Central Nervous System
COVERINGS OF THE BRAIN AND SPINAL CORD
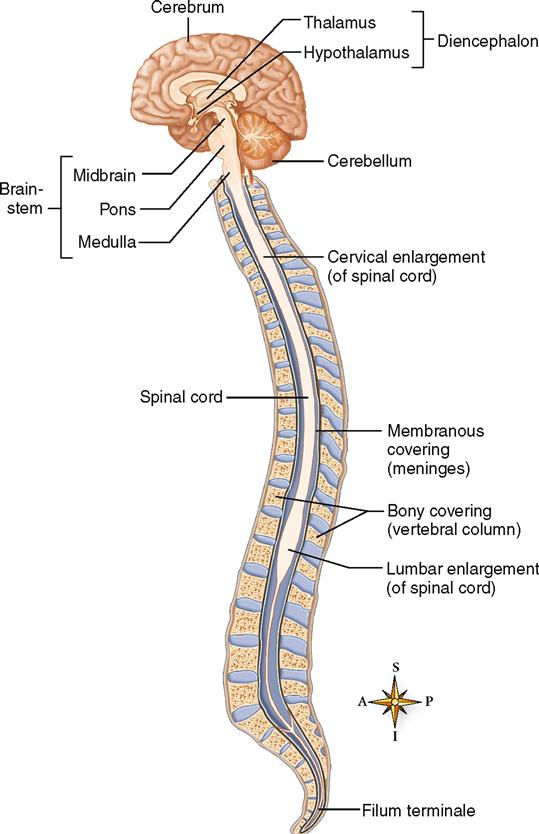
Because the brain and spinal cord are both delicate and vital, nature has provided them with two protective coverings. The outer covering consists of bone: cranial bones encase the brain; vertebrae encase the spinal cord. The inner covering consists of membranes known as meninges. Three distinct layers compose the meninges:
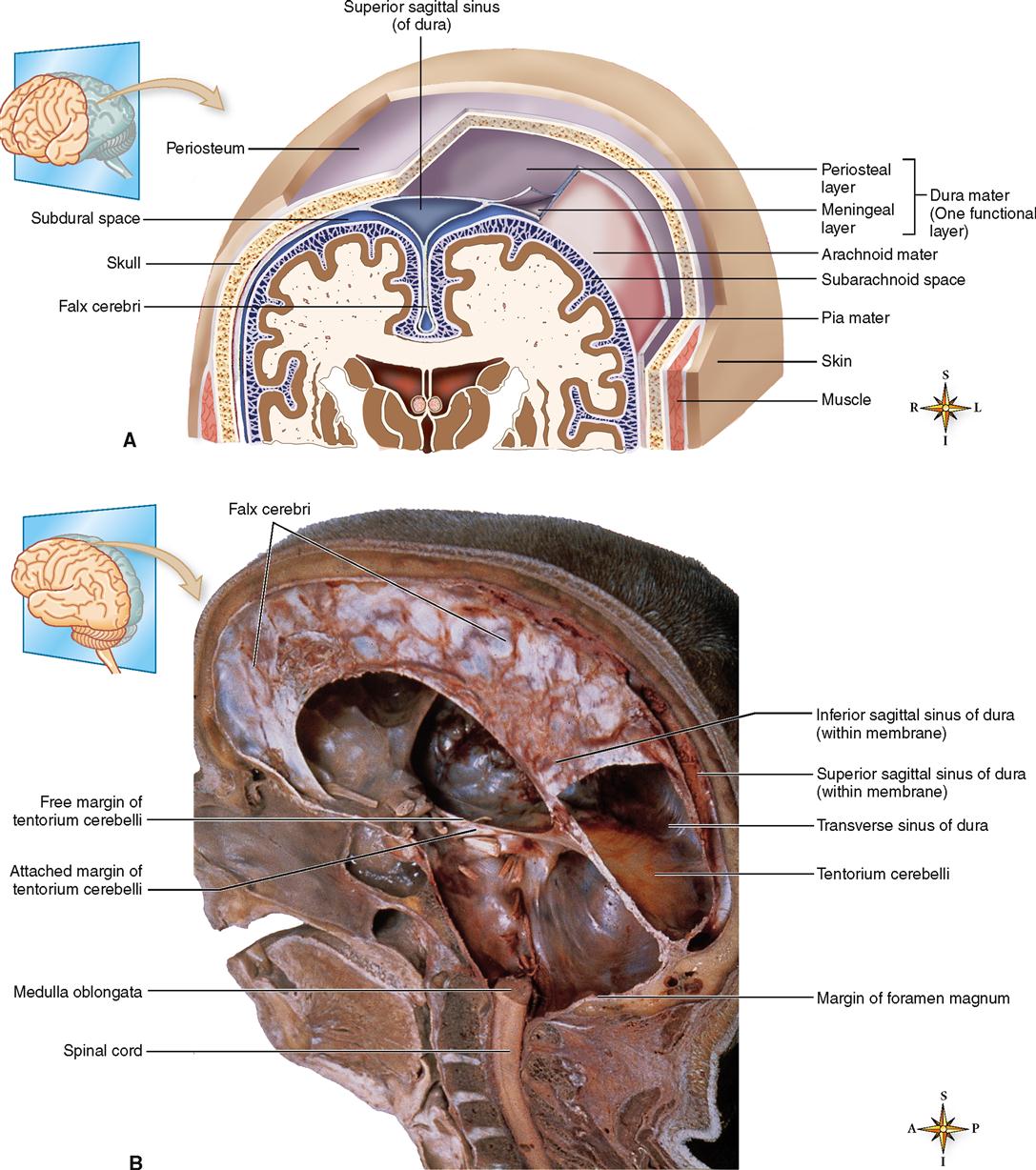
Observe their respective locations in Figures 14-2 and 14-3. The dura mater, made of strong white fibrous tissue, serves as the outer layer of the meninges and also as the inner periosteum of the cranial bones. The arachnoid mater, a delicate, spiderweb-like layer, lies between the dura mater and the pia mater, or innermost layer of the meninges. The transparent pia mater adheres to the outer surface of the brain and spinal cord and contains blood vessels.
The dura mater has three important inward extensions:
1. Falx cerebri. The falx cerebri projects downward into the longitudinal fissure to form a kind of partition between the two cerebral hemispheres. The Latin word falx means “sickle” and refers to the curving sickle shape of this partition as it extends from the roof of the cranial cavity (see Figure 14-2, B).
Figure 14-2 shows a large space within the dura, where the falx cerebri begins to descend between the left and right cerebral hemispheres. This space, called the superior sagittal sinus, is one of several dural sinuses. Dural sinuses function as venous reservoirs, collecting blood from brain tissues for the return trip to the heart.
A number of spaces lie between and around the meninges (see Figure 14-2). Three of these spaces are the following:
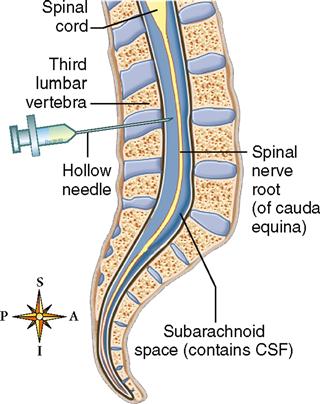
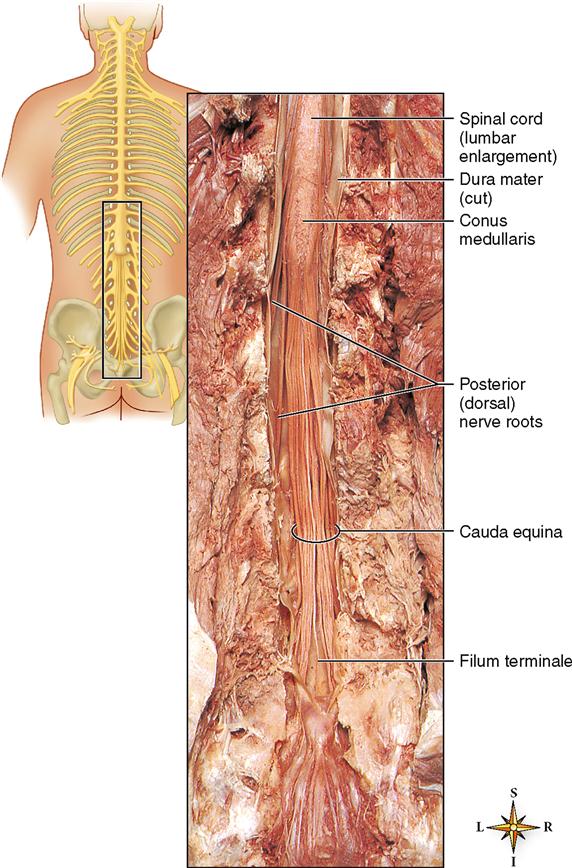
The meninges of the cord (see Figure 14-3) continue on down inside the spinal cavity for some distance below the end of the spinal cord. The pia mater forms a slender filament known as the filum terminale (see Figure 14-1). At the level of the third segment of the sacrum, the filum terminale blends with the dura mater to form a fibrous cord that disappears in the periosteum of the coccyx.
Infections of the meninges are discussed in Box 14-1.
CEREBROSPINAL FLUID
In addition to its bony and membranous coverings, nature has further protected the brain and spinal cord against injury by providing a cushion of fluid both around the organs and within them. This fluid is the cerebrospinal fluid (CSF). The CSF does more than simply provide a supportive, protective cushion, however. It is also a reservoir of circulating fluid that, along with blood, the brain monitors for changes in the internal environment. For example, changes in the carbon dioxide (CO2) content of CSF trigger homeostatic responses in the respiratory control centers of the brainstem that help regulate the overall CO2 content and pH of the body.
Fluid Spaces
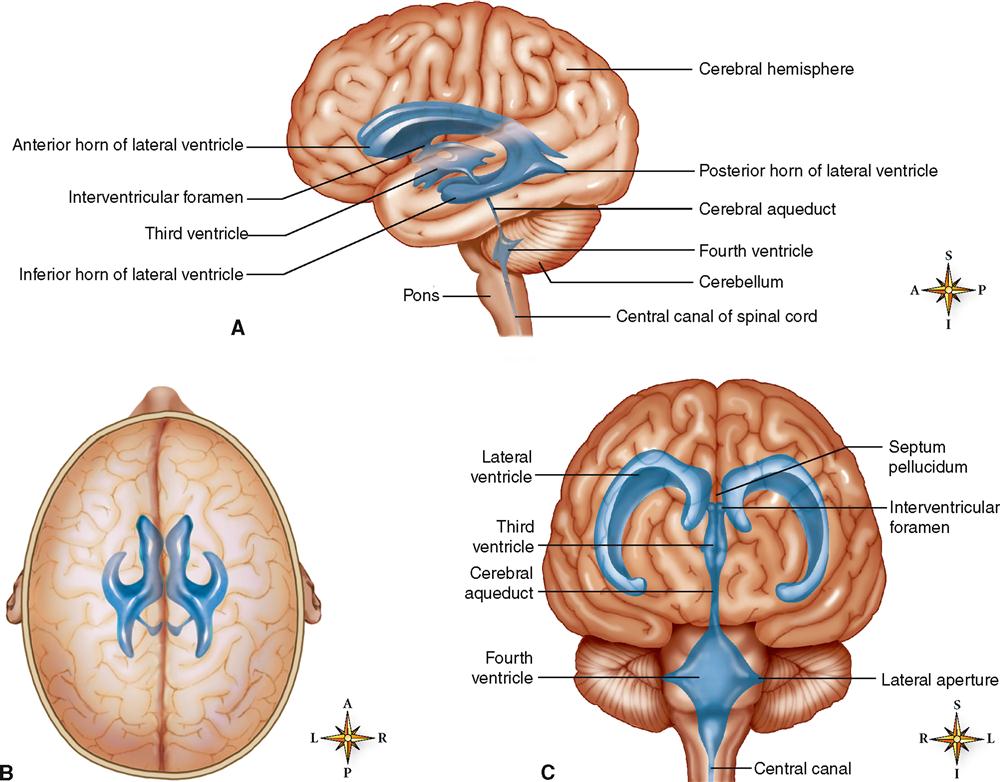
Cerebrospinal fluid is found in the subarachnoid space around the brain and spinal cord and within the cavities and canals of the brain and spinal cord.
The four large, fluid-filled spaces within the brain are called ventricles. Two of them, the lateral (or first and second) ventricles, are located one in each hemisphere of the cerebrum. As you can see in Figure 14-4, the third ventricle is little more than a thin, vertical pocket of fluid below and medial to the lateral ventricles. The fourth ventricle is a tiny, diamond-shaped space where the cerebellum attaches to the back of the brainstem. Actually, the fourth ventricle is simply a slight expansion of the central canal extending up from the spinal cord.
Formation and Circulation of Cerebrospinal Fluid
Formation of CSF occurs mainly by separation of fluid from blood in the choroid plexuses. Choroid plexuses are networks of capillaries that project from the pia mater into the lateral ventricles and into the roofs of the third and fourth ventricles. Each choroid plexus is covered with a sheet of a special type of ependymal (glial) cell that releases the CSF into the fluid spaces. From each lateral ventricle the fluid seeps through an opening, the interventricular foramen (of Monro), into the third ventricle, then through a narrow channel, the cerebral aqueduct (of Sylvius), into the fourth ventricle (Figure 14-5). Some of the fluid moves from the fourth ventricle directly into the central canal of the cord. Some of it moves out of the fourth ventricle through openings in its roof, two lateral foramina (of Luschka) and one median foramen (of Magendie). These openings allow CSF to move into the cisterna magna, a space behind the medulla that is continuous with the subarachnoid space around the brain and cord. The fluid circulates in the subarachnoid space and then is absorbed into venous blood through the arachnoid villi (fingerlike projections of the arachnoid mater into the brain’s venous sinuses). Briefly, here is the circulation route of cerebrospinal fluid: it is formed as fluid is separated from blood in the choroid plexuses, then it flows into the ventricles of the brain, circulates through the ventricles and into the central canal and subarachnoid spaces, and is then absorbed back into blood.
The amount of CSF in the average adult is about 140 ml (about 23 ml in the ventricles and 117 ml in the subarachnoid space of brain and cord). Box 14-2 explains the diagnostic value of testing a patient’s cerebrospinal fluid.
SPINAL CORD
Structure of the Spinal Cord
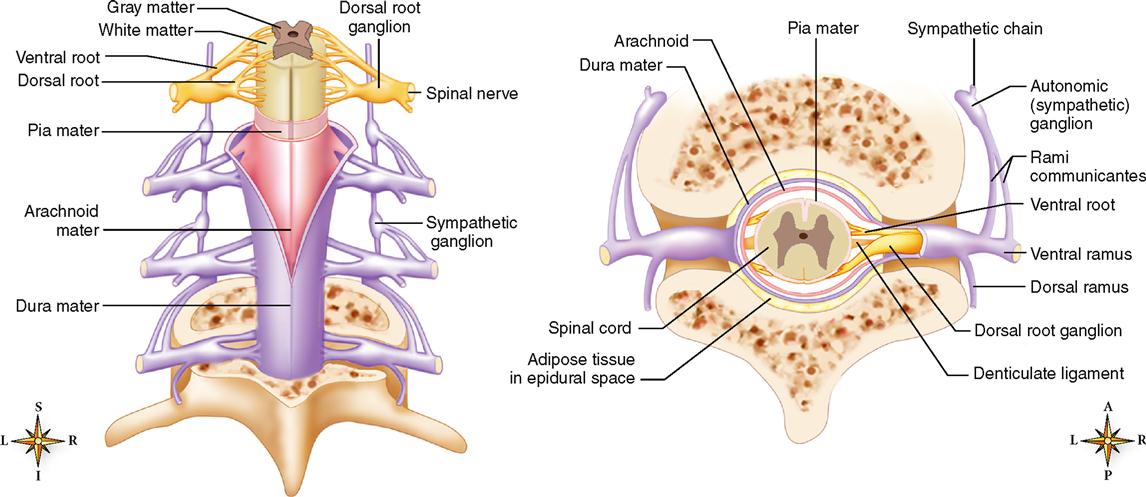
The spinal cord lies within the spinal cavity, extending from the foramen magnum to the lower border of the first lumbar vertebra (Figure 14-6), a distance of about 45 cm (18 inches) in the average body. The spinal cord does not completely fill the spinal cavity—which also contains the meninges, CSF, a cushion of adipose tissue, and blood vessels.
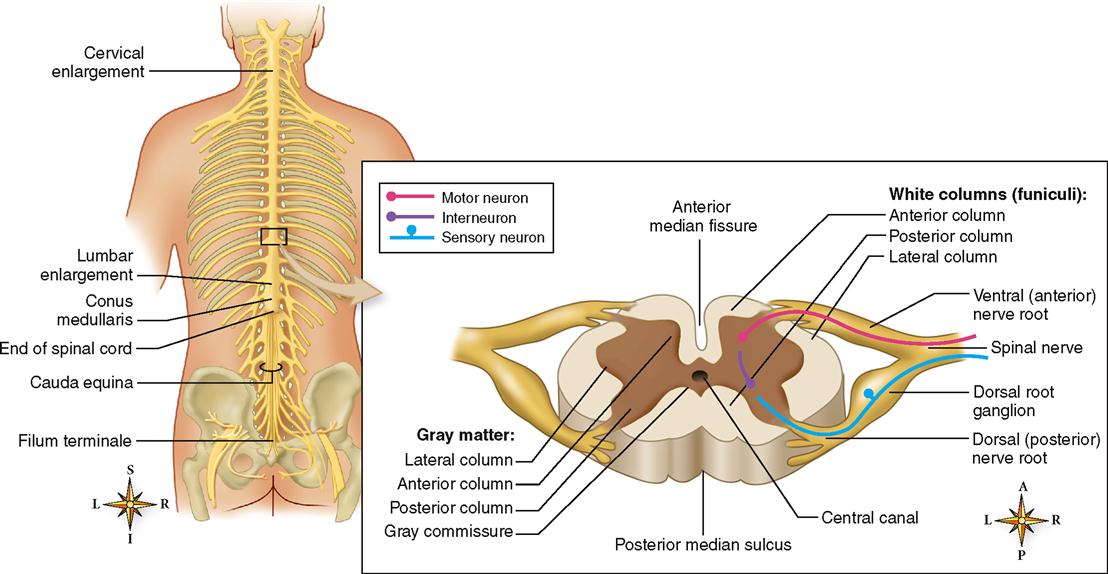
The spinal cord is an oval-shaped cylinder that tapers slightly as it descends and has two bulges, one in the cervical region and the other in the lumbar region (see Figure 14-6). Two deep grooves, the anterior median fissure and the posterior median sulcus, just miss dividing the cord into separate symmetrical halves. The anterior fissure is the deeper and the wider of the two grooves—a useful factor to remember when you examine spinal cord diagrams. It enables you to tell at a glance which part of the cord is anterior and which is posterior.
Two bundles of nerve fibers called nerve roots project from each side of the spinal cord (see Figure 14-6). Fibers comprising the dorsal (posterior) nerve root carry sensory information into the spinal cord. Cell bodies of these unipolar, sensory neurons make up a small region of gray matter in the dorsal nerve root called the dorsal (posterior) root ganglion. Fibers of the ventral (anterior) nerve root carry motor information out of the spinal cord. Cell bodies of these multipolar, motor neurons are in the gray matter that composes the inner core of the spinal cord. Numerous interneurons are also located in the gray matter core of the spinal cord. On each side of the spinal cord, the dorsal and ventral nerve roots join together to form a single mixed nerve called, simply, a spinal nerve. Spinal nerves, components of the peripheral nervous system, are considered in more detail in the next chapter.
The spinal cord ends at vertebra L1 in a tapered cone called the conus medullaris. As you can see in Figure 14-7, many nerve roots extending from the conus medullaris form a sort of “horse tail” of spinal nerve roots called the cauda equina. Within the cauda equina the long cordlike filum terminale is formed from the spinal meninges.
Although the gray matter core of the spinal cord looks like a flat letter H in transverse sections of the cord, it actually has three dimensions, because the gray matter extends the length of the cord. The H-shaped rod of gray matter is made up of anterior, lateral, and posterior gray columns. When viewed in a cross section, as in Figure 14-6, the columns forming the H appear to spread out like animal horns—and thus are also called anterior, posterior, and lateral gray horns. The left and right gray columns are joined in the middle by a band called the gray commissure. It is through the gray commissure that the central canal carries CSF through the spinal cord. The gray columns consist predominantly of cell bodies of interneurons and motor neurons.
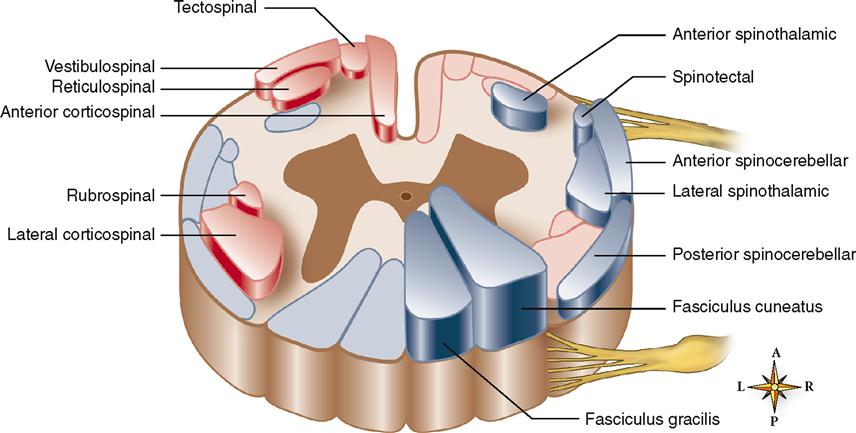
White matter surrounding the gray matter is subdivided in each half of the cord into three white columns or funiculi: the anterior, posterior, and lateral white columns. Each white column, or funiculus, consists of a large bundle of nerve fibers (axons) divided into smaller bundles called spinal tracts, shown in Figure 14-8. The names of most spinal cord tracts indicate the white column in which the tract is located, the structure in which the axons that make up the tract originate, and the structure in which they terminate. For example, the lateral corticospinal tract is located in the lateral white column of the cord. The axons that compose it originate from neuron cell bodies in the spinal cortex (of the cerebrum) and terminate in the spinal cord. The anterior spinothalamic tract lies in the anterior white column. The axons that compose it originate from neuron cell bodies in the spinal cord and terminate in a portion of the brain called the thalamus.
You may wish to refer to the atlas that accompanies this book, where you will find detailed photographs of a human spinal cord. How many structures can you identify in the atlas by sight?
Functions of the Spinal Cord
The spinal cord performs two general functions. Briefly, it provides conduction routes to and from the brain and serves as the integrator, or reflex center, for all spinal reflexes.
Spinal cord tracts provide conduction paths to and from the brain. Ascending tracts conduct sensory impulses up the cord to the brain. Descending tracts conduct motor impulses down the cord from the brain. Bundles of axons compose all tracts.
Tracts are both structural and functional organizations of the nerve fibers of the spinal cord. They are structural organizations in that all the axons of any one tract originate from neuron cell bodies located in the same area of the central nervous system, and all the axons terminate in a single structure elsewhere in the central nervous system. For example, all the fibers of the spinothalamic tract are axons originating from neuron cell bodies located in the spinal cord and terminating in the thalamus. Tracts are functional organizations in that all the axons that compose one tract serve one general function. For instance, fibers of the spinothalamic tracts serve a sensory function. They transmit impulses that produce the sensations of crude touch, pain, and temperature.
Because so many different tracts make up the white columns of the cord, we mention only a few of the more important ones. Locate each tract in Figure 14-8. Consult Tables 14-1 and 14-2 for a brief summary of these tracts.
TABLE 14-1
Major Ascending Tracts of Spinal Cord
| NAME | FUNCTION | LOCATION | ORIGIN* | TERMINATION† |
| Lateral spinothalamic | Pain, temperature, and crude touch on opposite side | Lateral white columns | Posterior gray column on opposite side | Thalamus |
| Anterior spinothalamic | Crude touch and pressure | Anterior white columns | Posterior gray column on opposite side | Thalamus |
| Fasciculi gracilis and cuneatus | Discriminating touch and pressure sensations, including vibration, stereognosis, and two-point discrimination; also conscious kinesthesia | Posterior white columns | Spinal ganglia on same side | Medulla |
| Anterior and posterior spinocerebellar | Unconscious kinesthesia | Lateral white columns | Anterior or posterior gray column | Cerebellum |
| Spinotectal | Touch related to visual reflexes | Lateral white columns | Posterior gray columns | Superior colliculus (midbrain) |
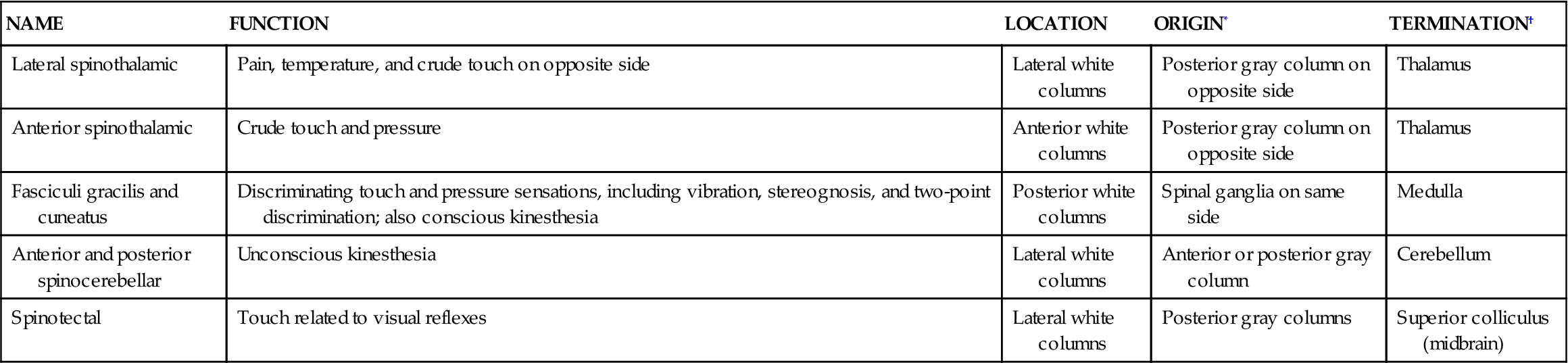
*Location of cell bodies of neurons from which axons of tract arise.
TABLE 14-2
Major Descending Tracts of Spinal Cord
| NAME | FUNCTION | LOCATION | ORIGIN* | TERMINATION† |
| Lateral corticospinal (or crossed pyramidal) | Voluntary movement, contraction of individual or small groups of muscles, particularly those moving hands, fingers, feet, and toes of opposite side | Lateral white columns | Motor areas or cerebral cortex of opposite side from tract location in cord | Lateral or anterior gray columns |
| Anterior corticospinal (direct pyramidal) | Same as lateral corticospinal except mainly muscles of same side | Anterior white columns | Motor cortex but on same side as location in cord | Lateral or anterior gray columns |
| Reticulospinal | Maintain posture during movement | Anterior white columns | Reticular formation (midbrain, pons, medulla) | Anterior gray columns |
| Rubrospinal | Coordination of body movement and posture | Lateral white columns | Red nucleus (of midbrain) | Anterior gray columns |
| Tectospinal | Head and neck movement during visual reflexes | Anterior white columns | Superior colliculus (midbrain) | Medulla and anterior gray columns |
| Vestibulospinal | Coordination of posture/balance | Anterior white columns | Vestibular nucleus (pons, medulla) | Anterior gray columns |
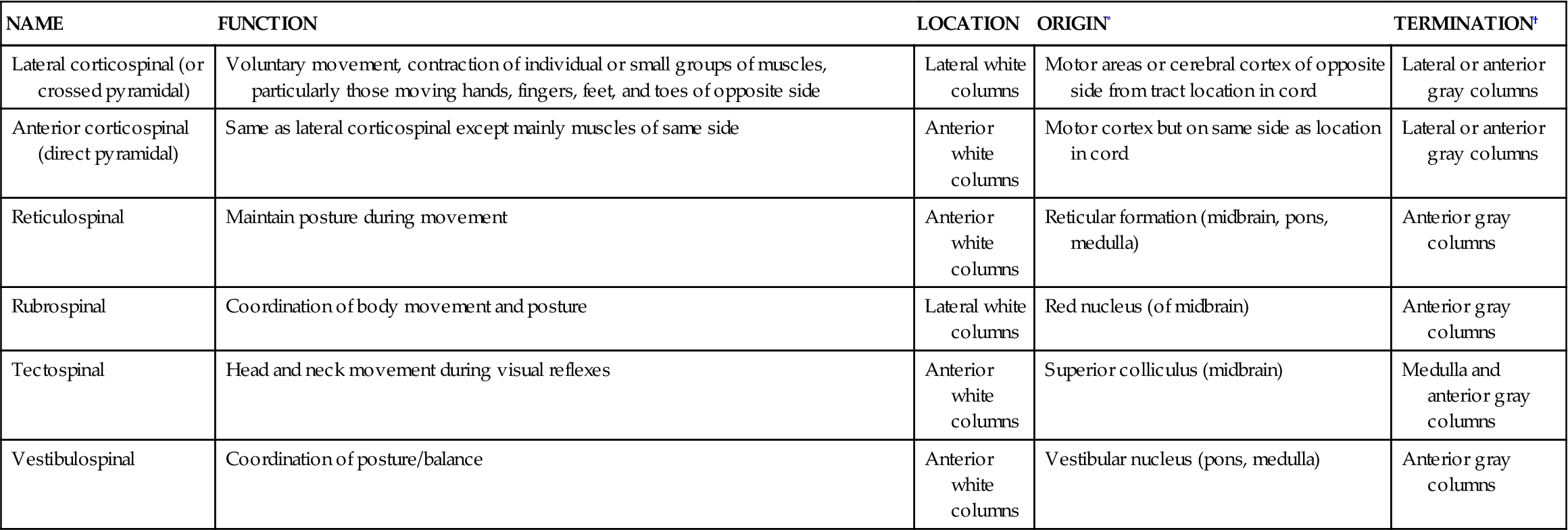
*Location of cell bodies of neurons from which axons of tract arise.
Five important ascending, or sensory, tracts and their functions, stated very briefly, are as follows:
1. Lateral spinothalamic tracts: crude touch, pain, and temperature
2. Anterior spinothalamic tracts: crude touch and pressure
4. Spinocerebellar tracts: subconscious kinesthesia
Further discussion of the sensory neural pathways may be found on pp. 506–507.
Six important descending, or motor, tracts and their functions described in brief are as follows:
2. Anterior corticospinal tracts: same as preceding except mainly muscles of same side of body
3. Reticulospinal tracts: help maintain posture during skeletal muscle movements
4. Rubrospinal tracts: transmit impulses that coordinate body movements and maintenance of posture
5. Tectospinal tracts: head and neck movement related to visual reflexes
6. Vestibulospinal tracts: coordination of posture and balance
Further discussion of motor neural pathways may be found on pp. 490–491.
The spinal cord also serves as the reflex center for all spinal reflexes. The term reflex center means the center of a reflex arc or the place in the arc where incoming sensory impulses become outgoing motor impulses. They are structures that switch impulses from afferent to efferent neurons. In two-neuron arcs, reflex centers are merely synapses between neurons. In all other arcs, reflex centers consist of interneurons interposed between afferent and efferent neurons. Spinal reflex centers are located in the gray matter of the cord.
BRAIN
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree