DRUG CLASSES
Barbiturates
Nonbarbiturates
• Benzodiazepines
• Nonbenzodiazepines
Sedatives and hypnotics are primarily used to treat insomnia. According to the National Sleep Foundation, insomnia affects nearly 70 million people in the United States. It may be caused by lifestyle changes, such as a new job, moving to a new town, or returning to school; jet lag; chronic pain; headaches; stress; or anxiety. Display 21.1 lists the criteria used to define insomnia.
In many cases insomnia is treated in the outpatient setting. Yet, one of the most frequent patient problems during hospitalization is insomnia. Patients are in unfamiliar surroundings that are unlike the home situation. Noises and lights at night often interfere with or interrupt sleep, as noted in Figure 21.1. An important part of meeting patient needs during illness is to help the patient gain rest and sleep. Sleep deprivation may interfere with the healing process; therefore, a hypnotic may be given. Also, these drugs may be prescribed for short-term use to promote sleep after discharge as a patient transitions to the home environment.
A hypnotic is a drug that induces drowsiness or sleep, meaning it allows the patient to fall asleep and stay asleep. Hypnotics are given at night or bedtime. A sedative is a drug that produces a relaxing, calming effect. Sedatives are usually given during daytime hours, and although they may make the patient drowsy, they usually do not produce sleep.
Sedatives and hypnotics are divided into two classes: barbiturates and nonbarbiturates. The nonbarbiturates are classified into two groups: benzodiazepines and nonbenzodiazepines. Barbiturates were once the drugs of choice to treat insomnia and anxiety; however, the side effects proved to be too harsh. Currently, barbiturates may be used in cases where a deep, nonwaking sleep is desired, such as the few states where assisted suicide is legal. The nonbarbiturates are now used as sedatives in place of barbiturates, because they are more effective in treating insomnia and the adverse reactions are less than the barbiturates. Some of the benzodiazepines are also used as antianxiety drugs (see Chapter 20). The benzodiazepines used primarily for sedation rather than anxiety are discussed in this chapter and include temazepam (Restoril) and triazolam (Halcion).
PHARMACOLOGY IN PRACTICE

Mr. Phillip’s wife died in an automobile accident, and he has had trouble coping with the loss. He complains about sleeping difficulties, he wakes frequently through the night. The primary health care provider prescribes a hypnotic, 1 capsule per night for use during the next 3 weeks. Read in this chapter about the sedative and hypnotic drugs, and then see if this recommendation helped Mr. Phillip.
Display 21.1 Criteria for the Diagnosis of Insomnia
One or more of the following symptoms must occur
• Difficulty falling asleep
• Waking often and trouble going back to sleep at night
• Waking too early in the morning
• Feeling tired upon waking
The nonbenzodiazepines are a group of unrelated drugs. Examples include eszopiclone (Lunesta) and zolpidem (Ambien). Barbiturates, benzodiazepines, and nonbenzodiazepines are listed in the Summary Drug Table: Sedatives and Hypnotics.
Actions
Barbiturates
All barbiturates have essentially the same mode of action. These drugs are capable of producing central nervous system (CNS) depression and mood alterations ranging from mild excitation to mild sedation, hypnosis (sleep), and deep coma. These drugs also are respiratory depressants; the degree of depression usually depends on the dose taken.
Benzodiazepines and Nonbenzodiazepines
Nonbarbiturate sedatives and hypnotics have essentially the same mode of action as the barbiturates—that is, they depress the CNS. The benzodiazepine effect on gamma (γ)-aminobutyric acid (GABA) to potentiate neural inhibition is discussed in Chapter 20. However, these drugs have a lesser effect on the respiratory rate—another reason they are chosen over barbiturates for insomnia.

Figure 21.1 Noises and lights in the environment may cause insomnia for the hospitalized patient.
The nonbenzodiazepine effects diminish after approximately 2 weeks. Persons taking these drugs for longer than 2 weeks may have a tendency to increase the dose to produce the desired effects (e.g., sleep, sedation). Physical tolerance and psychological dependence may occur, especially after prolonged use of high doses. However, their addictive potential appears to be less than that of the barbiturates. Discontinuing use of a sedative or hypnotic after prolonged use may result in mild to severe withdrawal symptoms.
Uses
The sedative and hypnotic drugs are used in the treatment of:
• Insomnia
• Convulsions or seizures
They are also used as adjuncts for anesthesia and for:
• Preoperative sedation
• Conscious sedation
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older adult patients may require a smaller hypnotic dose, and in some instances, a sedative dose may act like a hypnotic and produce sleep.
Adverse Reactions
• Nervous system reactions include dizziness, drowsiness, and headache.
• A common gastrointestinal reaction is nausea.
Contraindications
These drugs are contraindicated in patients with known hypersensitivity to sedatives or hypnotics. Do not administer these drugs to comatose patients, those with severe respiratory problems, those with a history of drug and alcohol habitual use, or pregnant or lactating women. Due to a specific enzyme reaction, grapefruit or its juice should not be taken if the patient is on triazolam or zaleplon. The barbiturates are classified as pregnancy category D drugs.
Benzodiazepines (e.g., estazolam, quazepam, temazepam, triazolam) used for sedation are classified as pregnancy category X drugs. Most nonbenzodiazepines are pregnancy category B or C drugs.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Childbearing Women
Women taking benzodiazepines should be warned of the potential risk to the fetus so that contraceptive methods may be instituted, if necessary. A child born to a mother taking benzodiazepines may experience withdrawal symptoms during the postnatal period.
Precautions
Sedatives and hypnotics should be used cautiously in lactating patients and in patients with hepatic or renal impairment, habitual alcohol use, and mental health problems.
Interactions
The following interactions may occur when a sedative or hypnotic is administered with another agent:
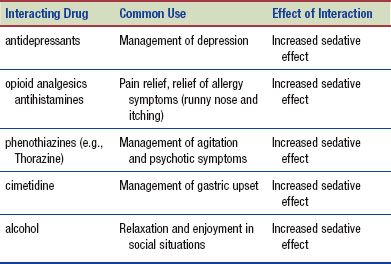
Over-the-counter (OTC) sleep aids are abundant, and patients may not volunteer information regarding their use of these alternative or complementary remedies. Always inquire about use of herbal or OTC products. Although lab testing is not conclusive, medical reports indicate a possible interaction with eucalyptus products causing increased sedation.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Melatonin is a hormone produced by the pineal gland in the brain. Melatonin has been used in treating insomnia, overcoming jet lag, and improving the effectiveness of the immune system, and as an antioxidant. The most significant use—at low doses—is the short-term treatment of insomnia. Melatonin obtained from animal pineal tissue is not recommended for use because of the risk of contamination. The synthetic form of melatonin does not carry this risk. Supplements should be purchased from a reliable source to minimize the risk of contamination. Drowsiness may occur within 30 minutes after taking the supplement. The drowsiness may persist for an hour or more, affecting any activity that requires mental alertness, such as driving. Possible adverse reactions include headache and depression. Although uncommon, allergic reactions (difficulty breathing, hives, or swelling of the lips, tongue, or face) to melatonin have been reported (DerMarderosian, 2003).
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
Before administering a sedative or hypnotic, document the patient’s blood pressure, pulse, and respiratory rate. Changes in vital signs (especially hypotension) may occur after drug administration, so having baseline values is important for comparison. In addition to the vital signs, assess the patient’s status by asking the following questions:
Hypnotic Drug Administration (for Sleep Disturbances)
 Is the patient uncomfortable? If the reason for discomfort is pain, an analgesic, rather than a hypnotic, may be required. A hypnotic may not be necessary because an analgesic can also induce drowsiness and sleep.
Is the patient uncomfortable? If the reason for discomfort is pain, an analgesic, rather than a hypnotic, may be required. A hypnotic may not be necessary because an analgesic can also induce drowsiness and sleep.
 When is the drug scheduled for administration? Is it too early for the patient to receive the drug—will they awaken early in the morning?
When is the drug scheduled for administration? Is it too early for the patient to receive the drug—will they awaken early in the morning?
 Are there disturbances in the environment that may keep the patient awake and decrease the effectiveness of the drug?
Are there disturbances in the environment that may keep the patient awake and decrease the effectiveness of the drug?
Sedative Drug Administration (for Relaxing and Calming)
 Is the sedative for a surgical procedure, and is its administration correctly timed?
Is the sedative for a surgical procedure, and is its administration correctly timed?
 Has a consent form for the procedure been signed before the medication is given? Informed consent cannot be established if the patient has medication in his or her system.
Has a consent form for the procedure been signed before the medication is given? Informed consent cannot be established if the patient has medication in his or her system.
If the patient is receiving one of these drugs for daytime sedation, assess the patient’s general mental state and level of consciousness. If the patient appears sedated and difficult to awaken, you should withhold the drug and contact the primary health care provider as soon as possible.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Valerian was originally used in Europe and was brought to North America on the Mayflower (Fig. 21.2). The herb is widely used for its sedative effects in conditions of mild anxiety or restlessness. It is particularly useful in individuals with insomnia. Valerian improves overall sleep quality by shortening the length of time it takes to fall asleep and decreasing the number of nighttime awakenings.
Formulated as a tea, tablet, capsule, or tincture, valerian is classified as “generally recognized as safe” (GRAS) for use in the United States. When used as an aid to sleep, valerian is taken approximately 1 hour before bedtime; less is used for anxiety. Valerian can be used in combination with other calming herbs, such as lemon balm or chamomile. It may take 2 to 4 weeks before the full therapeutic effect (i.e., improvement of mood and sleep patterns) occurs. Individuals have been known to experience withdrawal symptoms when they stop taking valerian abruptly (DerMarderosian, 2003).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


