Short Bowel Syndrome1
Khursheed N. Jeejeebhoy
1Abbreviations: CI, confidence interval; DFD, defined formula diet; EGF, epidermal growth factor; GH, growth hormone; GLP, glucagonlike peptide; HEN, home enteral nutrition; HGH, human growth hormone; HPN, home parenteral nutrition; IGF-I, insulinlike growth factor-I; IT, intestinal transplantation; ORS, oral rehydration solution; PN, parenteral nutrition; SCFA, short-chain fatty acid; TGF-α, transforming growth factor-α.
DEFINITION
A consensus paper (1) provided the following definitions: Short-bowel syndrome results from surgical resection, congenital defect, or disease-associated loss of absorption and is characterized by the inability to maintain protein-energy, fluid, electrolyte, or micronutrient balances when on a conventionally accepted, normal diet. Intestinal failure results from obstruction, dysmotility, surgical resection, congenital defect, or disease-associated loss of absorption and is characterized by the inability to maintain protein-energy, fluid, electrolyte, or micronutrient balance. The major difference between intestinal failure and short bowel is that intestinal failure is the result of a variety of conditions such as chronic intestinal obstruction, whereas short bowel implies a reduction of functional intestinal surface area for absorption.
ETIOLOGY
The principal causes of short bowel syndrome are outlined in Table 77.1. The two major causes of surgical short bowel are inflammatory bowel disease and vascular disease. The risk factors for vascular disease leading to resection of the intestine are the same as those for other vascular diseases: increasing age, smoking, cardiac disease leading to low output or predisposing to embolization, hypercoagulable states, diabetes, and vasculitis.
TABLE 77.1 CAUSES OF SHORT BOWEL SYNDROME | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||
PATHOPHYSIOLOGIC CONSIDERATIONS
To understand and treat this condition, it is necessary to understand normal function and how it is altered by the short bowel syndrome.
Gastric Emptying
The rate at which a meal enters the intestine is regulated by the rate of gastric emptying. Gastric emptying of liquids depends on their osmolarity. For digestible solids, the emptying is regulated by the particle size. However, intestinal contents entering the distal intestine inhibit gastric emptying (2). Gastric hypersecretion occurs after significant small bowel resection and reduces nutrient absorption by inactivating pancreatic enzymes.
Small Bowel
Small bowel motility is three times slower in the ileum than in the jejunum (3). In addition, the ileocecal valve may slow transit, especially when the ileum has been resected (4).
The adult small bowel receives about 5 to 6 L of endogenous secretions and 2 to 3 L of exogenous fluids per day. It reabsorbs most of this volume in the small bowel. The amount reabsorbed in the small intestine depends on the nature of the meal (5). With a meat- and salad-based meal, most of the fluid is absorbed in the jejunum, whereas with a milk and doughnut meal, less is absorbed proximally and more distally. In addition, the absorptive processes are different in the jejunum as compared with the ileum. These differences depend partly on the nature of the electrolyte transport processes and partly on the permeability of the intercellular junctions. In general, water absorption is a passive process resulting from the active transport of nutrients and electrolytes. The transport of sodium creates an electrochemical gradient and also drives the uptake of carbohydrates and amino acids across the intestinal mucosa. In addition, the ileum has neutral sodium chloride absorption. However, the net absorption depends not only on these processes but also on the extent of back diffusion of the transported material into the intestinal lumen through leaky intercellular junctions. In the jejunum, these junctions are very leaky, and thus jejunal contents are always isotonic.
Fluid absorption in this region of the bowel is very inefficient when compared with the ileum. It has been estimated that the efficiency of water absorption is 44% and 70% of the ingested load in the jejunum and ileum, respectively. For sodium, the corresponding estimates are 13% and 72% (5). Hence, the ileum is important in the conservation of fluid and electrolytes.
Unique Functions of the Ileum
The terminal ileum uniquely absorbs vitamin B12 and bile salts. Bile salts are essential for the efficient absorption of fats and fat-soluble vitamins. Normally, the demand for bile salts imposed by fat absorption cannot be met by synthesis alone. This full need is met only by ileal resorption of bile salts, which are then recycled into the intestine. With ileal resection, the loss of bile salts increases and is not met by an increase in synthesis. The bile salt pool is depleted, and fat absorption is reduced. In addition, loss of bile salts into the colon affects the colonocytes and reduces the ability of the colon to reabsorb salt and water. The result is increased diarrhea. In the colon, bile salts are also dehydroxylated to deoxy bile salts that induce colonic water secretion.
Colon
The colon has the slowest transit, varying between 24 and 150 hours. The intercellular junctions are the tightest in this part of the bowel, and the efficiency of water and salt absorption in the colon exceeds 90% (6). In addition, carbohydrate is fermented in the colon to short-chain fatty acids (SCFAs) having two important actions. First SCFAs enhance salt and water absorption (7). Second, the energy content of malabsorbed carbohydrates is salvaged by being absorbed as SCFAs. Data suggest that in patients with short bowel syndrome, this salvage may be greater than in physiologically normal persons (8). Thus, the colon becomes an important organ for fluid and electrolyte conservation and for the salvage of malabsorbed energy substrates in patients with a short bowel.
EFFECTS OF INTESTINAL RESECTION
Motility
Gastric motility is enhanced following small bowel resection (9). Whereas proximal resection does not increase the rate of intestinal transit, ileal resection significantly
accelerates intestinal transit (9, 10). In this situation, the colon aids in slowing intestinal transit so that in patients with a short bowel without a colon, a marker fed by mouth was completely excreted in a few hours (11).
accelerates intestinal transit (9, 10). In this situation, the colon aids in slowing intestinal transit so that in patients with a short bowel without a colon, a marker fed by mouth was completely excreted in a few hours (11).
Absorption of Fluid and Electrolytes
The effect of intestinal resection depends on the extent and site of resection. Proximal resection results in no bowel disturbance because the ileum and colon absorb the increased fluid and electrolyte load efficiently. The remaining ileum continues to absorb bile salts, and thus there is little reaching the colon to impede salt and water resorption. In contrast, when the ileum is resected, the colon receives a much larger load of fluid and electrolytes and also receives bile salts that reduce its ability to absorb salt and water, with resulting diarrhea. In addition, if the colon is resected, the ability to maintain fluid and electrolyte homeostasis is severely impaired (12).
Absorption of Nutrients
Absorption of nutrients occurs throughout the small bowel, and the removal of the jejunum alone causes the ileum to take over most of the lost function. In this situation, no significant malabsorption occurs (13). In contrast, even a loss of a 100 cm of ileum causes steatorrhea (14). The degree of malabsorption increases with the length of small bowel resection, and the variety of nutrients malabsorbed increases (15, 16). Balance studies of energy absorption showed that the absorption of fat and carbohydrate was equally reduced to between 50% and 75% of intake (17). However, nitrogen absorption was reduced to a lesser extent, namely, to 81% of intake (17). In the study of Ladefoged et al (16), the degrees of calcium, magnesium, zinc, and phosphorus absorption were reduced but did not correlate with the remaining length of bowel; and it was recommended that parenteral nutrition (PN) be mandatory in these patients. Other studies showed similar reduction in absorption, but only half the patients required parenteral replacement.
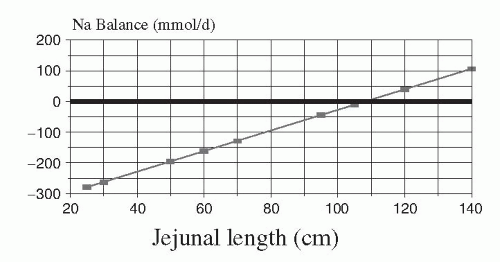
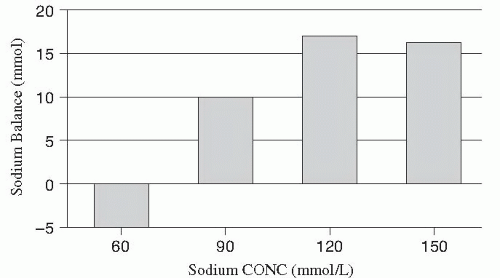
Data recalculated from Nightingale et al (18) in patients with a jejunostomy indicate that fluid balance can be maintained by the oral route if the remaining small bowel exceeds 110 cm (Fig. 77.1), but nutrient balance can be maintained even if the remaining bowel is as short as 60 cm (Fig. 77.2). The data taken as a whole suggest that it is easier to meet needs for energy and nitrogen by increasing oral intake than the needs for electrolytes and divalent ions. A review of the literature before the availability of PN showed that small bowel resections of up to 33% result in no malnutrition, and resections of up to 50% of normal length can be tolerated without special aids; however, patients with small bowel resection in excess of 75% of normal length require nutritional support to avoid severe malnutrition (19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29).
ADAPTATION OF THE INTESTINE
Following resection, the remaining small bowel hypertrophies and increases in absorptive function (30, 31, 32, 33). This process enhances the ability of the remaining bowel to recover the lost function and is thus an important compensatory process. The factors that influence this adaptation are complex and are discussed later, as are the effects of total PN.
Eating exposes the gastrointestinal tract to a unique set of stimuli that do not occur when the bowel is kept constantly empty, a process called bowel rest. The advent of PN resulted in the ability to rest the bowel for short or long periods of time without causing malnutrition, a situation that had not been possible previously. This process nourished the body but excluded the gut from nutrient and hormonal stimuli that occur during the ingestion of an oral diet. The advent of defined formula diets (DFDs) without residue and diets composed of monomers such as glucose instead of polymeric starch modified the stimuli received by the gut when exposed to a normal diet. Because nutrients are absorbed progressively along the length of the bowel, the jejunum is exposed to a higher concentration of nutrients than the ileum. Resection of the proximal bowel causes the ileum to receive more nutrients. Resection of the ileum, conversely, does not alter the jejunal nutrient load but may reduce stimuli from hormones released by the ileum.
Hormonal Response of the Ileum and Colon
A major advance in the understanding of intestinal adaptation has evolved with studies of the role of intestinotrophic hormones. These include growth hormone (GH) (34), insulinlike growth factor-I (IGF-I) (35), epidermal growth factor (EGF) (36), transforming growth factor-α (TGF-α) (37), and glucagon-like peptide-2 (GLP-2) (38). In mice, Drucker et al (39) showed that GLP-2 modified to reduce degradation by dipeptidyl peptidase was the most potent intestinotrophic factor. Jeppesen et al (40) showed that in normal individuals, GLP-2 levels in blood rose with a meal. In contrast, there was an absence of such a response in patients with combined ileal and colonic resection. In contrast, patients who had an ileal resection but retained colon had elevated fasting and meal-induced GLP-2 levels (41). These studies show that ileocolonic resection markedly reduces the likelihood of intestinal adaptation and causes patients with a jejunostomy to continue to have severe malabsorption. In contrast, preservation of the colon allows the remaining jejunum to adapt and helps to explain why patients with a remaining colon can often avoid permanent PN. Finally, isolated jejunal resection leaves the hormonal machinery of the ileum and colon intact.
Effect of Excluding Food from the Bowel Lumen
When food is excluded from the lumen, intestinal hypoplasia occurs in experimental animals. At the same time, body composition can be simultaneously maintained by the use of PN. These facts have been extensively documented, and the interested reader is referred to a review by Tappenden (42).
In growing or neonatal animals, PN and bowel rest maintained normal body growth but resulted in reduced bowel length and gastric and pancreatic hypoplasia (43, 44, 45, 46). Despite the occurrence of mucosal hypoplasia, the development of disaccharidase enzymes and glucose transport was accelerated, and mucosal levels of these enzymes increased in neonatal animals receiving PN (44, 46). Hypoplasia occurred mainly in the proximal small bowel and was less evident distally (45). In adult animals, the effect of PN and bowel rest diminished mucosal mass but stimulated glucose absorption per milligram of mucosal protein (47). In addition, PN and bowel rest increased intestinal permeability (48) and altered the response to endotoxin (49).
Does the Nature of Enteral Nutrition Cause Hypoplasia?
Factors Influencing Bowel Atrophy
In general, it appears that the decreased digestive and absorptive activities of the mucosa during bowel rest are the major reasons for hypoplasia. This concept is supported by the finding that simply increasing the tonicity of the bowel contents results in an increase of the mucosal mass (51). Absorption of amino acids leads to a nonspecific increase of mucosal function and mass (52). Finally, disaccharide hydrolysis followed by absorption stimulates mucosal growth to a greater extent than equivalent monosaccharide absorption (53).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree