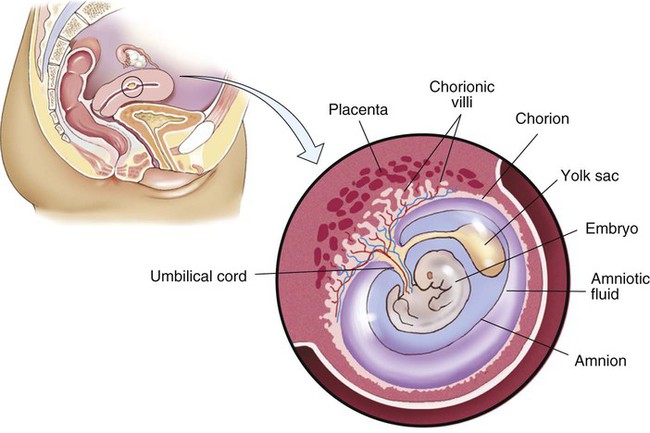
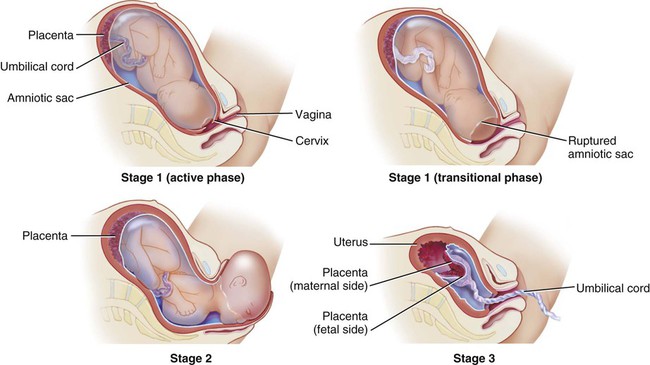
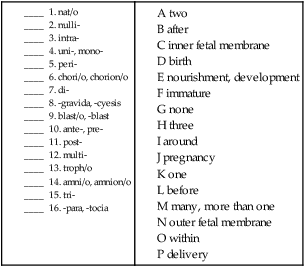
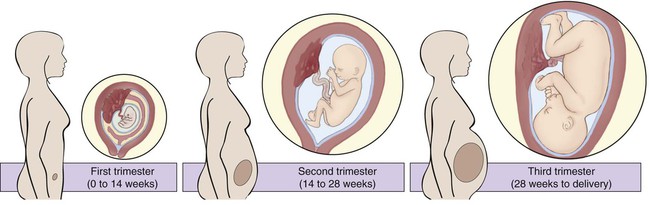
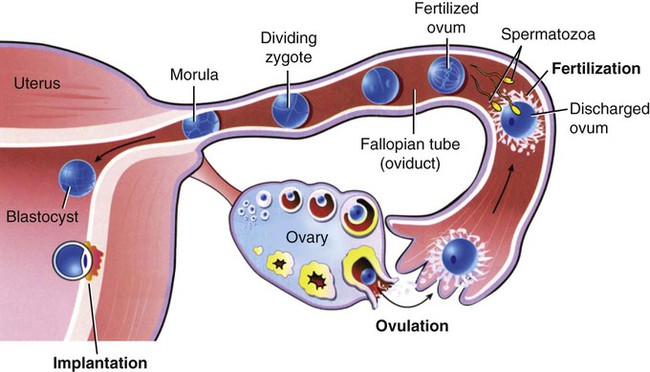
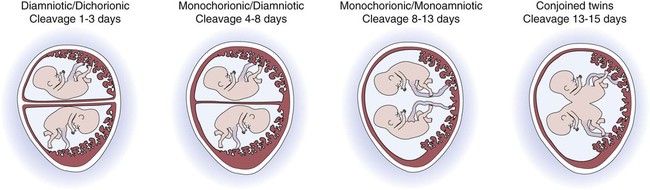
Time periods are important when using the terminology of pregnancy. A normal pregnancy is approximately 38 to 40 weeks, or 9 months. This time period is divided into trimesters, three 3-month segments. Specifically, the first trimester is less than 14 weeks 0 days; the second trimester is 14 weeks 0 days to less than 28 weeks 0 days; and the third trimester is 28 weeks 0 days until delivery (Fig. 7-1). Many ICD-10-CM codes require the addition of information as to the specific trimester of the patient’s pregnancy. The estimated date of delivery (EDD) of the infant can be calculated using a formula, Naegeli’s rule, that uses the first day of a woman’s last menstrual period (LMP), subtracts 3 months, and adds 7 days to come up with a “due” date. Note that this is based on 38 weeks (266 days). Forty weeks (280 days) is the standard time period for a pregnancy. The one-celled fertilized egg, or zygote, carrying the genome (complete set of chromosomal information) divides as it moves through the fallopian tube towards the uterus (Fig. 7-2). In the first few days after fertilization, when the zygote has become a solid ball of cells from repeated divisions, it is called a morula. It is called a morula, which is Latin for mulberry, because of its similar appearance. As it continues to develop, it moves from the fallopian tube into the uterus, and becomes implanted in the uterine wall. At this point, it is identified as a blastocyst. Upon implantation, human chorionic gonadotropin (hCG), the pregnancy hormone, is secreted by the blastocyst. The hCG stimulates the corpus luteum in the ovary to continue to produce progesterone and estrogen. The continued secretion of progesterone maintains the endometrial lining to nourish the growing zygote, while the estrogen contributes to increasing the size of the lining of the uterus and the number of blood vessels that it has. Twins are the result of a modification of this process. In the case of identical (monozygotic) twins, one zygote divides to develop into two genetically identical copies of chromosomes (identical genomes). When two ova are released and fertilized by two different sperm, fraternal (dizygotic) twins develop with two different sets of chromosomes (two genomes), making them not identical, but only as similar as siblings. Although a normal zygote has one set of membranes (an outer chorionic and inner amniotic) to support it through the pregnancy, twins may have a different configuration of sacs depending on when their fertilized eggs divide. If the egg divides 3 to 4 days after it is fertilized, the monozygotic twins will develop in two sets of sacs (dichorionic/diamniotic). If the division happens 3 to 8 days after fertilization, the twins will share the same outer sac (monochorionic) but each will be in its own inner sac (diamniotic). If the split occurs from 8 to 13 days after fertilization, they share the same outer and inner sac (monochorionic/monoamniotic). Finally, if the split happens after 13 days, the twins share the same outer and inner sac (monochorionic/monoamniotic), but the division is incomplete and results in conjoined twins (Fig. 7-3). At the same time that the embryo is developing, extraembryonic membranes are forming to sustain the pregnancy. Two of these, the amnion and the chorion, form the inner and outer sacs that contain the embryo (Fig. 7-4). The outer sac, the chorion, forms part of the placenta, a highly vascular structure that acts as a physical communication between the mother and the embryo. The chorionic villi are small projections that extend from the outer sac to provide a maximum amount of contact with the maternal blood supply. The inner sac, the amnion and its amniotic fluid, cushion the embryo, protect it against temperature changes, and allow it to move. On the outer side, the amniotic sac is connected to the yolk sac, the allantois, and to the placenta by way of the umbilical cord. The yolk sac, attached to the developing embryo, provides a source of nutrition for the early stage of development. The allantois is an embryonic structure that assists in waste removal and gas exchange. It later develops into the placenta and umbilical cord, which share similar functions. The umbilical cord is the tissue that connects the embryo to the placenta (and hence to the mother). When the baby is delivered, the umbilical cord is cut, and the baby is then dependent on his/her own body for all physiological processes. The remaining “scar” is the umbilicus, or navel. Stages of labor: Like the trimesters, labor is also divided into three stages: first, second, and third (Fig. 7-5). The first stage is the longest and, again, includes three parts: an early (or latent) phase, an active phase, and a transitional phase. The early phase, the longest, is marked by dilation of the cervix to approximately 4 centimeters and a changeover from irregular to regular contractions. The active phase has the now regular contractions becoming stronger and closer together. The final phase of the first stage, the transition phase, is the time when the cervix dilates to 10 centimeters and the baby moves down into the birth canal. The second stage is the time when the actual birth takes place and the umbilical cord is cut and clamped. The third stage is the delivery of the placenta. Combining Forms for the Anatomy and Physiology of Pregnancy Prefixes for the Anatomy and Physiology of Pregnancy
Pregnancy, Childbirth, and the Puerperium
 Recognize and use terms related to the anatomy and physiology of pregnancy
Recognize and use terms related to the anatomy and physiology of pregnancy
 Recognize and use terms related to the pathology of pregnancy
Recognize and use terms related to the pathology of pregnancy
 Recognize and use terms related to the procedures for pregnancy
Recognize and use terms related to the procedures for pregnancy
Anatomy and Physiology of Pregnancy
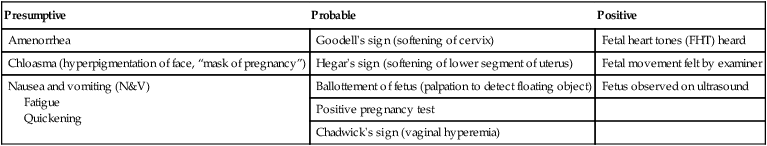
Presumptive
Probable
Positive
Amenorrhea
Goodell’s sign (softening of cervix)
Fetal heart tones (FHT) heard
Chloasma (hyperpigmentation of face, “mask of pregnancy”)
Hegar’s sign (softening of lower segment of uterus)
Fetal movement felt by examiner
Nausea and vomiting (N&V)
Fatigue
Quickening
Ballottement of fetus (palpation to detect floating object)
Fetus observed on ultrasound
Positive pregnancy test
Chadwick’s sign (vaginal hyperemia)
Meaning
Combining Form
amnion, inner fetal sac
amni/o, amnion/o
birth
nat/o
chorion, outer fetal sac
chorion/o, chori/o
development, nourishment
troph/o
embryonic, immature
blast/o
parturition, delivery
part/o
placenta
placent/o
pregnancy
gravid/o
umbilicus
umbilic/o, omphal/o
Prefix
Meaning
ante-
before
di-
two
intra-
within
mono-
one
multi-
many
neo-
new
nulli-
none
peri-
around
post-
after
pre-
before
primi-
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

 pounds and is 18 inches long. At this time, the pregnancy is considered to be at term. ICD-10 classifies late pregnancies as post-term pregnancy (from 40 to 42 completed weeks) and prolonged pregnancy (over 42 weeks).
pounds and is 18 inches long. At this time, the pregnancy is considered to be at term. ICD-10 classifies late pregnancies as post-term pregnancy (from 40 to 42 completed weeks) and prolonged pregnancy (over 42 weeks).