High-Yield Terms to Learn
Depolarizing blockade Neuromuscular paralysis that results from persistent depolarization of the end plate (eg, by succinylcholine) Desensitization A phase of blockade by a depolarizing blocker during which the end plate repolarizes but is less than normally responsive to agonists (acetylcholine or succinylcholine) Malignant hyperthermia Hyperthermia that results from massive release of calcium from the sarcoplasmic reticulum, leading to uncontrolled contraction and stimulation of metabolism in skeletal muscle Nondepolarizing blockade Neuromuscular paralysis that results from pharmacologic antagonism at the acetylcholine receptor of the end plate (eg, by tubocurarine) Spasmolytic A drug that reduces abnormally elevated muscle tone (spasm) without paralysis (eg, baclofen, dantrolene) Stabilizing blockade Synonym for nonpolarizing blockade
Neuromuscular Blocking Drugs
Classification and Prototypes
Skeletal muscle contraction is evoked by a nicotinic cholinergic transmission process. Blockade of transmission at the end plate (the postsynaptic structure bearing the nicotinic receptors) is clinically useful in producing muscle relaxation, a requirement for surgical relaxation, tracheal intubation and control of ventilation. The neuromuscular blockers are quaternary amines structurally related to acetylcholine (ACh). Most are antagonists (nondepolarizing type), and the prototype is tubocurarine. One neuromuscular blocker used clinically, succinylcholine, is an agonist at the nicotinic end plate receptor (depolarizing type).
Nondepolarizing Neuromuscular Blocking Drugs
Pharmacokinetics
All agents are given parenterally. They are highly polar drugs and do not cross the blood-brain barrier. Drugs that are metabolized (eg, mivacurium, by plasma cholinesterase) or eliminated in the bile (eg, vecuronium) have shorter durations of action (10-20 min) than those eliminated by the kidney (eg, metocurine, pancuronium, pipecuronium, and tubocurarine) which usually have durations of action of less than 35 min. In addition to hepatic metabolism, atracurium clearance involves rapid spontaneous breakdown (Hofmann elimination) to form laudanosine and other products. At high blood levels, laudanosine may cause seizures. Cisatracurium, a stereoisomer of atracurium, is also inactivated spontaneously but forms less laudanosine and currently is one of the most commonly used muscle relaxants in clinical practice.
Mechanism of Action
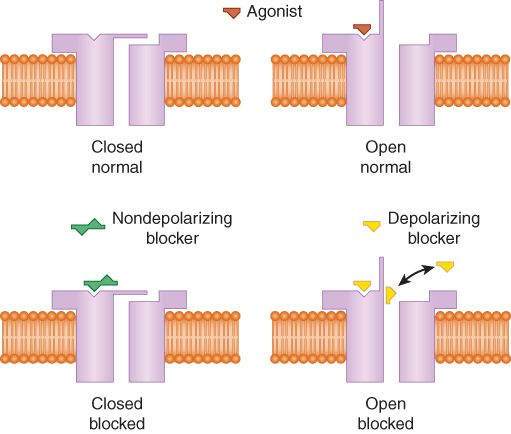
Nondepolarizing drugs prevent the action of ACh at the skeletal muscle end plate (Figure 27-1). They act as surmountable blockers. (That is, the blockade can be overcome by increasing the amount of agonist [ACh] in the synaptic cleft.) They behave as though they compete with ACh at the receptor, and their effect is reversed by cholinesterase inhibitors. Some drugs in this group may also act directly to plug the ion channel operated by the ACh receptor. Post-tetanic potentiation is preserved in the presence of these agents, but tension during the tetanus fades rapidly. See Table 27-1 for additional details. Larger muscles (eg, abdominal, diaphragm) are more resistant to neuromuscular blockade, but they recover more rapidly than smaller muscles (eg, facial, hand). Of the available nondepolarizing drugs, rocuronium (60-120 s) has the most rapid onset time.
FIGURE 27-1
Drug interactions with the acetylcholine (ACh) receptor on the skeletal muscle end plate. Top: ACh, the normal agonist, opens the sodium channel. Bottom left: Nondepolarizing blockers bind to the receptor to prevent opening of the channel. Bottom right: Succinylcholine causes initial depolarization (fasciculation) and then persistent depolarization of the channel, which leads to muscle relaxation.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 27-6.)
TABLE 27-1 Comparison of a typical nondepolarizing neuromuscular blocker (tubocurarine) and a depolarizing blocker (succinylcholine).
Succinylcholine Process Tubocurarine Phase I Phase II Administration of tubocurarine Additive Antagonistic Augmenteda
Administration of succinylcholine Antagonistic Additive Augmenteda
Effect of neostigmine Antagonistic Augmenteda
Antagonistic Initial excitatory effect on skeletal muscle None Fasciculations None Response to tetanic stimulus Unsustained (“fade”) Sustainedb
Unsustained Post-tetanic facilitation Yes No Yes
aIt is not known whether this interaction is additive or synergistic (superadditive).
bThe amplitude is decreased, but the response is sustained.
Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 9th ed. McGraw-Hill, 2007.
Depolarizing Neuromuscular Blocking Drugs
Pharmacokinetics
Succinylcholine is composed of 2 ACh molecules linked end to end. Succinylcholine is metabolized by cholinesterase (butyrylcholinesterase or pseudocholinesterase) in the liver and plasma. It has a duration of action of only a few minutes if given as a single dose. Blockade may be prolonged in patients with genetic variants of plasma cholinesterase that metabolize succinylcholine very slowly. Such variant cholinesterases are resistant to the inhibitory action of dibucaine. Succinylcholine is not rapidly hydrolyzed by acetylcholinesterase.
Mechanism of Action
Succinylcholine acts like a nicotinic agonist and depolarizes the neuromuscular end plate (Figure 27-1).
The initial depolarization is often accompanied by twitching and fasciculations (prevented by pretreatment with small doses of a nondepolarizing blocker). Because tension cannot be maintained in skeletal muscle without periodic repolarization and depolarization of the end plate, continuous depolarization results in muscle relaxation and paralysis. Succinylcholine may also plug the end plate channels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree