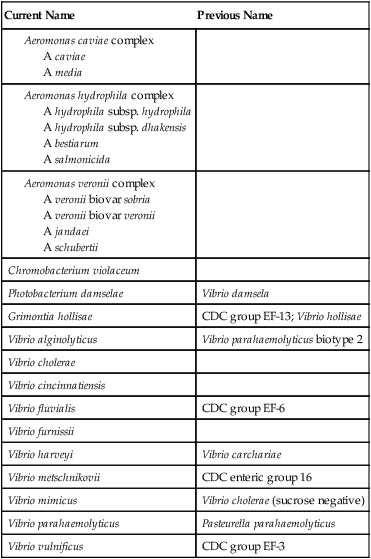
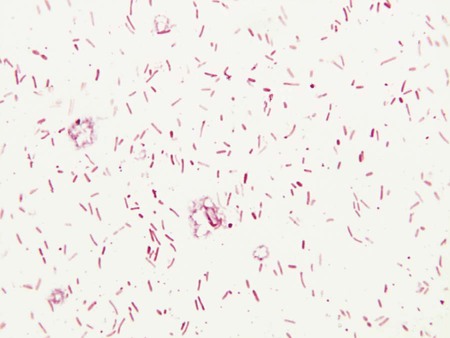
1. Describe the general characteristics of the organisms discussed in this chapter, including natural habitat, route of transmission, Gram stain reactions, and cellular morphology. 2. Describe the media used to isolate Vibrio spp. and the organisms’ colonial appearance. 3. Explain the physiologic activity of the cholera toxin and its relationship to the pathogenesis of the organism. 4. Describe the clinical significance of Aeromonas spp., Chromobacterium sp., and Vibrio spp. other than Vibrio cholerae. 5. Correlate the patient’s signs and symptoms and laboratory data to identify an infectious agent. Many aspects of the epidemiology of Vibrio spp., Aeromonas spp., and C. violaceum are similar (Table 26-1). The primary habitat for most of these organisms is water; generally, brackish or marine water for Vibrio spp., freshwater for Aeromonas spp., and soil or water for C. violaceum. Aeromonas spp. may also be found in brackish water or marine water with a low salt content. None of these organisms are considered part of the normal human flora. Transmission to humans is by ingestion of contaminated water, fresh produce, meat, dairy products, or seafood or by exposure of disrupted skin and mucosal surfaces to contaminated water. TABLE 26-1 As a notorious pathogen, V. cholerae elaborates several toxins and factors that play important roles in the organism’s virulence. Cholera toxin (CT) is primarily responsible for the key features of cholera (Table 26-2). Release of this toxin causes mucosal cells to hypersecrete water and electrolytes into the lumen of the gastrointestinal tract. The result is profuse, watery diarrhea, leading to dramatic fluid loss. The fluid loss results in severe dehydration and hypotension that, without medical intervention, frequently lead to death. This toxin-mediated disease does not require the organism to penetrate the mucosal barrier. Therefore, blood and the inflammatory cells typical of dysenteric stools are notably absent in cholera. Instead, “rice water stools,” composed of fluids and mucous flecks, are the hallmark of cholera toxin activity. TABLE 26-2 Pathogenesis and Spectrum of Diseases V. cholerae produces several other toxins and factors, but the exact role of these in disease is still uncertain (see Table 26-2). To effectively release toxin, the organism first must infiltrate and distribute itself along the cells lining the mucosal surface of the gastrointestinal tract. Motility and chemotaxis mediate the distribution of organisms, and mucinase production allows penetration of the mucous layer. Toxin coregulated pili (TCP) provide the means by which bacilli attach to mucosal cells for release of cholera toxin. Because no special considerations are required for isolation of these genera from extraintestinal sources, the general specimen collection and transport information provided in Table 5-1 is applicable. However, stool specimens suspected of containing Vibrio spp. should be collected and transported only in Cary-Blair medium. Buffered glycerol saline is not acceptable, because glycerol is toxic for vibrios. Feces is preferable, but rectal swabs are acceptable during the acute phase of diarrheal illness. Microscopically, vibrios are gram-negative, straight or slightly curved rods (Figure 26-1). When stool specimens from patients with cholera are examined using dark-field microscopy, the bacilli exhibit characteristic rapid darting or shooting-star motility. However, direct microscopic examination of stools by any method is not commonly used for laboratory diagnosis of enteric bacterial infections.
Vibrio, Aeromonas, Chromobacterium, and Related Organisms
Epidemiology
Species
Habitat (Reservoir)
Mode of Transmission
Vibrio cholerae
Niche outside of human gastrointestinal tract between occurrence of epidemics and pandemics is uncertain; may survive in a dormant state in brackish or saltwater; human carriers also are known but are uncommon
Fecal-oral route, by ingestion of contaminated washing, swimming, cooking, or drinking water; also by ingestion of contaminated shellfish or other seafood
V. alginolyticus
Brackish or saltwater
Exposure to contaminated water
V. cincinnatiensis
Unknown
Unknown
Photobacterium damsela
Brackish or saltwater
Exposure of wound to contaminated water
V. fluvialis
Brackish or saltwater
Ingestion of contaminated water or seafood
V. furnissii
Brackish or saltwater
Ingestion of contaminated water or seafood
Grimontia hollisae
Brackish or saltwater
Ingestion of contaminated water or seafood
V. metschnikovii
Brackish, salt and freshwater
Unknown
V. mimicus
Brackish or saltwater
Ingestion of contaminated water or seafood
V. parahaemolyticus
Brackish or saltwater
Ingestion of contaminated water or seafood
V. vulnificus
Brackish or saltwater
Ingestion of contaminated water or seafood
Aeromonas spp.
Aquatic environments around the world, including freshwater, polluted or chlorinated water, brackish water and, occasionally, marine water; may transiently colonize gastrointestinal tract; often infect various warm- and cold-blooded animal species
Ingestion of contaminated food (e.g., dairy, meat, produce) or, water; exposure of disrupted skin or mucosal surfaces to contaminated water or soil; traumatic inoculation of fish fins and or fishing hooks
Chromobacterium violaceum
Environmental, soil and water of tropical and subtropical regions. Not part of human flora
Exposure of disrupted skin to contaminated soil or water
Pathogenesis and Spectrum of Disease
Species
Virulence Factors
Spectrum of Disease and Infections
Vibrio cholerae
Cholera toxin; zonula occludens (Zot) toxin (enterotoxin); accessory cholera enterotoxin (Ace) toxin; O1 and O139 somatic antigens, hemolysin/cytotoxins, motility, chemotaxis, mucinase, and toxin coregulated pili (TCP) pili.
Cholera: profuse, watery diarrhea leading to dehydration, hypotension, and often death; occurs in epidemics and pandemics that span the globe. May also cause nonepidemic diarrhea and, occasionally, extra intestinal infections of wounds, respiratory tract, urinary tract, and central nervous system
V. alginolyticus
Specific virulence factors for the non–V. cholerae species are uncertain.
Ear infections, wound infections; rare cause of septicemia; involvement in gastroenteritis is uncertain
V. cincinnatiensis
Rare cause of septicemia
P. damsela
Wound infections and rare cause of septicemia
V. fluvialis
Gastroenteritis
V. furnissii
Rarely associated with human infections
Grimontia hollisae
Gastroenteritis; rare cause of septicemia
V. metschnikovii
Rare cause of septicemia; involvement in gastroenteritis is uncertain
V. mimicus
Gastroenteritis; rare cause of ear infection
V. vulnificus
Wound infections and septicemia; involvement in gastroenteritis is uncertain
Aeromonas spp.
Aeromonas spp. produce various toxins and factors, but their specific role in virulence is uncertain.
Gastroenteritis, wound infections, bacteremia, and miscellaneous other infections, including endocarditis, meningitis, pneumonia, conjunctivitis, and osteomyelitis
Chromobacterium violaceum
Endotoxin, adhesins, invasins and cytolytic proteins have been described.
Rare but dangerous infection. Begins with cellulitis or lymphadenitis and can rapidly progress to systemic infection with abscess formation in various organs and septic shock
Laboratory Diagnosis
Specimen Collection and Transport
Direct Detection Methods
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine