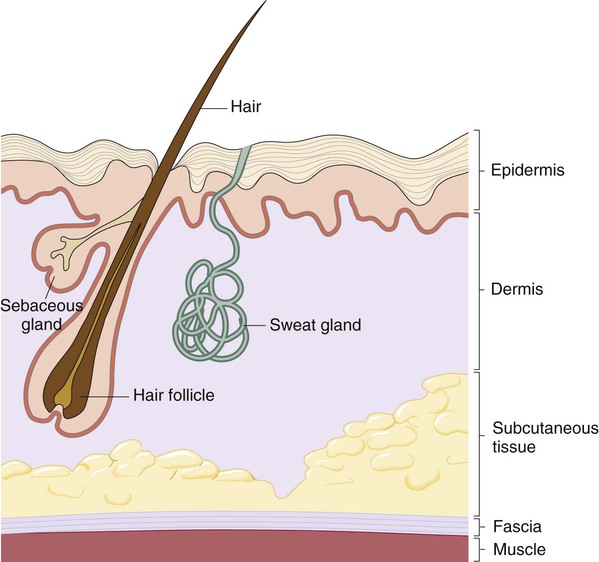
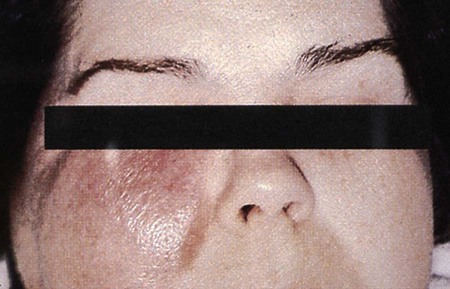
1. Identify the three layers of the skin and describe the function of the skin in host defense including the physical and chemical properties. 2. List the organisms that colonize the skin and are considered normal flora. 3. Describe the mechanisms for the transmission that allow bacteria to invade and cause skin and soft tissue infections. 4. Define each of the following manifestations of skin infection: 5. Characterize each of the following types of infection, and describe the associated laboratory diagnosis: 6. List an organism that commonly causes the following types of infection, and describe the associated laboratory diagnosis: 7. Define sinus tract, including organisms associated with this condition. 8. Identify the pathogens most frequently associated with infections in patients with diabetes mellitus. 9. Describe and evaluate a specimen submitted for culture from the following types of infection: ulcers, nodules or abscess, pyoderma or cellulitis, vesicles or bullae, sinus tracts, fistula, burns, postsurgical wounds, and bite infections. 10. Correlate patient signs and symptoms with laboratory results to identify the etiologic agent associated with the skin, soft tissue, or wound infection. The skin is divided into three distinct layers: the epidermis (the outermost layer), the dermis, and the subcutaneous tissue (Figure 76-1). The epidermis is made up of layered squamous epithelium. Hair follicles, sebaceous glands (oil-producing), and sweat glands open to the skin surface through the epidermis. The dermis is composed of dense connective tissue rich in blood and nerve endings, and this is where some hair follicles and sebaceous glands originate. The subcutaneous tissue contains loose connective tissue and is rich in fat. Deeper hair follicles and sweat gland originate in this layer. Below the subcutaneous layer are thin fascial membranes (sheets or bands of fibrous tissue) covering muscles, ligaments, and other connective tissues. The skin is the body’s largest and thinnest organ. It forms a self-repairing and protective boundary between the body’s internal environment and the external environment. Skin plays a crucial role in the control of body temperature, excretion of water and salts, synthesis of important chemicals and hormones, and as a sensory organ. The skin has an important protective function because of the composition of the outermost layer of the epidermis, which is composed of cells containing keratin, a water-repellent protein. The skin’s normal microbial flora, pH, and chemical defenses (high salt and acidic environment) also help prevent colonization by many pathogens. The resident microbial flora is listed in Box 76-1. Because of the diversity of etiologic agents, clinicians will often rely on the appearance of skin lesions for diagnostic clues in order to determine the required laboratory testing. The physical characteristics of the lesions can indicate the need for smear, culture, biopsy, or surgical procedures. Some of the terms most frequently used to describe manifestations of skin infections are provided in Table 76-1. Figure 76-2 shows examples of some skin lesions. TABLE 76-1 Manifestations of Skin Infections Adapted from Lazar AJF: Robbins Basic Pathology, ed 8, St. Louis, 2007, Saunders. Numerous infections of the skin may occur. Several of the most common are discussed here. Folliculitis, furuncles, and carbuncles are localized abscesses either in or around hair follicles. These infections are distinguished from one another based on size and the extent of involvement in subcutaneous tissues. Table 76-2 summarizes each infection’s respective clinical features. For the most part, these infections are precipitated by blockage of the hair follicle with skin oils (sebum) or because of minor trauma resulting from friction such as that caused by clothes rubbing the skin. Staphylococcus aureus is the most common etiologic agent for all three infections. Members of the Enterobacteriaceae family may also cause folliculitis. Outbreaks of folliculitis caused by Pseudomonas aeruginosa have been reported to be associated with the use of whirlpools, swimming pools, and hot tubs. TABLE 76-2 Infections Involving Hair Follicles Because of their ability to utilize the keratin in the epidermal cells, the dermatophyte fungi are significant and well-suited pathogens for infection. Unlike the previously discussed infections, dermatophytes do not invade the deeper layers of skin. Because keratin is also present in hair and nails, these fungi may also cause superficial infections at these sites (see Chapter 61 for more information). Most infections in the deeper layers of the epidermis and dermis result from the inoculation of microorganisms by traumatic breaks in the skin. These superficial skin infections usually do not require surgical intervention. Table 76-3 summarizes these infections. In most instances, these infections resolve with local care and only occasionally require antimicrobial therapy. TABLE 76-3 Infections of the Epidermal and Dermal Layers of the Skin In many instances, infections of the epidermis and dermis extend deeper and become subcutaneous infections and may even reach the fascia or muscle. For example, erysipelas (Figure 76-3) can develop into subcutaneous cellulitis and eventually necrotizing fasciitis. Similarly, folliculitis can readily develop into a subcutaneous abscess or carbuncle that can extend to the fascia. Cellulitis can also extend to the subcutaneous tissues (Figure 76-4). Anaerobic cellulitis is associated with the production of large amounts of gas by organisms that may be present in the subcutaneous tissue. This type of infection is most often located in the extremities and is particularly common among patients with diabetes. The infection may involve the neck, abdominal wall, perineum, connective tissue, or be present in other areas. Anaerobic cellulitis may also occur as a postoperative condition. The onset and spread of the lesion is usually slow and patients may not immediately show obvious systemic effects. The causative agents in deep tissue infections are almost always a mixture of aerobic/facultative and anaerobic organisms. Common aerobic/facultative organisms include Escherichia coli, alpha-hemolytic and nonhemolytic streptococci, and S. aureus, but group A streptococci and other members of the Enterobacteriaceae may be encountered as well. The anaerobes are typically found in greater numbers and in more variety, and include Peptostreptococcus spp., Bacillus fragilis group strains, Prevotella, Porphyromonas, other anaerobic gram-negative bacilli, and clostridia. Bacteremia is not usually present.
Skin, Soft Tissue, and Wound Infections
General Considerations
Anatomy of the Skin
Function of the Skin
Prevalence, Etiology, and Pathogenesis
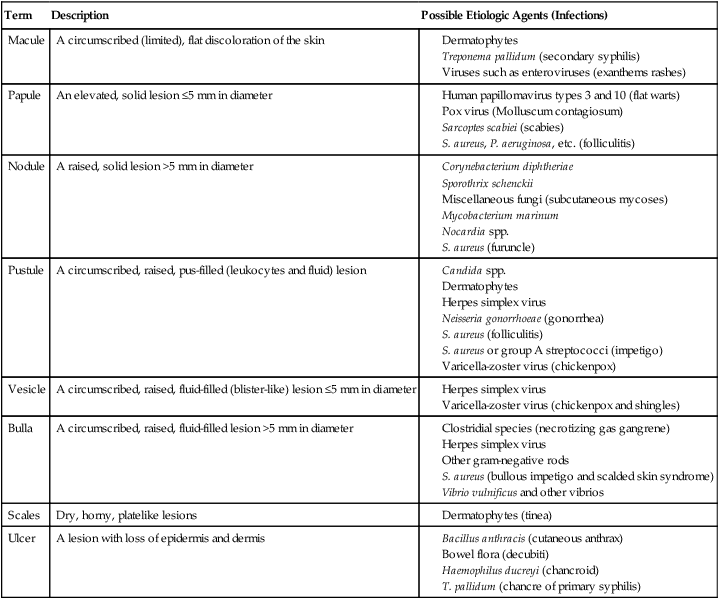
Term
Description
Possible Etiologic Agents (Infections)
Macule
A circumscribed (limited), flat discoloration of the skin
Papule
An elevated, solid lesion ≤5 mm in diameter
Nodule
A raised, solid lesion >5 mm in diameter
Pustule
A circumscribed, raised, pus-filled (leukocytes and fluid) lesion
Vesicle
A circumscribed, raised, fluid-filled (blister-like) lesion ≤5 mm in diameter
Bulla
A circumscribed, raised, fluid-filled lesion >5 mm in diameter
Scales
Dry, horny, platelike lesions
Ulcer
A lesion with loss of epidermis and dermis
Skin and Soft Tissue Infections
Infections of the Epidermis and Dermis
Infections in or around Hair Follicles
Infection
Skin Manifestations
Folliculitis—(minor infection of hair follicles)
Papules or pustules that are pierced by a hair and surrounded with redness
Furuncle (boil)
Abscess that begins as a red nodule in a hair follicle that ultimately becomes painful and full of pus
Carbuncle
Furuncles that coalesce and spread more deeply to the dermis and subcutaneous tissues; they usually have multiple sites, which drain to the skin surface (sinuses)
Infections in the Keratinized Layer of the Epidermis
Infections in the Deeper Layers of the Epidermis and Dermis
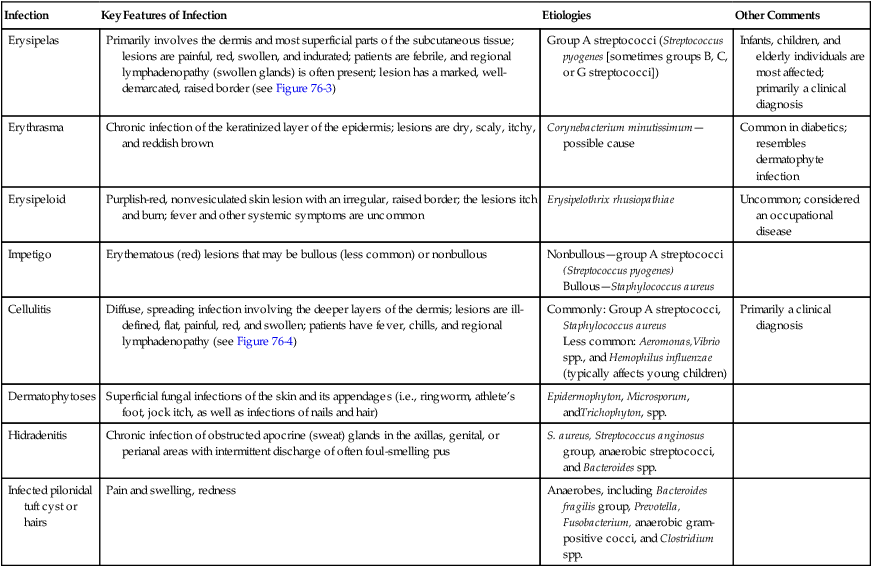
Infection
Key Features of Infection
Etiologies
Other Comments
Erysipelas
Primarily involves the dermis and most superficial parts of the subcutaneous tissue; lesions are painful, red, swollen, and indurated; patients are febrile, and regional lymphadenopathy (swollen glands) is often present; lesion has a marked, well-demarcated, raised border (see Figure 76-3)
Group A streptococci (Streptococcus pyogenes [sometimes groups B, C, or G streptococci])
Infants, children, and elderly individuals are most affected; primarily a clinical diagnosis
Erythrasma
Chronic infection of the keratinized layer of the epidermis; lesions are dry, scaly, itchy, and reddish brown
Corynebacterium minutissimum—possible cause
Common in diabetics; resembles dermatophyte infection
Erysipeloid
Purplish-red, nonvesiculated skin lesion with an irregular, raised border; the lesions itch and burn; fever and other systemic symptoms are uncommon
Erysipelothrix rhusiopathiae
Uncommon; considered an occupational disease
Impetigo
Erythematous (red) lesions that may be bullous (less common) or nonbullous
Nonbullous—group A streptococci (Streptococcus pyogenes)
Bullous—Staphylococcus aureus
Cellulitis
Diffuse, spreading infection involving the deeper layers of the dermis; lesions are ill-defined, flat, painful, red, and swollen; patients have fever, chills, and regional lymphadenopathy (see Figure 76-4)
Commonly: Group A streptococci, Staphylococcus aureus
Less common: Aeromonas,Vibrio spp., and Hemophilus influenzae (typically affects young children)
Primarily a clinical diagnosis
Dermatophytoses
Superficial fungal infections of the skin and its appendages (i.e., ringworm, athlete’s foot, jock itch, as well as infections of nails and hair)
Epidermophyton, Microsporum, andTrichophyton, spp.
Hidradenitis
Chronic infection of obstructed apocrine (sweat) glands in the axillas, genital, or perianal areas with intermittent discharge of often foul-smelling pus
S. aureus, Streptococcus anginosus group, anaerobic streptococci, and Bacteroides spp.
Infected pilonidal tuft cyst or hairs
Pain and swelling, redness
Anaerobes, including Bacteroides fragilis group, Prevotella, Fusobacterium, anaerobic gram-positive cocci, and Clostridium spp.
Infections of the Subcutaneous Tissues
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Skin, Soft Tissue, and Wound Infections


