Although the BoNT works only at endplates, it is not necessary to identify the motor point or endplate region, since this region is generally broad and the BoNT diffuses. Identifying the motor point usually requires repeated repositioning of the needle under electrical stimulation or EMG guidance (Traba Lopez and Esteban, 2001), is painful and any advantage in efficacy appears minimal.
Spasticity patterns
The most common pattern of spasticity in the upper limb involves flexion of the fingers, wrist and elbow, adduction with internal rotation at the shoulder, and sometimes thumb curling across the palm or fist (Mayer et al., 2002) (Fig. 14.1). Wrist or elbow extension is less common. There may sometimes be a combination of metacarpophalangeal flexion and proximal interphalangeal extension.

Fig. 14.1 Common pattern of spasticity in upper and lower limbs.
The most common pattern of spasticity in the lower limb involves extension at the knee, plantarflexion at the ankle and sometimes inversion of the foot (Mayer et al., 2002) (Fig. 14.1). This pattern is seen unilaterally in stroke. It occurs bilaterally in cerebral palsy and some spinal cord lesions, producing a “toe-walking pattern.” Other patterns of spasticity in the lower limbs include “scissoring” adduction at the hip joints, flexion or extension at the knees and spastic extension of the great toe (Mayer et al., 2002).
It is important to distinguish plantarflexion posture caused by spastic contraction of the calf muscles from flaccid “drop foot” caused by paresis of the tibialis anterior and other dorsiflexor muscles. Drop foot classically occurs with peroneal nerve palsy or lumbar radiculopathy and occasionally after stroke. Use of BoNT is not indicated in flaccid drop foot, and ankle–foot orthotic splints are usually sufficient to bring the foot and ankle to neutral position.
Extensor posturing at the knee also requires careful consideration before injection because quadriceps strength is important in maintaining weight-bearing stance during walking, and some degree of residual spasticity may be helpful. Additionally, the large powerful muscles of the proximal lower limb require high doses of BoNT approaching recommended maximums, and most patients will benefit more from the application of this dose elsewhere.
Treatment guide
Note that in Figs. 14.2 to 14.16 (below) target muscles are printed in bold and lines with arrowheads represent approximate injection vectors.
Fig. 14.2 Injection of flexor digitorum superficialis.
Fig. 14.3 Injection of flexor digitorum profundus.
Fig. 14.4 Injection of adductor pollicis and other thenar muscles.
Fig. 14.5 Injection of flexor pollicis longus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


