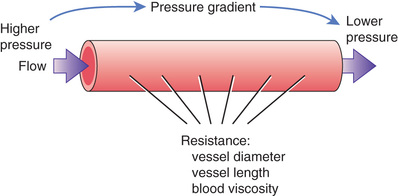
What Makes Blood Flow?
Blood moves within vessels because the force that drives flow is greater than the resistance to flow. As shown in Fig. 34.2, the force that drives blood flow is the pressure gradient between two points in a vessel. Blood will flow from the point where pressure is higher toward the point where pressure is lower. Resistance to flow is determined by the diameter and length of the vessel and by blood viscosity. From a pharmacologic viewpoint, the most important determinant of resistance is vessel diameter: the larger the vessel, the smaller the resistance. Accordingly, when vessels dilate, resistance declines, causing blood flow to increase—and when vessels constrict, resistance rises, causing blood flow to decline. To maintain adequate flow when resistance rises, blood pressure must rise as well.
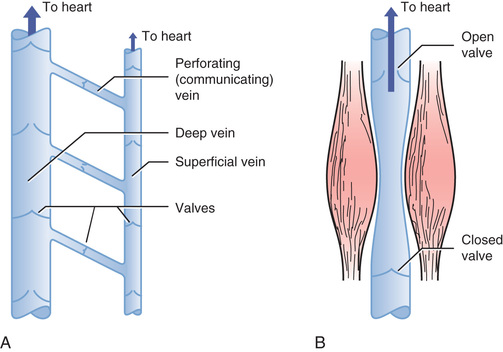
How Does Blood Get Back to the Heart?
As indicated in Fig. 34.3, pressure falls progressively as blood moves through the systemic circulation. Pressure is 120 mm Hg when blood enters the aorta, 30 mm Hg when blood enters capillaries, and only 18 mm Hg when blood leaves capillaries, and then drops to negative values (0 to −5 mm Hg) in the right atrium. (Negative atrial pressure is generated by expansion of the chest during inspiration.)
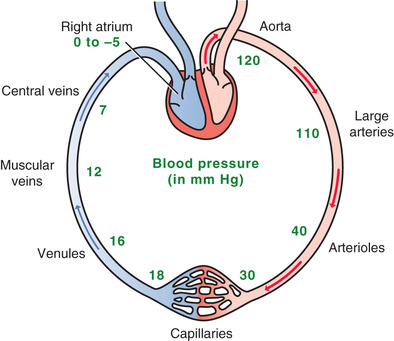
Given that pressure is only 18 mm Hg when blood leaves capillaries, we must ask, “How does blood get back to the heart?” In addition to the small pressure head in venules, three mechanisms help ensure venous return. First, negative pressure in the right atrium helps “suck” blood toward the heart. Second, constriction of smooth muscle in the venous wall increases venous pressure, which helps drive blood toward the heart. Third, and most important, the combination of venous valves and skeletal muscle contraction constitutes an auxiliary “venous pump.” As shown in Fig. 34.4A, the veins are equipped with a system of one-way valves. When skeletal muscles contract (Fig. 34.4B), venous blood is squeezed toward the heart—the only direction the valves will permit.
Regulation of Cardiac Output
In the average adult, cardiac output is about 5 L/minute. Hence, every minute, the heart pumps the equivalent of all the blood in the body. In this section, we consider the major factors that determine how much blood the heart pumps.
Determinants of Cardiac Output
The basic equation for cardiac output is:
CO=HR×SV

where CO is cardiac output, HR is heart rate, and SV is stroke volume. According to the equation, an increase in HR or SV will increase CO, whereas a decrease in HR or SV will decrease CO. For the average person, heart rate is about 70 beats/minute and stroke volume is about 70 mL. Multiplying these, we get 4.9 L/minute—the average value for CO.
Heart Rate
Heart rate is controlled primarily by the autonomic nervous system (ANS). Rate is increased by the sympathetic branch acting through beta1-adrenergic receptors in the sinoatrial (SA) node. Rate is decreased by the parasympathetic branch acting through muscarinic receptors in the SA node. Parasympathetic impulses reach the heart through the vagus nerve.
Stroke Volume
Stroke volume is determined largely by three factors: (1) myocardial contractility, (2) cardiac afterload, and (3) cardiac preload. Myocardial contractility is defined as the force with which the ventricles contract. Contractility is determined primarily by the degree of cardiac dilation, which in turn is determined by the amount of venous return. The importance of venous return in regulating contractility and SV is discussed separately later. In addition to regulation by venous return, contractility can be increased by the sympathetic nervous system, acting through beta1-adrenergic receptors in the myocardium.
Preload
Preload is formally defined as the amount of tension (stretch) applied to a muscle before contraction. In the heart, stretch is determined by ventricular filling pressure, that is, the force of venous return: the greater filling pressure is, the more the ventricles will stretch. Cardiac preload can be expressed as either end-diastolic volume or end-diastolic pressure. As discussed later, an increase in preload will increase SV, whereas a decrease in preload will reduce SV. Frequently, the terms preload and force of venous return are used interchangeably—although they are not truly equivalent.
Afterload
Afterload is formally defined as the load against which a muscle exerts its force (i.e., the load a muscle must overcome in order to contract). For the heart, afterload is the arterial pressure that the left ventricle must overcome to eject blood. Common sense tells us that, if afterload increases, SV will decrease. Conversely, if afterload falls, SV will rise. Cardiac afterload is determined primarily by the degree of peripheral resistance, which in turn is determined by constriction and dilation of arterioles. That is, when arterioles constrict, peripheral resistance rises, causing AP (afterload) to rise as well. Conversely, when arterioles dilate, peripheral resistance falls, causing AP to decline.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree