Rheumatoid Arthritis-related Lymphadenopathy
L. Jeffrey Medeiros, MD
Key Facts
Terminology
Lymphadenopathy accompanying rheumatoid arthritis (RA)
Etiology/Pathogenesis
Smoking is risk factor
Infectious agent may act as antigenic trigger of RA
Genetic susceptibility and impaired T-cell function are involved in RA
Clinical Issues
Lymphadenopathy occurs in ˜ 75% of RA patients at some point in their clinical course
Can be localized or systemic
Microscopic Pathology
Marked follicular hyperplasia in cortex and medulla of lymph node
“Starry sky” pattern within germinal centers
Hyaline-like eosinophilic deposits(+/-)
Interfollicular areas show marked plasmacytosis
Capillary endothelial hyperplasia
Ancillary Tests
Immunophenotype
Polytypic B cells and plasma cells; normal T cells
EBER(+) in ˜ 20% of RA-related lymph nodes
No monoclonal Ig or TCR gene rearrangements
Diagnostic Checklist
It is unusual for RA-related lymphadenopathy to be initial manifestation of RA
Clinical history is often available to support diagnosis
Joint symptoms &/or physical manifestations
Laboratory results supporting diagnosis of RA
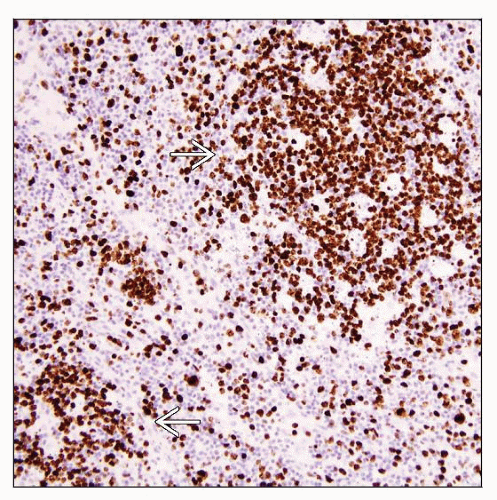
 Lymphadenopathy in an untreated patient with rheumatoid arthritis (RA). A follicle with a hyperplastic germinal center and many tingible body macrophages resulting in a “starry sky” pattern is shown. |
TERMINOLOGY
Definitions
Lymphadenopathy accompanying rheumatoid arthritis (RA)
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Smoking is risk factor
Increases risk of developing RA
Correlates with increased disease severity
Autoimmune Disease
Infectious agent may act as antigenic trigger of RA
Possible/suspected organisms include
Epstein-Barr virus (EBV), Cytomegalovirus (CMV), Parvovirus
Rubella virus, Mycoplasma species
Genetic susceptibility is involved in RA
Association with HLA-DR1 and HLA-DR4
Recently reported loci at chromosomes 10p15, 12q13, and 22q13
T-cell function is impaired in RA
RA is mediated by inflammatory mediators and cytokines released by macrophages and synovial lining cells
Activated by CD4(+) T helper cells
Important cytokines: Tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6
Bone and cartilage destruction mediated by prostaglandins, matrix metalloproteinases, RANKL
CLINICAL ISSUES
Epidemiology
Incidence
RA affects 0.8% of world population
Age
˜ 80% of patients develop RA between 35-50 years
Can affect patients at any age
Gender
Male to female ratio = 1:3-5
Site
Most common sites of lymphadenopathy: Cervical, supraclavicular, axillary
Any lymph node group can be affected
Presentation
RA usually has insidious onset
10% of patients have acute onset with rapid polyarticular involvement
Initial symptoms may be nonspecific and generalized
Fatigue, weakness, anorexia, fever, musculoskeletal pain
Joint involvement often follows generalized symptoms
Small joints in hands and feet are affected before large joints
Typically symmetric
Lymphadenopathy occurs in ˜ 75% of RA patients at some point in their clinical course
Can be localized or systemic
Felty syndrome = RA, splenomegaly, and autoimmune neutropenia
In 1987, American Rheumatism Association proposed criteria to help establish diagnosis of RA
Total of 4 of 7 criteria support diagnosis of RA
Morning stiffness
Arthritis in 3 or more joints
Arthritis of hand joints
Symmetric arthritis
Rheumatoid nodule(s)
Serum rheumatoid factor (RF)(+)
Typical radiographic changes
Laboratory Tests
Rheumatoid factor (RF)
RF = immunoglobulins that react with Fc portion of IgG molecules
Most standard tests detect IgM
˜ 60% of patients with RA have elevated RF in serum
RF can be elevated in other autoimmune diseases
Sjögren syndrome, systemic lupus erythematosus
Serum RF levels can be positive in healthy individuals
˜ 5%; positivity tends to increase with age
Anti-cyclic citrullinated peptide antibodies (anti-CCP)
Positive 80-85% of RA patients; more sensitive than RF
Higher specificity for RA (90-96%) than RF (50-80%)
Natural History
RA is progressive disease that can be crippling in untreated patients
RA-related lymphadenopathy can wax and wane
Treatment
Drugs
Immunomodulator agents
Methotrexate is commonly used
Anti-TNF α and other recently developed biological therapies
Therapies used more commonly in the past
Azathioprine
Gold
Prognosis
Patients with RA have increased risk of malignant lymphoma
Risk is ˜ 2x greater than general population
Increased risk of lymphoma is attributable to RA itself
Highest risk in patients who are serum RF(+)
Can be detected after 5 years of follow-up
Therapy of RA patients also may increase risk of developing lymphoma
Common types of lymphoma that occur in RA patients
Diffuse large B-cell lymphoma (DLBCL) is most common
˜ 60-70% of all lymphomas in RA patients
Classical Hodgkin lymphoma (HL)
Nodular sclerosis or mixed cellularity most often reported
Other lymphoma types reported with some frequency in RA patients
Follicular lymphoma
Mantle cell lymphoma
Marginal zone B-cell lymphomas
Peripheral T-cell lymphoma not otherwise classified
Evidence of EBV present in subset of DLBCL and classical HL of RA patients
˜ 20% of DLBCLs are EBV(+)
IMAGE FINDINGS
Radiographic Findings
Joints show juxtaarticular osteopenia and bone erosion with narrowing of joint spaces
Lymphadenopathy can be detected by various imaging methods
MICROSCOPIC PATHOLOGY
Histologic Features
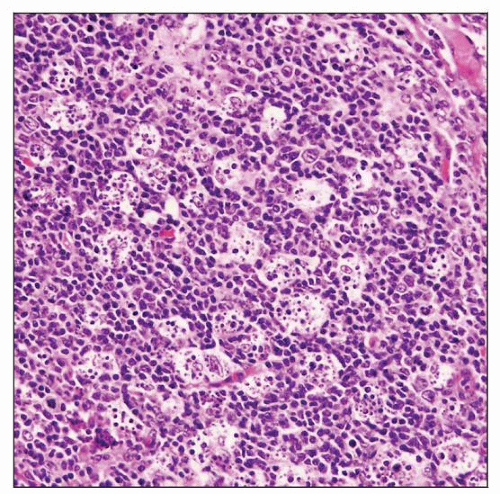
Marked follicular hyperplasia in cortex and medulla of lymph node
Follicles of various sizes and shapes
“Starry sky” pattern within reactive germinal centers
± hyaline-like eosinophilic deposits in germinal centers
Can be extensive and replace lymph node parenchyma
Dystrophic calcification can occur
PAS(+), Congo red(-)
“Cracking artifact” around follicles in poorly fixed tissues
Interfollicular areas
Plasmacytosis is present and often prominent
Small aggregates or sheets of plasma cells without atypia
Cytoplasmic globules of Ig in plasma cells (Russell bodies)
Capillary endothelial hyperplasia
Neutrophils in sinuses and interfollicular areas
± sarcoid-like granulomas
After immunosuppressive therapy lymph nodes often show
Reduced follicular hyperplasia
Expanded interfollicular regions and paracortical hyperplasia
After gold therapy lymph nodes may show
Nonbirefringent crystalline structures throughout parenchyma
Free within spaces or in histiocyte cytoplasm
RA patients can develop lymphoplasmacytic infiltrates of lung
Interstitial or nodular pattern
± reactive germinal centers
Aggregates of small lymphocytes and plasma cells
Can be associated with amyloid
Rheumatoid nodules can occur in lung ± lymphoplasmacytic infiltrate
Cytologic Features
Very few reports in literature of fine needle aspiration findings of RA-related lymphadenopathy
ANCILLARY TESTS
Immunohistochemistry
Follicles
Polytypic surface Ig, pan-B-cell antigens(+)
CD10(+), Bcl-6(+), Bcl-2(-)
CD21 and CD23 expression by follicular dendritic cells (FDCs) in follicles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree