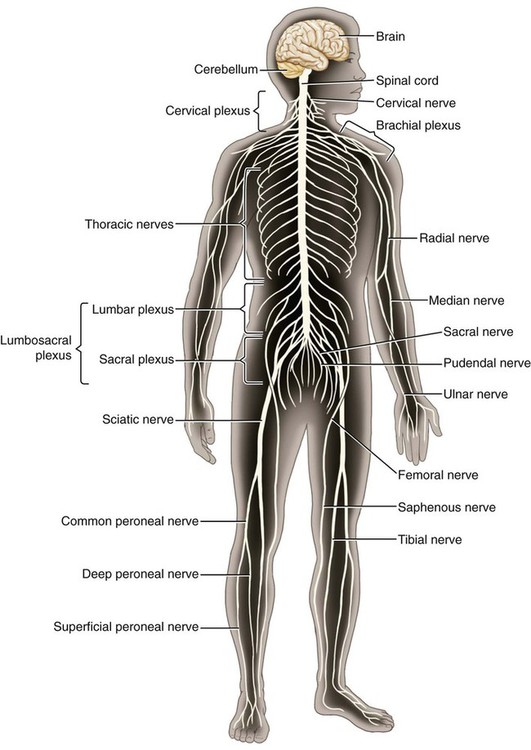
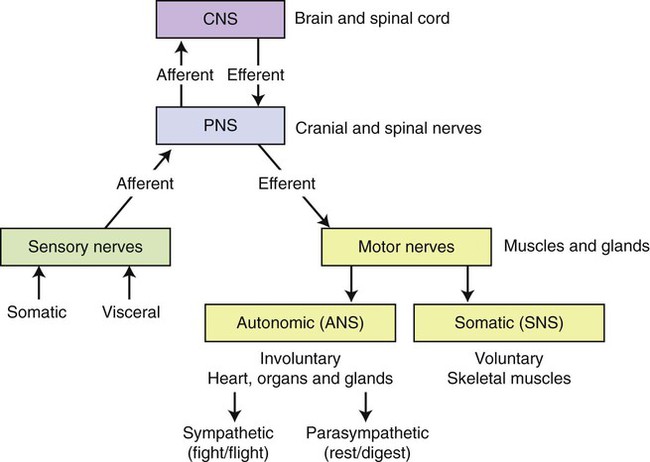
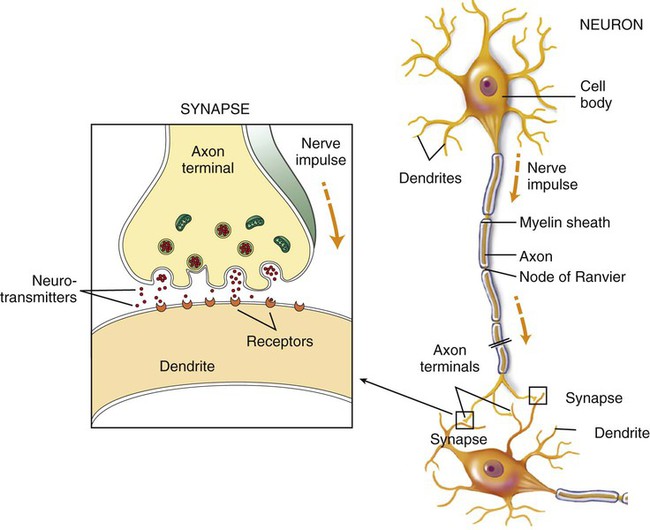
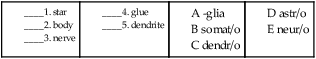
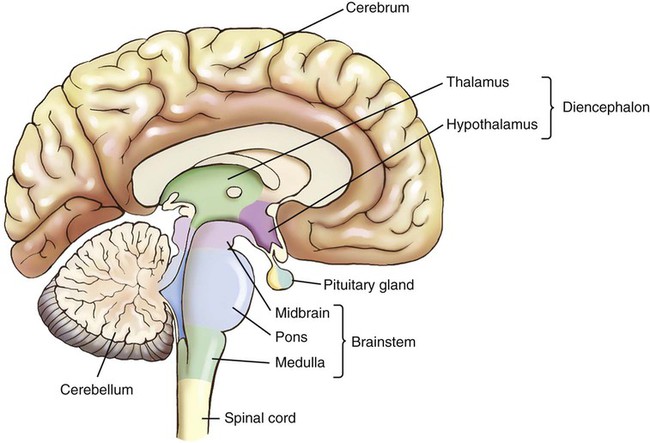
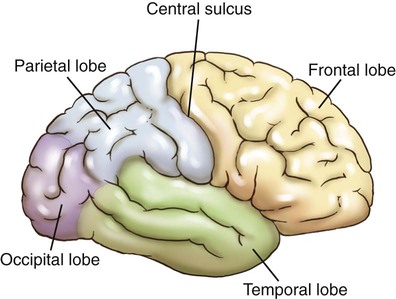
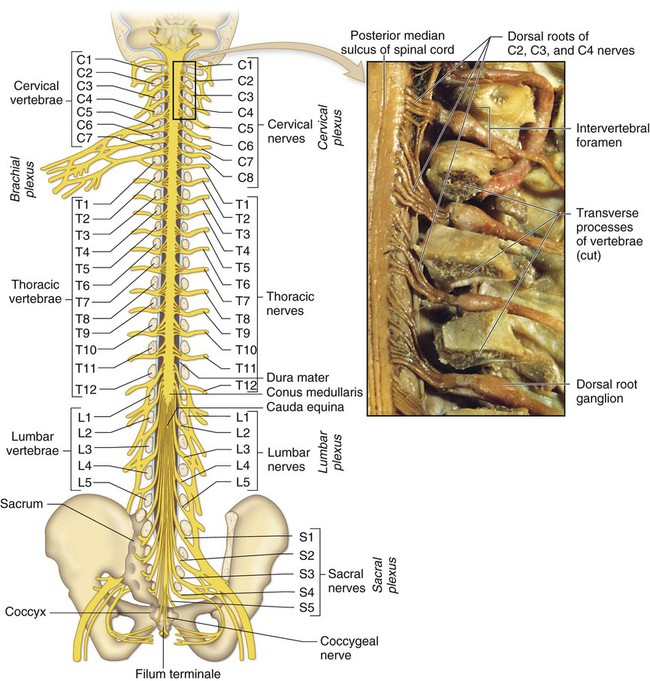
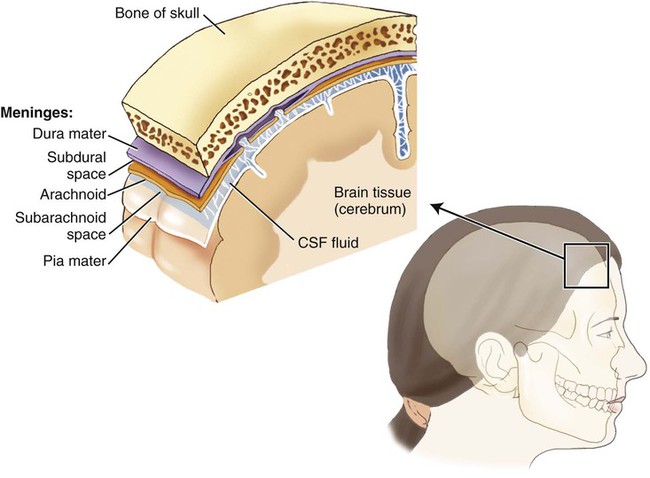
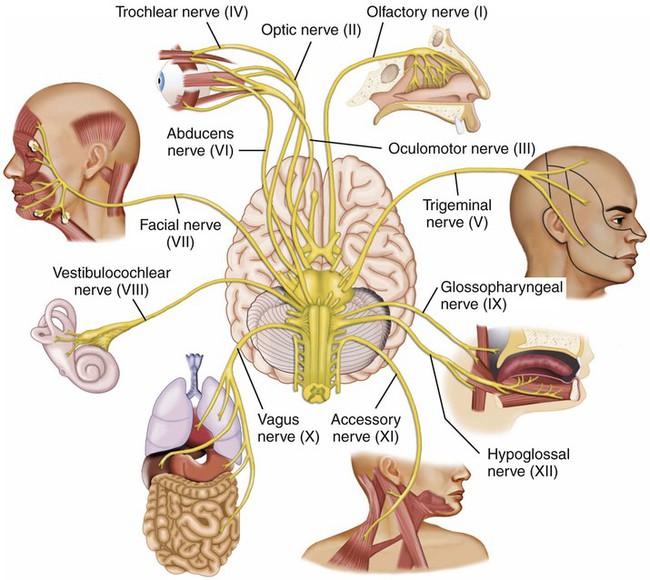
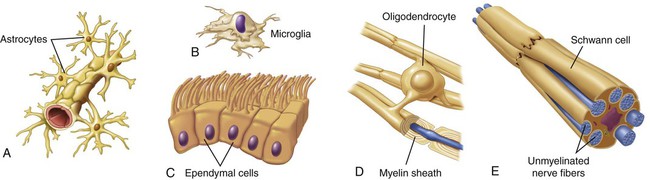
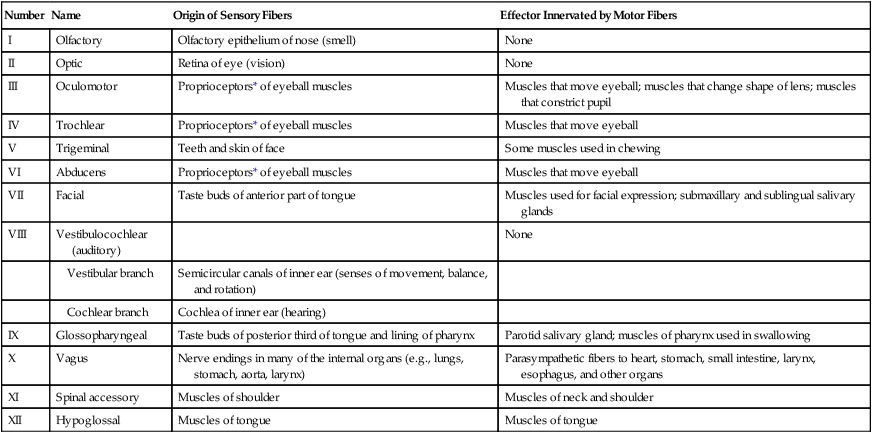
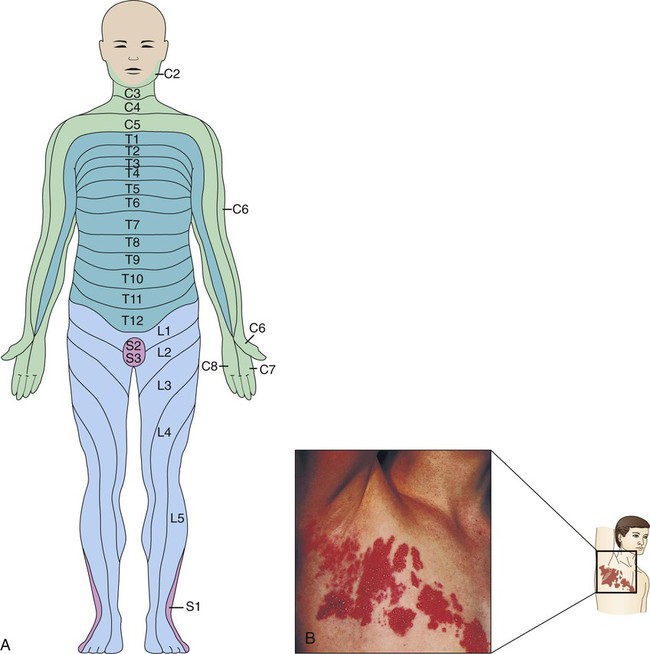
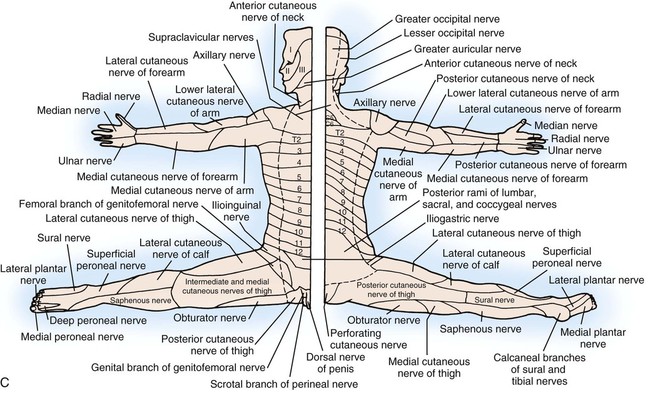
The nervous system is divided into two main systems. (See Figure 11-2 for a schematic of the divisions). The central nervous system (CNS) is composed of the brain and the spinal cord. It is the only site of nerve cells called interneurons, which connect sensory and motor neurons. The peripheral nervous system (PNS) is composed of the nerves that extend from the brain and spinal cord to the tissues of the body. These are organized into 12 pairs of cranial nerves and 31 pairs of spinal nerves. The PNS is further divided into sensory and motor nerves. Sensory (afferent) nerves carry impulses to the brain and spinal cord, whereas motor (efferent) nerves carry impulses away from the brain and spinal cord. PNS nerves are further categorized into two subsystems: Somatic nervous system (SNS): this system is voluntary in nature. These nerves collect information from and return instructions to the skin, muscles, and joints. Autonomic nervous system (ANS): mostly involuntary functions are controlled by this system as sensory information from the internal environment is sent to the CNS, and, in return, motor impulses from the CNS are sent to involuntary muscles: the heart, glands, and organs. The nervous system is made up of the following two types of cells: 1. Parenchymal cells, or neurons, the cells that carry out the work of the system. 2. Stromal cells, or glia, the cells that provide a supportive function. The basic unit of the nervous system is the nerve cell, or neuron (Fig. 11-3). Not all neurons are the same, but all have features in common. Dendrites, projections from the cell body, receive neural impulses, also called action potentials, from a stimulus of some kind. This impulse travels along the dendrite and into the cell body, which is the control center of the cell. This cell body contains the nucleus and surrounding cytoplasm. From the axon’s terminal fibers, the neurotransmitter is released from the cell to travel across the space between these terminal fibers and the dendrites of the next cell. This space is called the synapse (see Fig. 11-3). The impulse continues in this manner until its destination is reached. A nerve is a group of bundled axons in the PNS. Most nerves contain both sensory and motor fibers. The supportive, or stromal, glia are also called neuroglia (Fig. 11-4). They accomplish their supportive function by physically holding the neurons together and also protecting them. There are different kinds of neuroglia, including astrocytes, ependymal cells, oligodendroglia, microglia, and Schwann cells. Astrocytes connect neurons and blood vessels and form a structure called the blood-brain barrier (BBB), which prevents or slows the passage of some drugs and disease-causing organisms to the CNS. Ependymal cells line the ventricles of the brain and produce cerebrospinal fluid. Oligodendroglia cover the axons of neurons in the central nervous system, forming their myelin sheath. Microglia perform an active protective function by engulfing and ingesting infectious organisms. As stated previously, the CNS is composed of the brain and the spinal cord. The brain is one of the most complex organs of the body. It is divided into four parts: the cerebrum, the diencephalon, the brainstem, and the cerebellum (Fig. 11-5). The largest portion of the brain, the cerebrum, is divided into two halves, or hemispheres (Fig. 11-6). It is responsible for thinking, reasoning, and memory. The surfaces of the hemispheres are covered with gray matter and are called the cerebral cortex. Arranged into folds, the valleys are referred to as sulci (sing. sulcus), and the ridges are called the gyri (sing. gyrus). The cerebrum is further divided into sections called lobes, each of which has its own functions: 1. The frontal lobe contains the function of speech and the motor area that controls voluntary movement on the contralateral side of the body. It also is in charge of personality, emotions, and problem solving. 2. The temporal lobes contain the auditory and olfactory areas, and is where sequencing and memory occur. 3. The parietal lobes control the sensations of touch and taste, and also is control of spatial perception. 4. The occipital lobe is responsible for vision. 5. The insular lobes, located under the frontal and temporal lobes, are responsible for empathy, interceptive (internal sensing) awareness, and cognition. The term insula is derived from the Latin word meaning “island,” probably because it is not obviously continuous with the other lobes. Synonyms for insular lobe are the island of Reil and insular cortex. The spinal cord extends from the medulla oblongata to the first lumbar vertebra (Fig. 11-7). It then extends into a structure called the cauda equina (which means “horse’s tail” in Latin). The conus medullaris is the end of the spinal cord, whereas the cauda equina is the collection of nerve roots that extends from it. The meninges act as protective coverings for the CNS and are composed of three layers separated by spaces (Fig. 11-8). The dura mater is the tough, fibrous outer covering of the meninges. Its literal meaning is “hard mother.” The falx cerebri is the sickle-shaped fold between the hemispheres. The dura mater is classified as cranial dura mater and spinal dura mater. The tentorium cerebella is an extension of the dura mater that separates the cerebellum from the lower part of the occipital lobes. The diaphragm sellae is a small dural fold that covers the sella turcica; it has a small opening for the infundibulum of the pituitary. The space between the dura mater and arachnoid membrane is called the subdural space. If in the skull, it is the cranial subdural space; if in the spine, it is referred to as the spinal subdural space. Likewise, the subarachnoid space is further categorized as cranial subarachnoid and spinal subarachnoid spaces. The next layer is the arachnoid membrane, a thin, delicate membrane that takes its name from its spidery appearance. The subarachnoid space is the space between the arachnoid membrane and the pia mater. It contains cerebrospinal fluid (CSF), a clear fluid that protects the brain and spinal cord and removes waste products and monitors for internal changes. CSF is also present in cavities in the brain called ventricles. Finally, the pia mater is the thin, vascular membrane that is the innermost of the three meninges; its literal meaning is “soft mother.” The arachnoid and pia mater are referred to as leptomeninges for their slender appearance as opposed to the thick, tough nature of the dura mater. The peripheral nervous system is divided into: • 12 pairs of cranial nerves that conduct impulses between the brain and head, neck, thoracic, and abdominal areas, and • 31 pairs of spinal nerves that closely mimic the organization of the vertebrae and provide innervations to the rest of the body. The peripheral nerves are a combination of afferent (sensory) nerves and efferent (motor) nerves. The motor nerves are either voluntary or involuntary. The autonomic nervous system (ANS) consists of nerves that regulate involuntary function such as cardiac or smooth muscle. The ANS is further divided into the sympathetic and parasympathetic nervous systems, two opposing mechanisms that provide balance in the body: • The sympathetic nervous system is capable of producing a “fight-or-flight” response. This is the part of the nervous system that helps the individual respond to perceived stress. The heart rate and blood pressure increase, digestive processes slow, and sweat and adrenal glands increase their secretions. • The parasympathetic nervous system tends to do the opposite of the sympathetic nervous system—slowing the heart rate, lowering blood pressure, increasing digestive functions, and decreasing adrenal and sweat gland activity. This is sometimes called the “rest and digest” system. An example of a sensory response follows: Cranial nerves are named by their number and also their function or distribution. See Figure 11-9 and the table on the next page. *Proprioceptors are receptors located in muscles, tendons, or joints that provide information about body position and movement. • The olfactory bulb, the structure responsible for our sense of smell, is coded to the first cranial nerve, the olfactory nerve. • The optic chiasma is the area of the brain where the optic nerve fibers partially cross and is coded to the second cranial nerve, the optic nerve. If damage to the optic nerve fibers occurs before (proximal to) the chiasma, the patient will exhibit loss of vision on the same side of the lesion. If the damage occurs after (distal to) the chiasma, the vision in the opposite eye is affected because of the crossing. The optic chiasma is coded to the optic nerve. • The fifth cranial nerve, the trigeminal nerve, has three main branches: the ophthalmic nerve, the mandibular nerve, and the maxillary nerve. The ophthalmic nerve receives sensory information from several structures of the eye (except the retina) and the skin of the forehead and nose. The maxillary nerve receives information from the teeth of the upper jaw and the sinuses and skin of the midface. The mandibular nerve has both sensory and motor functions for the lower jaw. Each of these nerves arises from the Gasserian ganglion, also referred to as the trigeminal ganglion, which is a sensory ganglion. This collection of nerves is significant in that it is the site of a dormant herpes virus after a primary herpes infection. • The facial nerve, cranial nerve VII, has several structures coded to it that have word parts associated with the ear: the chorda tympani (named for its path through the middle ear) is actually involved in the perception of taste, the greater superficial petrosal nerve (innervates the lacrimal glands), the nerve to the stapes (innervates the muscle of one of the ossicles of the ear), the parotid plexus (the location of branching of the facial nerve at one of the salivary glands near the ear), and the posterior auricular nerve (provides sensation from and innervation to the external ear and occipital region of the head). Also coded to the facial nerve are the geniculate and submandibular ganglia. The geniculate ganglion, named for its bent knee appearance, is a mix of sensory, motor, and parasympathetic nerves that provide a sense of taste and innervates several glands in the head and neck. The submandibular ganglion is part of the autonomic nervous system as one of the four parasympathetic ganglia of the head and neck. • The vestibulocochlear nerve, cranial nerve VIII, is termed the acoustic nerve in PCS. Because its primary functions are balance and hearing, it’s not surprising that the vestibular (sensing positional information) and cochlear (carrying information about sound) nerves are coded to it. The vestibular ganglion (also called Scarpa’s ganglion) connects the vestibular nerve and semicircular canals of the inner ear. The spiral ganglion, a collection of nerve cells in the cochlea that sends sound to the cochlear nerve, is also coded to cranial nerve VIII. • The glossopharyngeal nerve, cranial nerve IX, is used to code the carotid sinus nerve and the tympanic nerve. The carotid sinus nerve supplies the area that is the small cavity at the beginning of the internal carotid artery, the carotid sinus, along with the structure of the carotid body. This nerve carries impulses that detect pressure and changes in pH in the carotid body. The tympanic nerve (also called Jacobson’s nerve) is a mix of sensory, parasympathetic, and sympathetic nerve fibers that serve the middle ear, the parotid gland, and the carotid plexus. • The last of the cranial nerves that require extra detail is the tenth cranial nerve, the vagus nerve. Coded to this nerve are the anterior and posterior vagal trunks that direct nerves to organs in the front and back of the body, along with the superior and recurrent (inferior) laryngeal nerves (serving the voice box) and the pharyngeal and pulmonary plexuses. The pharyngeal plexus has sensory and motor fibers for parts of the throat, whereas the pulmonary plexus supplies the lungs. If the nerve fibers from several spinal nerves form a network, it is termed a plexus. Collections of cell bodies in the PNS are referred to as ganglia (sing. ganglion). Spinal nerves are named by their location (cervical, thoracic, lumbar, sacral, and coccygeal) and by number. These nerves are either sensory (often referred to as cutaneous) or muscular. Dermatomes are skin surface areas supplied by a single afferent spinal nerve. These areas are so specific that it is actually possible to map the body by dermatomes (Fig. 11-10, A). This specificity can be demonstrated in patients with shingles, who show similar patterns as specific peripheral nerves are affected (Fig. 11-10, B). Myotomes are the areas of muscles that are supplied by a single efferent spinal nerve (Fig. 11-10, C). • Occipital nerves (greater, third, and sub-) are coded to cervical nerves that supply the skin and muscles of the head and neck. • Head and neck sympathetic nerves are used to code the ciliary, otic, sphenopalatine (also referred to as pterygopalatine), and submandibular (formerly called submaxillary) ganglia. The internal carotid plexus and the cavernous plexus are located near the internal carotid artery. The internal carotid plexus is lateral to it, whereas the cavernous plexus is inferior and medial to it. The stellate ganglion, named for its starlike appearance, is located in the lower part of the neck; it may be cut in order to control hyperhidrosis (excessive sweating) or Raynaud’s phenomenon. The cervical ganglia (inferior and superior) are sympathetic nerves in the neck area. • The median nerve is used to code the anterior interosseous and the palmar cutaneous nerve. • The radial nerve is used to code the dorsal digital, musculospiral, palmar cutaneous, and posterior interosseous nerves. • The intercostal, intercostobrachial, and subcostal nerves are coded to the thoracic nerve. Note that each incorporates the word part for the ribs (cost/o), which will help you locate these nerves to the chest. • Thoracic autonomic nerves are used to code the cardiac, esophageal, thoracic, and pulmonary plexuses. The superior, middle, and inferior cardiac nerves, which are part of the cardiac plexus, are coded as a thoracic sympathetic nerve. The greater, lesser, and least splanchnic nerves, which are sympathetic nerves to the organs within the thorax and the thoracic ganglion, part of the thoracic plexus, are also coded as a thoracic sympathetic nerve. • The abdominal sympathetic nerve is used to code a large number of plexuses, ganglia, and nerves. Fortunately, the word parts should be familiar to students who have completed the digestive system chapter. The celiac plexus (also called the solar plexus) and ganglion serve the belly, whereas the hepatic, gastric, renal, splenic, suprarenal, and pancreatic plexuses serve the liver, stomach, kidneys, spleen, adrenals, and pancreas respectively. The inferior and superior mesenteric plexuses and ganglia serve the mesentery, whereas the superior and inferior hypogastric plexuses serve the pelvic cavity. The myenteric plexus (also called Auerbach’s plexus) is the primary nervous supply to the digestive system and is responsible for gastric motility. The pelvic splanchnic nerves regulate the evacuation of the bowels and bladder. The submucous plexus, also called Meissner’s plexus, innervates smooth muscle, whereas the abdominal aortic plexus surrounds the abdominal aorta. • The superior clunic and the lumbosacral trunk are coded to the lumbar nerve. • The lumbar sympathetic nerve is used to code the lumbar ganglion and the lumbar splanchnic nerve. • The pudendal nerve is used to code the posterior labial or posterior scrotal nerves. • The sacral sympathetic nerve is used to code the ganglion impar (also called the ganglion of Walther), the pelvic and sacral splanchnic nerve, and the sacral ganglion. • The saphenous nerve is coded to the entry of the femoral nerve. • The tibial nerve is used to code the medial popliteal, medial sural cutaneous, and medial and lateral plantar nerves.
Nervous System
 Recognize and use terms related to the anatomy and physiology of the nervous system.
Recognize and use terms related to the anatomy and physiology of the nervous system.
 Recognize and use terms related to the pathology of the nervous system.
Recognize and use terms related to the pathology of the nervous system.
 Recognize and use terms related to the procedures for the nervous system.
Recognize and use terms related to the procedures for the nervous system.
Anatomy and Physiology
Organization of the Nervous System
Cells of the Nervous System
Neurons
Glia
The Central Nervous System
Brain (Encephalon)
Cerebrum
Spinal Cord
Meninges
The Peripheral Nervous System
Cranial Nerves
Number
Name
Origin of Sensory Fibers
Effector Innervated by Motor Fibers
I
Olfactory
Olfactory epithelium of nose (smell)
None
II
Optic
Retina of eye (vision)
None
III
Oculomotor
Proprioceptors* of eyeball muscles
Muscles that move eyeball; muscles that change shape of lens; muscles that constrict pupil
IV
Trochlear
Proprioceptors* of eyeball muscles
Muscles that move eyeball
V
Trigeminal
Teeth and skin of face
Some muscles used in chewing
VI
Abducens
Proprioceptors* of eyeball muscles
Muscles that move eyeball
VII
Facial
Taste buds of anterior part of tongue
Muscles used for facial expression; submaxillary and sublingual salivary glands
VIII
Vestibulocochlear (auditory)
None
Vestibular branch
Semicircular canals of inner ear (senses of movement, balance, and rotation)
Cochlear branch
Cochlea of inner ear (hearing)
IX
Glossopharyngeal
Taste buds of posterior third of tongue and lining of pharynx
Parotid salivary gland; muscles of pharynx used in swallowing
X
Vagus
Nerve endings in many of the internal organs (e.g., lungs, stomach, aorta, larynx)
Parasympathetic fibers to heart, stomach, small intestine, larynx, esophagus, and other organs
XI
Spinal accessory
Muscles of shoulder
Muscles of neck and shoulder
XII
Hypoglossal
Muscles of tongue
Muscles of tongue
Spinal Nerves
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree