Patient Story
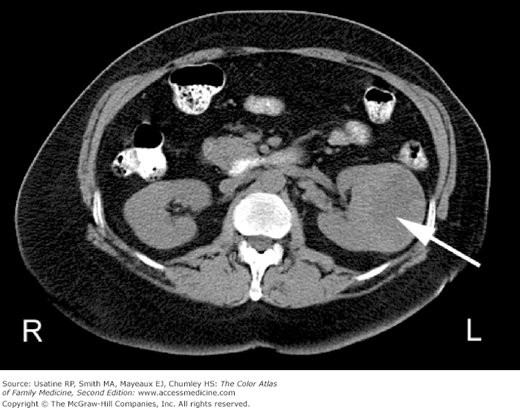
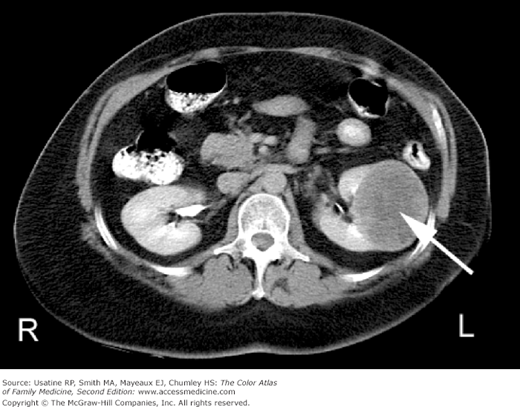
A 56-year-old man with hypertension presents with a 2-week history of left-sided flank pain. Urinalysis shows microscopic hematuria and a CT scan (Figures 71-1 and 71-2) demonstrates a solid left renal mass. Work-up for metastatic disease was negative. A biopsy confirmed renal cell carcinoma and a radical nephrectomy was performed.
Figure 71-2
CT with contrast in the same patient shows the solid hypodense renal cell carcinoma mass (arrow) in the left kidney and contrasting normal parenchyma. The contrast is taken up better by the remaining normal kidney tissue and the tumor becomes more visible. (Courtesy of Michael Freckleton, MD.)
Introduction
Renal tumors are a heterogeneous group of kidney neoplasms derived from the various parts of the nephron. Each type of tumor possesses distinct genetic characteristics, histologic features, and, to some extent, clinical phenotypes that range from benign (approximately 20% of small masses) to high-grade malignancy. Ninety percent to 95% of kidney neoplasms are renal cell carcinomas (RCCs).1,2
Epidemiology
- RCC comprises 2% to 3% of all malignant diseases in adults and is the seventh most common cancer in men and ninth most common cancer in women.2
- An estimated 60,920 cases were diagnosed and approximately 13,120 deaths occurred in 2011 from kidney and renal pelvis cancer.3 The age-adjusted incidence rate was 14.6 per 100,000 persons with a median age at diagnosis of 64 years.3
- Lifetime risk of kidney and renal pelvis cancer is 1.56% (1 in 63 people will be diagnosed during their lifetime).3 These cancers are more common in men than women (approximately 2:1).
- Approximately 2% to 3% of cases are familial (e.g., von Hippel-Lindau syndrome).2
- Metastatic disease at presentation occurs in 23% to 33%; the most common sites of distant metastases (in descending order) are lung (with or without mediastinal or hilar nodes), bone, upper abdomen (including the tumor bed, adrenal gland, contralateral kidney, and liver), brain, and other sites (e.g., skin, spleen, heart, diaphragm, gut, connective tissue, and pancreas).4
Etiology and Pathophysiology
- Clear cell carcinoma (from high lipid content) (60% to 80%).
- Papillary carcinoma (5% to 15%), further delineated into type 1 and the more aggressive type 2.
- Chromophobic tumors (3% to 10%) and other rare subtypes, such as medullary, which occurs almost exclusively in patients with sickle cell trait.
Risk Factors
Diagnosis
Most presentations are incidental (identified during other tests) and, consequently, although the incidence has increased, more cancers are diagnosed at early stages.2 Despite this fact, mortality rates have also increased.
- Hematuria (40%) and flank pain (40%).
- Weight loss and anemia (approximately 33%).
- Flank mass (approximately 25%).
- The classic triad of hematuria, flank pain, and flank mass occurs in 5% to 10% of patients.1
- Other reported symptoms include night sweats, bone pain, fatigue, and sudden onset of left varicocele.
- Systemic symptoms may be caused by metastases or paraneoplastic syndromes, such as parathyroid hormone-related protein (causing hypercalcemia and renal stones), renin (causing hypertension), or erythropoietin (causing erythrocytosis).2
Potentially useful studies: SOR C
- Hemoglobin (anemia).
- Liver chemistries (metastatic disease or paraneoplastic syndrome).
- Urinalysis (hematuria—gross or microscopic).
- Urine cytology (neoplastic cells).
- The National Comprehensive Cancer Network (NCCN) also suggests a metabolic panel including lactate dehydrogenase (LDH) as part of the initial work-up.5
- The work-up for indeterminate renal masses suggested by the American College of Radiology (ACR) includes either CT scan of the abdomen (Figures 71-1, 71-2, and 71-3) (solid renal mass; signs suggestive of renal vein or caval thrombus include filling defects, enlargement of the vessel, and rim enhancement) or abdominal MRI (slightly more sensitive and tends to upgrade cystic lesions; Figure 71-4); either scan should be done without and with contrast.6
- An ultrasound (US) of the kidney retroperitoneal may help to clarify a mass that is probably a hyperdense cyst (the most common renal mass).
- Angiography may be used to define vascular anatomy before nephron-sparing surgery.6
For the purpose of staging a RCC, ACR recommends:6
- Multidetector CT without and with contrast.
- Chest X-ray (CXR, tumor may extend into the hilar lymph nodes) or chest CT.
- MRI if patient is unable to undergo CT with contrast.
- Bone scans and brain MRI should be reserved for patients with abnormal blood chemistries, symptoms, or large and locally aggressive or metastatic primary renal cancers.
A renal biopsy is only needed on occasion based on the appearance and size of the mass; US, CT, or MRI can be used for image guidance.4 ACR indications for biopsy include:
- Confirming an infected cyst.
- Identifying lymphoma.
- Determining a metastasis.
- Confirming RCC in certain circumstances, including prior to ablative therapies.
Differential Diagnosis
- Simple cysts.
- Renal calculi/nephrolithiasis (see Chapter 68, Kidney Stones).
- Benign neoplasms (infrarenal hematoma, adenoma, angiomyolipoma [see Figure 71-4

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree