Rosai-Dorfman Disease
L. Jeffrey Medeiros, MD
Roberto N. Miranda, MD
Key Facts
Terminology
Rosai-Dorfman disease (RDD) and sinus histiocytosis with massive lymphadenopathy are equivalent terms
Etiology/Pathogenesis
Unknown; histologic features are suggestive of virus
Clinical Issues
Spontaneous regression occurs in most patients
No specific therapy required
Macroscopic Features
Large, often massive lymph nodes
Often matted with capsular fibrosis
Microscopic Pathology
Lymph nodes show dilated sinuses
Associated small lymphocytes and plasma cells
RDD histiocytes characterized by
Abundant eosinophilic cytoplasm
Central vesicular nucleus
Small but distinct central nucleolus
Emperipolesis
In extranodal sites
Emperipolesis often focal or absent
Ancillary Tests
Immunohistochemistry
S100(±), CD1a(-)
Top Differential Diagnoses
Langerhans cell histiocytosis
Chronic granulomatous inflammation
IgG4-related disease
Metastatic neoplasms to lymph node sinuses
TERMINOLOGY
Abbreviations
Rosai-Dorfman disease (RDD)
Synonyms
Sinus histiocytosis with massive lymphadenopathy (SHML)
Histiocytose lipidique ganglionnaire pseudotumorale de Destombes
Definitions
Benign proliferation of histiocytes with characteristic cytologic features
Histiocytes show emperipolesis (engulfment of lymphocytes)
Histiocytes express S100 protein
ETIOLOGY/PATHOGENESIS
Infectious Agents
Histologic similarities between Salmonella infection and RDD have been observed
No culture evidence or other data to support
Other infectious agents are possible
One study has reported SV40 polyoma virus in subset of cases of soft tissue-based RDD
Genetic
RDD has been reported in identical twins or families, suggesting genetic predisposition
Rare familial forms of RDD have been reported
SLC29A3 mutations have been identified
Faisalabad histiocytosis is genetic syndrome that is similar to RDD
Autoimmune
An autoimmune etiology has been suggested
Subset of RDD patients have coexistent autoimmune disease
Association with autoimmune lymphoproliferative syndrome
Tumor-Associated
RDD, typically focal, can be associated with lymphomas, most commonly
Nodular lymphocyte-predominant Hodgkin lymphoma
Follicular lymphoma
Unknown
Most cases of RDD are of unknown etiology
CLINICAL ISSUES
Epidemiology
Incidence
Rare; worldwide geographic distribution
Age
Wide range
Newborn to ˜ 75 years; more common in children
Gender
M:F = 3:2
Ethnicity
All races affected
Site
Lymph nodes
Extranodal sites in ˜ 20% of patients
Head and neck region common
Upper respiratory tract, skin
Other common sites
Skin, soft tissues, gastrointestinal tract
Bones, breast, dura
Presentation
Lymphadenopathy, often without any symptoms
Usually localized
Cervical lymph nodes most often involved
Often bilateral with massive enlargement
B symptoms are uncommon but can occur
Fever, night sweats can precede lymphadenopathy
Laboratory abnormalities in subset of patients
Polyclonal hypergammaglobulinemia common
Blood lymphocytes with low CD4 to CD8 ratio
Hemolytic anemia
Treatment
In most patients, RDD regresses spontaneously
Usually no specific therapy needed
RDD can persist for months or, rarely, years before regression
Rare subset of patients have aggressive RDD and require therapy
Therapies: Steroids, radiation therapy, chemotherapy
Patients have been reported with rapid response to steroids
Rituximab (anti-CD20) has been used with response in some patients
Surgical excision for patients with obstruction/compression-type symptoms
Prognosis
Excellent for most affected patients
Rare cases can be clinically aggressive
No effective therapy for these rare aggressive cases
Fatalities can occur as a result of
Accompanying immune dysregulation
Mass effect in vital organs
IMAGE FINDINGS
Radiographic Findings
Lymphadenopathy
MACROSCOPIC FEATURES
General Features
Enlarged lymph nodes: Often massive
Often matted with capsular fibrosis
MICROSCOPIC PATHOLOGY
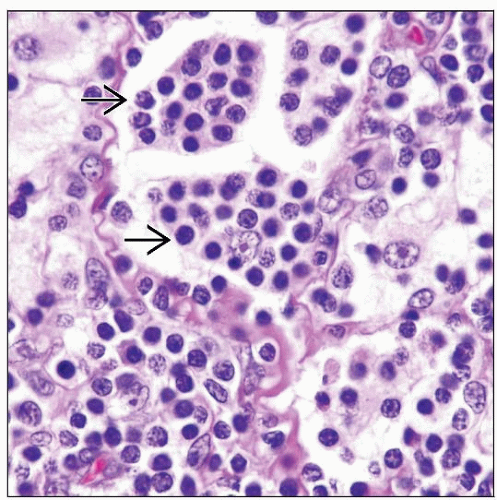
Histologic Features
Lymph nodes
Overall lymph node architecture is intact but distorted
Marked dilatation of sinuses
Filled with RDD histiocytes
Associated with small lymphocytes and plasma cells
Granulocytes not present, unless superimposed necrosis or infection
RDD histiocytes show emperipolesis
Engulf cells that become located in histiocyte cytoplasm
Small lymphocytes, plasma cells, or erythrocytes
Cells surrounded by intracytoplasmic vacuole that appears as a halo
Engulfed cells are usually viable
Often marked plasmacytosis between sinuses
Sclerosis is common (˜ 75% of cases)
Reactive follicles often present
Eosinophils rare or absent; mitoses are uncommon
Rarely, affected lymph nodes can undergo infarct
Extranodal sites
RDD histiocytes can be sparse in areas
Emperipolesis can be absent
Small lymphocytes and plasma cells often numerous
Fibrosis can be prominent
RDD can be associated with Hodgkin or non-Hodgkin lymphomas
RDD is often a small focus in this setting
Incidental finding usually without impact on prognosis
Cytologic Features
RDD histiocytes are characterized by
Large size with abundant eosinophilic cytoplasm
Well-defined cell borders
Central, often round nucleus
Distinct central nucleolus
Emperipolesis ±/-, with small lymphocytes in histiocyte cytoplasm
Halos around lymphocytes not seen in cytologic preparations
Halos are result of fixation artifact in routine histologic sections
Associated with many inflammatory cells
Early lesions: Many small lymphocytes and immunoblasts
Late lesions: More plasma cells; cytoplasmic globules (± Russell bodies)
Predominant Pattern/Injury Type
Sinusoidal
Predominant Cell/Compartment Type
Histiocyte
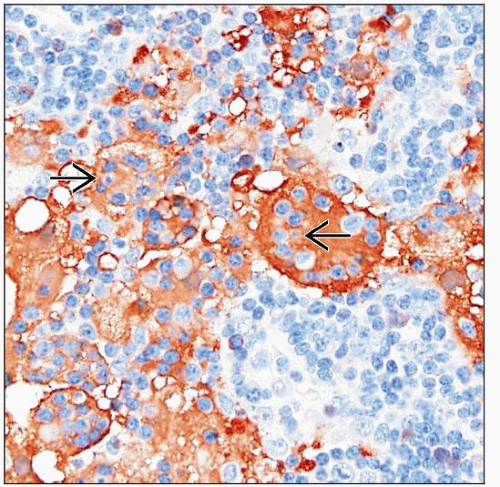
ANCILLARY TESTS
Immunohistochemistry
RDD histiocytes are
S100(±), CD1a(-), langerin/CD207(-)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree