Skin and Its Appendages
STRUCTURE OF THE SKIN
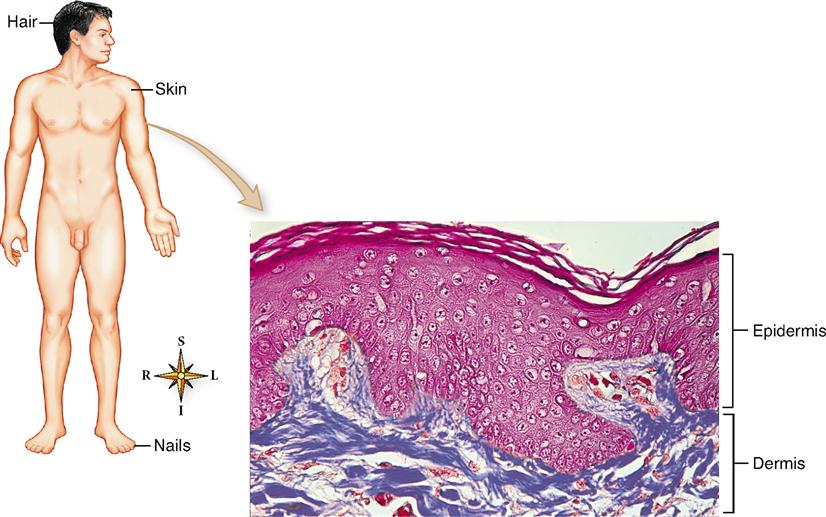
The skin is a thin, relatively flat organ classified as a membrane—the cutaneous membrane. As Figure 7-1 shows, two primary layers compose the skin:
The epidermis is an epithelial layer derived from the ectodermal germ layer of the embryo. By the seventeenth week of gestation, the epidermis of the developing baby has all the essential characteristics of the adult. The deeper dermis is derived from the mesoderm.
The dermis is a relatively dense and vascular connective tissue layer that may average more than 4 mm in thickness in some body areas. The area where the cells of the epidermis meet the connective tissue cells of the dermis is called the dermoepidermal junction (DEJ) (Figure 7-2). Beneath the dermis lies a loose hypodermis rich in fat and loose fibrous connective tissue.
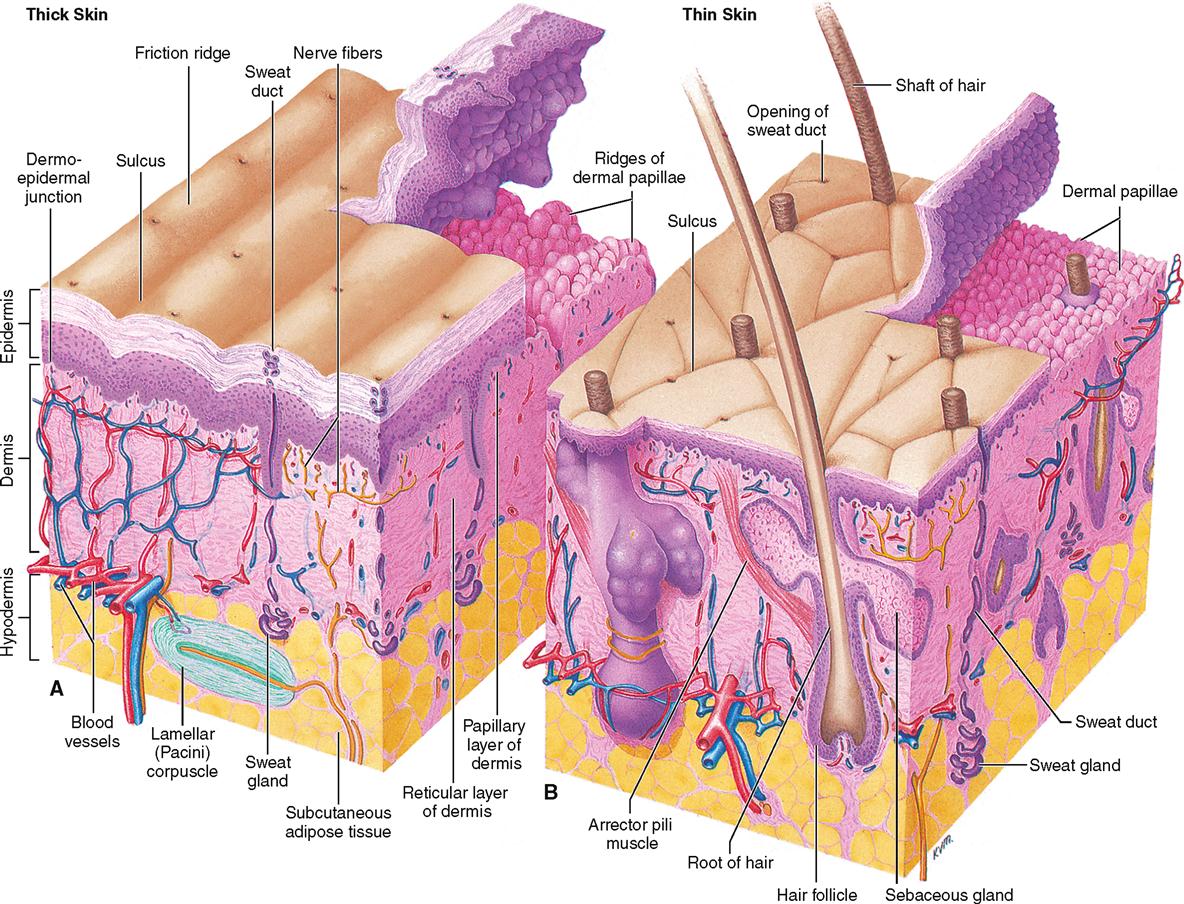
Thin and Thick Skin
Most of the body surface is covered by skin that is classified as thin skin. The hairless skin covering the palms of the hands (and fingertips), soles of the feet, and other body areas subject to friction is classified as thick skin. These terms refer only to the epidermal layer and not to overall or total skin thickness, which includes the epidermis and dermis. Total skin thickness varies from 0.5 mm in areas such as the eyelids to more than 5 mm over the back, with most of the difference accounted for by variation in depth of the dermis.
In thick skin, each of the five strata, or layers, of the epidermis described below are present, and each stratum is generally several cell layers thick. The outermost stratum—the stratum corneum—is especially noticeable in thick skin and is generally composed of many cell layers. Hair is not found in thick skin.
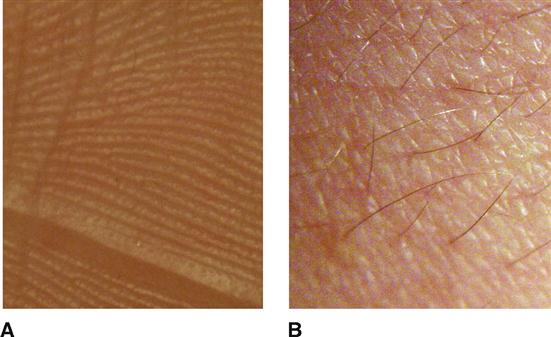
Furthermore, in thick skin the underlying dermal papillae are raised in curving parallel epidermal ridges—or friction ridges—to form fingerprints or footprints that are visible on the overlying epidermis. As their name implies, friction ridges increase friction—similar to the function of the ridges of tire treads. These ridges help us pick up and manipulate small objects with the hands and provide slip resistance to the soles of the feet. The epidermal ridges also act as sensory organs, amplifying vibrations as we lightly swipe across a textured surface. The surface of thick skin is seen in Figure 7-3, A.
In thin skin, the number of cell layers in each epidermal stratum is less than in thick skin, and one or more strata may be absent entirely. Raised parallel ridges are not present in the dermis of thin skin (Figure 7-3, B). Instead, the dermal papillae project upward individually and therefore no “fingerprints” are formed on the more superficial epidermis above.
Epidermis
CELL TYPES
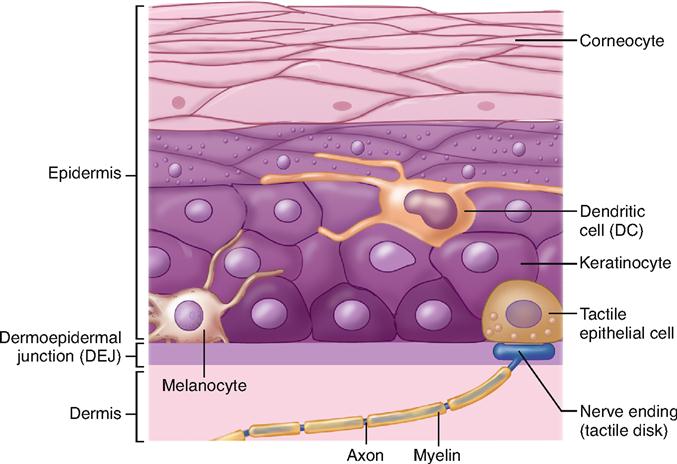
The epidermis is composed of several types of epithelial cells (Figure 7-4).
Keratinocytes eventually become filled with a tough, fibrous protein called keratin. These cells, arranged in distinct strata, or layers, are by far the most important cells in the epidermis. They make up more than 90% of the epidermal cells and form the principal structural element of the outer skin. After they are dead and fully keratinized, the flattened keratinocytes are sometimes called corneocytes.
Melanocytes contribute colored pigments to the skin and serve to decrease the amount of ultraviolet (UV) light that can penetrate into the deeper layers of the skin. Although they often compose more than 5% of the epidermal cells, melanocytes may also be completely absent from the skin in certain nonlethal conditions (Box 7-1).
Epidermal dendritic cells (DCs) of the skin, also called Langerhans cells, are branched cells that play a role in immunity. As a type of antigen-presenting cell (APC), each dendritic cell finds markers (antigens) on bacteria and other invaders and presents them to other immune system cells for recognition and destruction—an important defensive function. These cells originate in the bone marrow but migrate to the deep cell layers of the epidermis early in life. Dendritic cells and other APCs are discussed further in Chapter 24.
Tactile epithelial cells, also called Merkel cells, are located in the deepest layer of the epidermis. As Figure 7-4 shows, they connect to sensory nerve endings to form structures that serve as light touch receptors.
CELL LAYERS
The cells of the epidermis are found in up to five distinct layers, or strata. Each stratum (meaning “layer”) is named for its structural or functional characteristics. The strata of the epidermis are listed here in order from deepest to most superficial.
The stratum corneum is sometimes called the barrier area of the skin because it functions as a barrier to water loss and to many environmental threats ranging from microorganisms and harmful chemicals to physical trauma. Once this barrier layer is damaged, the effectiveness of the skin as a protective covering is greatly reduced, and most contaminants can easily pass through the lower layers of the cellular epidermis. If the glycophospholipid barrier is washed away by prolonged soaking in water (especially if the water contains lipid-dissolving detergents), the keratin may absorb water and make the skin appear puffy and wrinkled—most easily seen in thick skin because of its high water content. Certain diseases of the skin cause the stratum corneum layer of the epidermis to thicken far beyond normal limits—a condition called hyperkeratosis. The result is a thick, dry, scaly skin that is inelastic and subject to painful fissures.
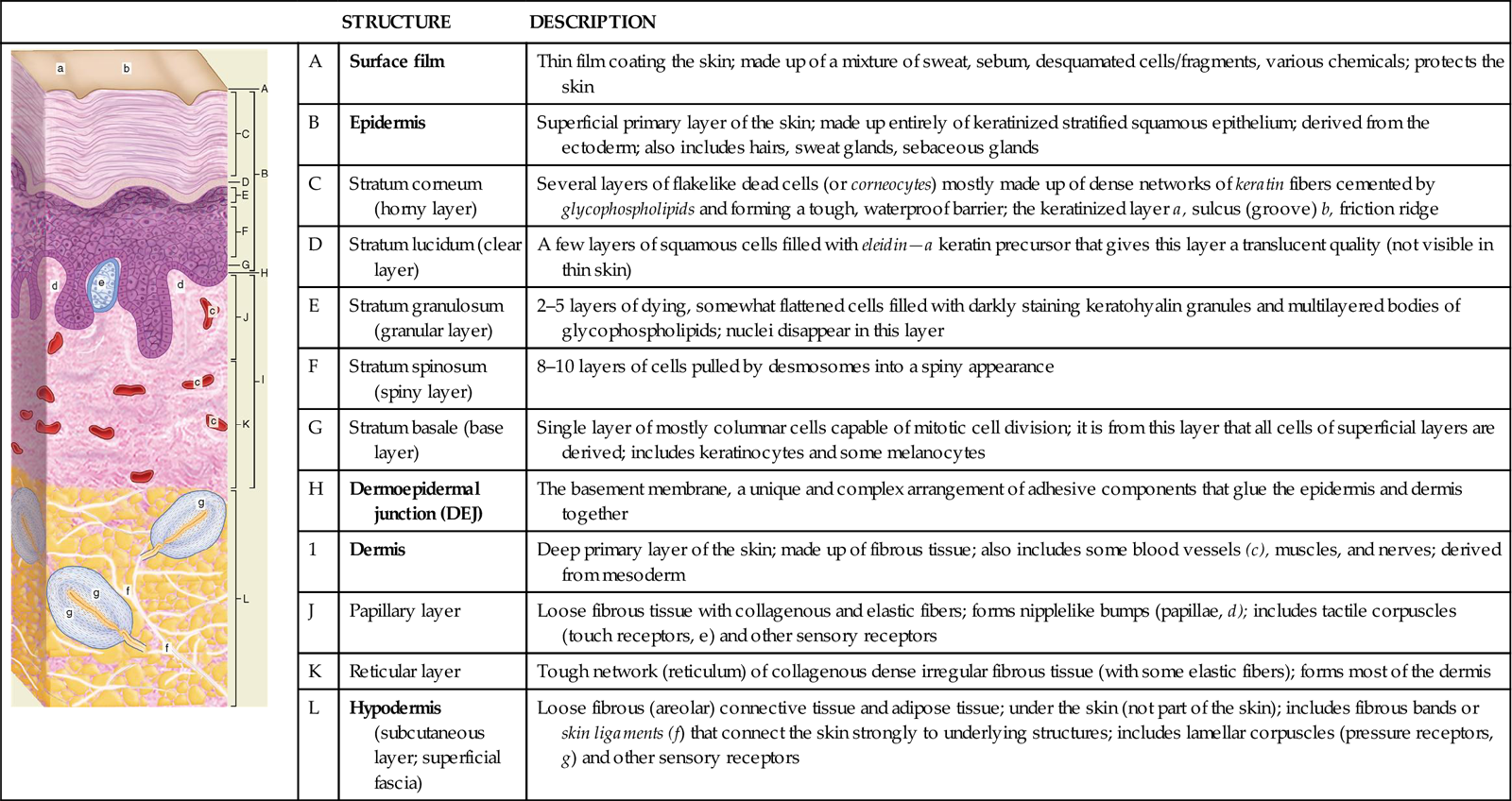
Table 7-1 clearly shows each of these layers of the epidermis.
TABLE 7-1
| STRUCTURE | DESCRIPTION | ||
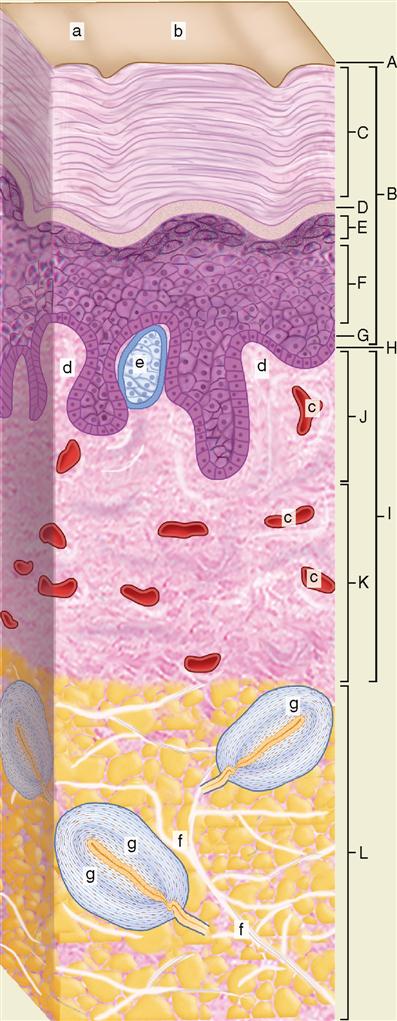 | A | Surface film | Thin film coating the skin; made up of a mixture of sweat, sebum, desquamated cells/fragments, various chemicals; protects the skin |
| B | Epidermis | Superficial primary layer of the skin; made up entirely of keratinized stratified squamous epithelium; derived from the ectoderm; also includes hairs, sweat glands, sebaceous glands | |
| C | Stratum corneum (horny layer) | Several layers of flakelike dead cells (or corneocytes) mostly made up of dense networks of keratin fibers cemented by glycophospholipids and forming a tough, waterproof barrier; the keratinized layer a, sulcus (groove) b, friction ridge | |
| D | Stratum lucidum (clear layer) | A few layers of squamous cells filled with eleidin—a keratin precursor that gives this layer a translucent quality (not visible in thin skin) | |
| E | Stratum granulosum (granular layer) | 2–5 layers of dying, somewhat flattened cells filled with darkly staining keratohyalin granules and multilayered bodies of glycophospholipids; nuclei disappear in this layer | |
| F | Stratum spinosum (spiny layer) | 8–10 layers of cells pulled by desmosomes into a spiny appearance | |
| G | Stratum basale (base layer) | Single layer of mostly columnar cells capable of mitotic cell division; it is from this layer that all cells of superficial layers are derived; includes keratinocytes and some melanocytes | |
| H | Dermoepidermal junction (DEJ) | The basement membrane, a unique and complex arrangement of adhesive components that glue the epidermis and dermis together | |
| 1 | Dermis | Deep primary layer of the skin; made up of fibrous tissue; also includes some blood vessels (c), muscles, and nerves; derived from mesoderm | |
| J | Papillary layer | Loose fibrous tissue with collagenous and elastic fibers; forms nipplelike bumps (papillae, d); includes tactile corpuscles (touch receptors, e) and other sensory receptors | |
| K | Reticular layer | Tough network (reticulum) of collagenous dense irregular fibrous tissue (with some elastic fibers); forms most of the dermis | |
| L | Hypodermis (subcutaneous layer; superficial fascia) | Loose fibrous (areolar) connective tissue and adipose tissue; under the skin (not part of the skin); includes fibrous bands or skin ligaments (f) that connect the skin strongly to underlying structures; includes lamellar corpuscles (pressure receptors, g) and other sensory receptors |
EPIDERMAL GROWTH AND REPAIR
The most important function of the integument—protection—largely depends on the special structural features of the epidermis and its ability to create and repair itself after injury or disease.
Turnover time and regeneration time are terms used to describe the period required for a population of cells to mature and reproduce. Obviously, as the surface cells of the stratum corneum are lost, replacement of keratinocytes by mitotic activity must occur. New cells must be formed at the same rate that old keratinized cells flake off from the stratum corneum to maintain a constant thickness of the epidermis. Cells push upward from the stratum basale into each successive layer, die, become keratinized, and eventually desquamate (fall away), as did their predecessors. This fact illustrates a physiological principle: while life continues, the body’s work is never done. Even at rest it is producing millions upon millions of new cells to replace old ones.
A cell-signaling protein called epidermal growth factor (EGF) plays a role in regulating the regeneration and repair of the epidermis, as its name suggests. Discovery of EGF has led to its use as a therapy to stimulate skin repairs in diabetic and pressure ulcers and other conditions. EGF requires the hormone insulin-like growth factor 1 (EGF-1) to have its full effect in stimulating skin growth and repair. Growth hormone (GH) also has a growth-promoting effect on epidermal cells. The cooperative actions of hormones are explored further in Chapters 18 and 19.
Research suggests that the regeneration time required for completion of mitosis, differentiation, and movement of new keratinocytes from the stratum basale to the surface of the epidermis is about 35 days. The process can be accelerated by abrasion of the skin surface, which tends to peel off a few of the cell layers of the stratum corneum. The result is an intense stimulation of mitotic activity in the stratum basale and a shortened turnover period. If abrasion continues over a prolonged period, the increase in mitotic activity and shortened turnover time will result in an abnormally thick stratum corneum and the development of calluses at the point of friction or irritation. Although callus formation is a normal and protective response of the skin to friction, several skin diseases are also characterized by abnormally high mitotic activity in the epidermis. In such conditions, the thickness of the corneum is dramatically increased. As a result, scales accumulate and skin lesions often develop.
Normally, about 10% to 12% of all cells in the stratum basale enter mitosis each day. Cells migrating to the surface proceed upward in vertical columns from discrete groups of 8 to 10 of these basal cells undergoing mitosis. Each group of active basal cells, together with its vertical columns of migrating keratinocytes, is called an epidermal proliferating unit, or EPU. Keratinization proceeds as the cells migrate toward the stratum corneum. As mitosis continues and new basal cells enter the column and migrate upward, fully keratinized “dead” cells are sloughed off at the skin surface. Numerous skin diseases are characterized by an abnormally high rate of keratinization.
Dermoepidermal Junction
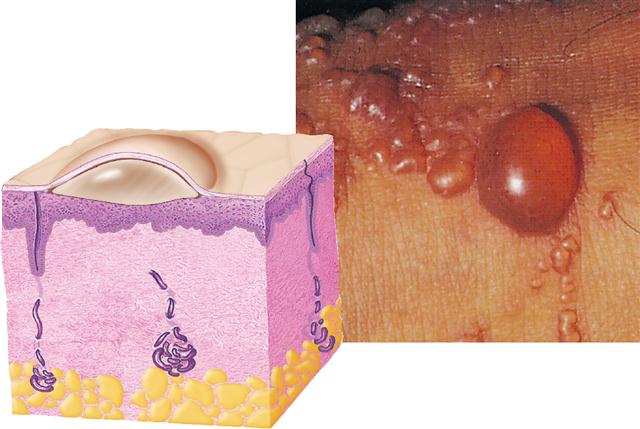
Electron microscopy and histochemical studies have demonstrated the existence of a rather unique area between the epidermis and dermis called the dermoepidermal junction (DEJ).
The DEJ is a unique kind of basement membrane (BM) that includes special fibrous elements and a unique polysaccharide gel that strongly cement the superficial epidermis to the dermis below. The junction “glues” the two layers together and provides mechanical support for the epidermis, which is attached to its upper surface. Box 7-2 shows what happens when this “skin glue” fails.
In addition, the DEJ serves as a partial barrier to the passage of some cells and large molecules. Certain dyes, for example, if injected into the dermis cannot passively diffuse upward into the epidermis unless the junctional barrier is damaged by heat, enzymes, or other chemicals that change its permeability characteristics. Although the junction is remarkably effective in preventing separation of the two skin layers, even when they are subjected to relatively high shear force, this barrier is thought to have only a limited role in preventing passage of harmful chemicals or disease-causing organisms through the skin from the external environment. Any widespread detachment of a large area of epidermis from the dermis is an extremely serious condition that may result in overwhelming infection and death.
Dermis
The dermis, or corium, is sometimes called the “true skin.” It is composed of two layers—a thin papillary layer and a thicker reticular layer. The dermis is much thicker than the epidermis and may exceed 4 mm on the soles and palms. It is thinnest on the eyelids and penis, where it seldom exceeds 0.5 mm. As a rule of thumb, the dermis on the ventral surface of the body and over the appendages is generally thinner than on the dorsal surface. The mechanical strength of the skin is in the dermis. In addition to serving a protective function against mechanical injury and compression, this layer of the skin provides a reservoir storage area for water and important electrolytes. A widespread network of nerves and nerve endings in the dermis called somatic sensory receptors also process sensory information such as pain, pressure, touch, and temperature. Sensory receptors are discussed in detail in Chapter 17. At various levels of the dermis extend a variety of muscle fibers, hair follicles, sweat and sebaceous glands, and many blood vessels. It is the rich vascular supply of the dermis that plays a critical role in regulation of body temperature—a function described later in the chapter.
PAPILLARY LAYER
Note in Figure 7-2 that the thin superficial layer of the dermis forms bumps, called dermal papillae, that project into the epidermis. Papilla (plural, papillae) is the Latin word for “nipple” and is used often in anatomy to name any small, nipplelike bump. The papillary layer takes its name from the papillae on its surface. Between the sculptured surface of the papillary layer and the stratum basale lies the important dermoepidermal junction.
The papillary layer and its papillae are composed essentially of loose fibrous connective tissue elements and a fine network of thin collagenous and elastic fibers. The thin epidermal layer of the skin conforms tightly to the ridges of dermal papillae. As a result, the epidermis also has characteristic ridges on its surface. Epidermal ridges are especially well defined on the tips of the fingers and toes. In each of us they form a unique pattern—an anatomical fact made famous by the art of fingerprinting. These ridges perform a function that is very important to human survival: they allow us to grip surfaces well enough to walk upright on slippery surfaces and to grasp and use tools. For that reason, they are usually called friction ridges.
RETICULAR LAYER
The thick reticular layer of the dermis consists of a much more dense reticulum, or network of fibers, than is seen in the papillary layer above it. It is this dense layer of tough and interlacing white collagenous fibers that when commercially processed from animal skin, results in leather. Although most of the fibers in this layer are of the collagenous type, which gives toughness to the skin, elastic fibers are also present. These fibers make the skin stretchable and elastic (able to rebound).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree