Patient Story
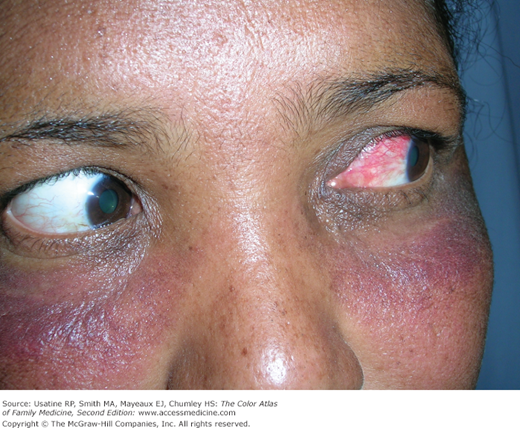
A 45-year-old woman presents with 1 day of increasing eye pain, eye redness, and difficulty in seeing. On examination there was scleral injection and exquisite globe tenderness (Figure 17-1). Her review of systems is positive for morning stiffness and swelling in both of her hands. The patient was urgently referred to an ophthalmologist who diagnosed her with scleritis. Her visual acuity was reduced minimally. A slit lamp exam revealed injected sclera with a bluish hue in the affected eye and a rare anterior chamber cell. The posterior segment was normal.
The ophthalmologist prescribed an oral NSAID, specifically indomethacin, as it effectively crosses the blood-brain barrier and gets good levels in the eye.
Introduction
Episcleritis and scleritis are inflammation of the deeper layers of the eye, the vascular episclera, and the avascular sclera. Episcleritis presents with segmental eye redness, discomfort but not severe pain, and no vision loss. Scleritis can have overlying episcleritis, but also has a violaceous hue, is painful, and may cause vision loss. Scleritis typically has an associated underlying condition (autoimmune or infectious) that should be identified and treated. Scleritis is treated with NSAIDs, systemic glucocorticoids, or immunosuppressive medications. Patients with scleritis are often referred to an ophthalmologist as vision loss is common.
Epidemiology
- Scleritis usually presents between the ages of 30 and 50 years and is twice as common in women compared to men.1
- Forty-four percent of patients presenting with scleritis to specialty health centers were found to have an associated systematic disease (37% rheumatic, 7% infection), most commonly (15%) rheumatoid arthritis.2
Etiology and Pathophysiology
- Scleritis and episcleritis are inflammatory conditions causing congestion of the deeper 2 of the 3 vascular layers (conjunctival, episcleral, and scleral plexuses) overlying the avascular sclera.
- Scleritis often occurs with episcleritis; episcleritis does not involve the sclera and does not progress to scleritis.
- Scleritis disrupts vascular architecture and may cause vision loss; episcleritis does not.
- Causes of scleritis:
- Systemic autoimmune diseases such as rheumatoid arthritis, Wegener granulomatosis, seronegative spondyloarthropathies, relapsing polychondritis, systemic lupus erythematosus (SLE). Figure 17-2 shows a young woman with SLE and scleritis.
- Infections (Pseudomonas, tuberculosis, syphilis, herpes zoster).
- Less common causes include gout and sarcoidosis.
- Idiopathic.
- Systemic autoimmune diseases such as rheumatoid arthritis, Wegener granulomatosis, seronegative spondyloarthropathies, relapsing polychondritis, systemic lupus erythematosus (SLE). Figure 17-2 shows a young woman with SLE and scleritis.
- Causes of episcleritis
- Most often idiopathic.
- May be associated with any of the conditions listed above, especially if the presentation is nodular or recurrent.
- Most often idiopathic.
Diagnosis
Scleritis
- Segmental or diffuse inflammation of sclera (dark red, purple, or blue color), with overlying episclera and conjunctival inflammation (Figures 17-1, 17-2, and 17-3).
- Severe, boring eye pain often radiating to head and neck that worsens with eye movement. However, 20% of patients may not have pain, including those with the necrotizing type (scleromalacia perforans) and those taking immunosuppressive agents prior to the onset of scleritis.1
- Photophobia and vision loss.