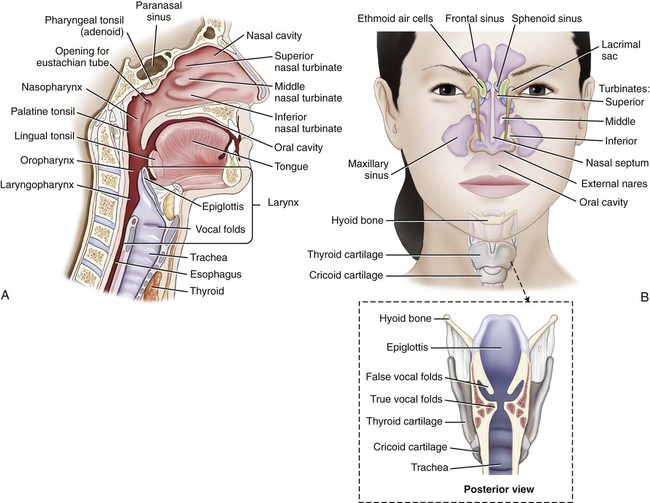
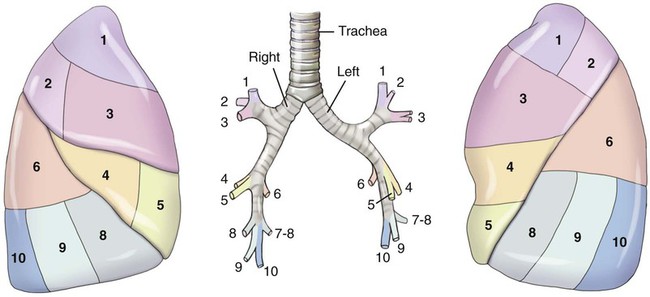
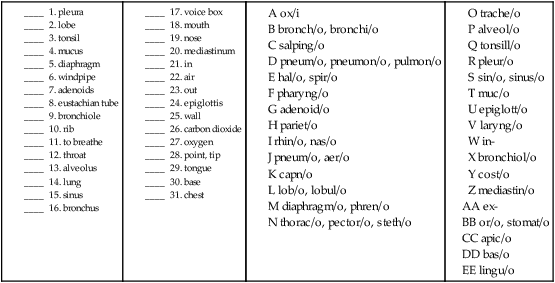
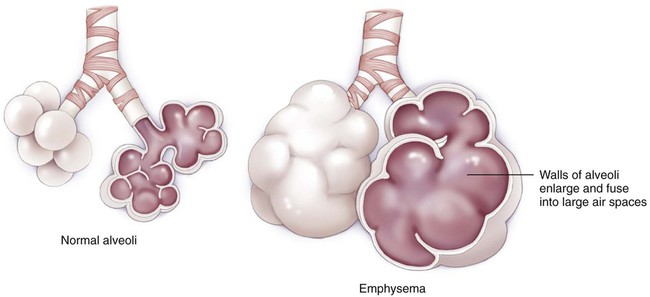
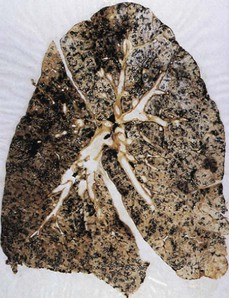
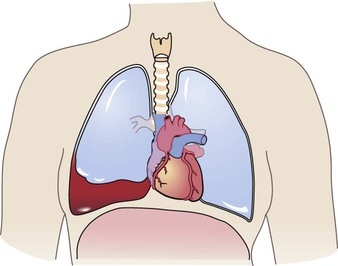
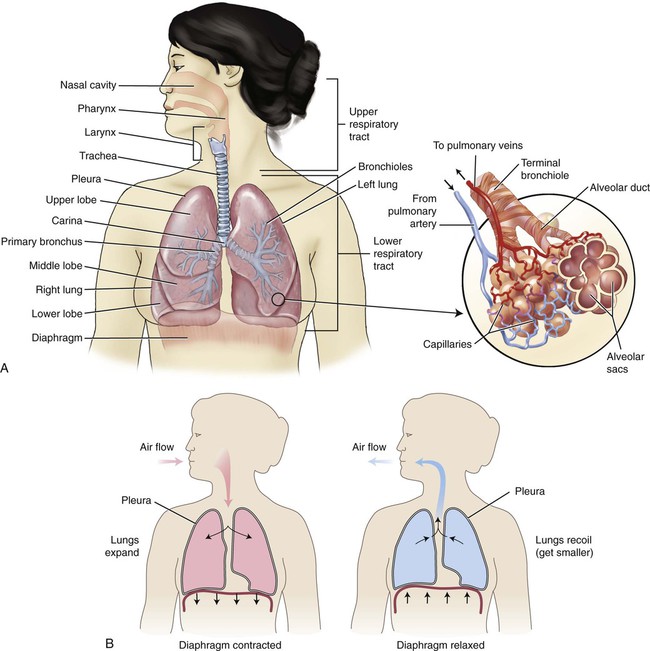
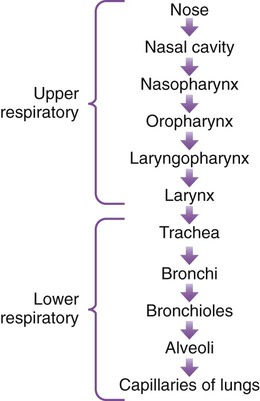
• Delivering oxygen (O2) to the blood for transport to cells in the body. • Excreting the waste product of cellular respiration, carbon dioxide (CO2). • Filtering, cleansing, warming, and humidifying air taken into the lungs. • Regulating the pH of the blood. • Helping the production of sound for speech and singing. • Providing the tissue that receives the stimulus for the sense of smell, olfaction. The respiratory system (Fig. 10-1) partners with the circulatory system to deliver oxygen to and remove carbon dioxide from the cells of the body. Breathing in (inspiration or inhalation) pulls air containing oxygen into the lungs, where it passes into the circulatory system. Carbon dioxide is released when air is pushed out of the lungs (expiration or exhalation). When one dies, one breathes out and no longer breathes in again—hence the expression the patient has “expired.” Using the combining form spir/o, meaning “to breathe,” we can see that respiration means to breathe again (and again). The term ventilation is used to describe the movement of air into the lungs, whether it is a natural or an artificial activity. The respiratory system is anatomically divided into conduction passageways and gas exchange surfaces. The upper respiratory tract (the nose, pharynx, and larynx) and the lower respiratory tract (the trachea, bronchial tree, and lungs) (Fig. 10-1, A) make up the two sections of the conduction passageways. The gas exchange surfaces are the alveoli of the lungs and the cells of the body. There are two main forms of respiration: external respiration and internal respiration. External respiration is the process of exchanging oxygen (O2) and carbon dioxide (CO2) between the lungs and the blood (Fig. 10-1, B). Internal respiration is the exchange of gases between the blood and the cells of the body. A third type of respiration, cellular respiration (also called cellular metabolism), is the use of oxygen to generate energy. The upper respiratory system encompasses the area from the nose to the larynx (Fig. 10-2, A). Air can enter the body through the mouth, but for the most part it enters the body through the two nares (nostrils) of the nose that are separated by the nasal septum. The nasal turbinates (also called nasal conchae) are three scroll-shaped bones (inferior, middle, and superior) that increase the surface area that air must pass over on its way to the lungs (Fig. 10-2, B). The vibrissae (the coarse hairs in the nose) serve to filter out large particulate matter, and the mucous membrane and cilia (small hairs) of the respiratory tract provide a further means of keeping air clean, warm, and moist as it travels to the lungs. The cilia continually move in a wavelike motion to push the sticky mucus and debris out of the respiratory tract. The air then travels up and backward, where it is filtered, warmed, and humidified by the environment in the upper portion of the nasal cavity. Damage to the cilia keeps the germ-laden mucus from leaving the body and consequently provides a hospitable environment for infection. Figure 10-3 illustrates the route of air into the body. The receptors for olfaction are located in the nasal cavity, which is connected to the paranasal sinuses, collectively named for their proximity to the nose. Each lung is composed of sections called lobes, which correspond to the secondary bronchi that supply these areas within each lung. The right lung is made up of three lobes, whereas the left has only two (see Fig. 10-1, A). The abbreviations for the lobes of the lungs are RUL (right upper lobe), RML (right middle lobe), RLL (right lower lobe), LUL (left upper lobe), and LLL (left lower lobe). Within each of these lobes, the secondary bronchi branch out to tertiary bronchi, and the areas that each supplies are referred to as segments (Fig. 10-4). Each segment is supplied with blood from a segmental artery that branches off the pulmonary arteries. The segments are named by their location (e.g., anterior, posterior, apical, basal, medial, or lateral). The lingula is the area where the superior and inferior segments appear on the left lung. Although named for its tongue-like shape, it has been postulated that it may represent the remnants of a left middle lobe. At the end of the segmental bronchi are still smaller branches called bronchioles. These bronchioles end in terminal bronchioles that branch to respiratory bronchioles. The respiratory bronchioles extend into microscopic alveolar ducts capped by air sacs called alveoli (sing. alveolus). Each alveolus is in contact with a blood capillary to provide a means of exchange of gases. At this point O2 is diffused across cell membranes into the blood cells, and CO2 is diffused out to be expired. The muscles responsible for normal, quiet respiration are the dome-shaped diaphragm and the muscles between the ribs (intercostal muscles). On inspiration, the diaphragm is pulled down as it contracts and the intercostal muscles expand, pulling air into the lungs because of the resulting negative pressure (see Fig. 10-1, B). On expiration the diaphragm and intercostal muscles relax, pushing air out of the lungs. Combining Forms for the Anatomy and Physiology of the Respiratory System Prefixes for Anatomy and Physiology of the Respiratory System Terms Related to Symptoms and Signs Involving the Respiratory System (RØØ-R99) Terms Related to Abnormal Breath Sounds (RØ6-RØ9)
Respiratory System
 Recognize and use terms related to the anatomy and physiology of the respiratory system.
Recognize and use terms related to the anatomy and physiology of the respiratory system.
 Recognize and use terms related to the pathology of the respiratory system.
Recognize and use terms related to the pathology of the respiratory system.
 Recognize and use terms related to procedures for the respiratory system.
Recognize and use terms related to procedures for the respiratory system.
ICD-10-PCS Example from Index
Rhinoplasty
Rhinorrhaphy—see Repair, Nose 09QK
Rhinoscopy 09JKXZZ
Functions of the Respiratory System
Anatomy and Physiology
Upper Respiratory Tract
Lower Respiratory Tract
Meaning
Combining Form
adenoid
adenoid/o
air
pneum/o, aer/o
alveolus
alveol/o
base
bas/o
bronchiole
bronchiol/o
bronchus
bronch/o, bronchi/o
carbon dioxide
capn/o
chest
steth/o, thorac/o, pector/o
diaphragm
diaphragm/o, diaphragmat/o, phren/o
epiglottis
epiglott/o
eustachian tube
salping/o
larynx (voicebox)
laryng/o
lobe
lob/o, lobul/o
lung
pulmon/o, pneumon/o, pneum/o
mediastinum
mediastin/o
mouth
or/o, stomat/o
mucus
muc/o
nose
nas/o, rhin/o
oxygen
ox/i, ox/o
pharynx (throat)
pharyng/o
pleura
pleur/o
point, tip, apex
apic/o
rib
cost/o
septum, wall
sept/o, pariet/o
sinus
sinus/o, sin/o
sound
phon/o
to breathe
spir/o, hal/o
tongue
lingu/o
tonsil
tonsill/o
trachea (windpipe)
trache/o
viscera
viscer/o
Prefix
Meaning
ex-
out
in-
in
inter-
between
oxy-
oxygen
para-
near
re-
again
Pathology

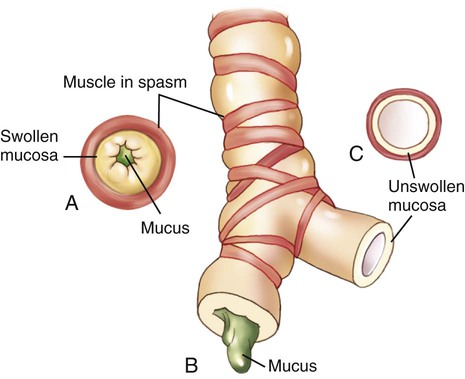
A, Cross section of a bronchiole occluded by muscle spasm, swollen mucosa, and mucus. B, Longitudinal section of an obstructed bronchiole. C, Cross-section of a clear bronchiole.
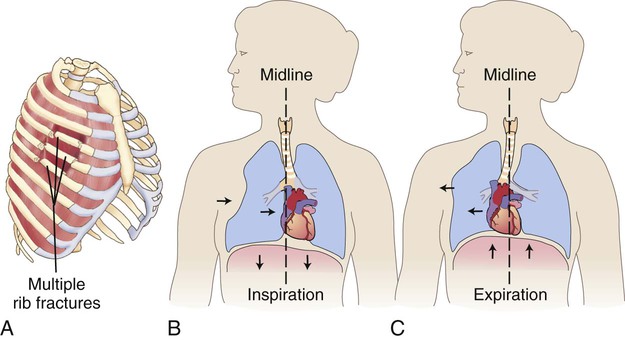
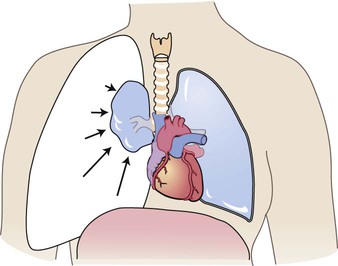
A, Fractured rib sections are unattached to the rest of the chest wall. B, On inspiration, the flail segment of ribs is sucked inward, causing the lung to shift inward. C, On expiration, the flail segment of ribs bellows outward, causing the lung to shift outward. Air moves back and forth between the lungs instead of through the upper airway.
Term
Word Origin
Definition
aphonia
a- no, not, without
phon/o sound
-ia condition
Loss of ability to produce sounds. Dysphonia is difficulty making sounds.
apnea
a- no, not, without
-pnea breathing
Abnormal, periodic cessation of breathing.
bradypnea
brady- slow
-pnea breathing
Abnormally slow breathing.
Cheyne-Stokes respiration
Deep, rapid breathing followed by a period of apnea.
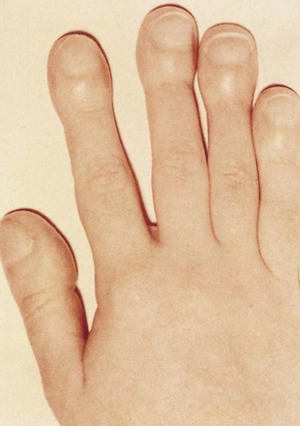
clubbing
Abnormal enlargement of the distal phalanges as a result of diminished O2 in the blood (Fig. 10-5).
cyanosis
cyan/o blue
-osis abnormal condition
Lack of oxygen in blood seen as bluish or grayish discoloration of the skin, nail beds, and/or lips.
dyspnea
dys- difficult
-pnea breathing
Difficult and/or painful breathing. DOE is dyspnea on exertion. Eupnea is good, normal breathing. (Eu- means healthy, normal).
epistaxis
Nosebleed. Also called rhinorrhagia.
hemoptysis
hem/o blood
-ptysis spitting
Coughing up blood or blood-stained sputum.
hypercapnia
hyper- excessive
capn/o carbon dioxide
-ia condition
Condition of excessive CO2 in the blood.
hyperpnea
hyper- excessive
-pnea breathing
Excessively deep breathing. Hypopnea is extremely shallow breathing.
hyperventilation
hyper- excessive
Abnormally increased breathing.
hypoxemia
hypo- deficient
ox/o oxygen
-emia blood condition
Condition of deficient O2 in the blood. Hypoxia is the condition of deficient oxygen in the tissues.
orthopnea
orth/o straight
-pnea breathing
Condition of difficult breathing unless in an upright position (Fig. 10-6).
pleurodynia
pleur/o pleura
-dynia pain
Pain in the chest caused by inflammation of the intercostal muscles.
pyrexia
pyr/o fire
-exia condition
Fever.
shortness of breath (SOB)
Breathlessness; air hunger.
sputum, abnormal
Mucus coughed up from the lungs and expectorated through the mouth. If abnormal, may be described as to its amount, color, or odor.
tachypnea
tachy- fast
-pnea breathing
Rapid, shallow breathing.
thoracodynia
thorac/o chest
-dynia pain
Chest pain.
An important part of the diagnostic process is the evaluation of breath sounds, usually through the use of a stethoscope. This “listening” is termed auscultation, and the “tapping” is called percussion. Normal breath sounds are termed vesicular, misnamed by the inventor of the stethoscope, Laennec. He interpreted the sound as originating from the tiny sacs of the alveoli, instead of the trachea and bronchi, where they actually occur. Abnormal breath sounds are collectively referred to as adventitious sounds.
Term
Word Origin
Definition
friction sounds
Sounds made by dry surfaces rubbing together. Characteristic of inflamed pleurae; may also have a grating or creaking sound.
hiccough
Sound produced by the involuntary contraction of the diaphragm, followed by rapid closure of the glottis. Also called hiccup, singultus.
rales
Also called crackles or crepitations, an abnormal lung sound heard on inspiration, characterized by discontinuous bubbling, clicking, or rattling noises. May be associated with pneumonia or congestive heart failure and are characterized as moist, dry, fine, and/or coarse.
rhonchi
If used as a term without further description (see wheezes), rhonchi are continuous abnormal rumbling sounds heard on expiration, caused by airways blocked with secretions.
stridor
Continuous, high-pitched inspiratory sound from the larynx; a sign of upper airway obstruction or epiglottitis.
wheezing
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access