Reactive Paracortical Hyperplasia
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Predominantly T-cell response commonly seen in viral and drug-related lymphadenopathies
Clinical Issues
Patients typically present with enlarged lymph nodes, either localized or widespread
Systemic symptoms can be present
Size, location, and consistency of lymph nodes, as well as age and duration, are important factors in identifying etiology
Microscopic Pathology
Overall lymph node architecture is preserved
Paracortical areas are markedly expanded by heterogeneous population of cells
Small lymphocytes, histiocytes, and immunoblasts
Immunoblasts are large with prominent nucleoli
Can resemble Hodgkin or Reed-Sternberg cells
CD30(+), CD45(+), CD15(-)
Ancillary Tests
Normal T-cell immunophenotype
No evidence of monoclonal IgH or T-cell receptor gene rearrangements
Top Differential Diagnoses
Dermatopathic lymphadenopathy
Anaplastic large cell lymphoma
Myeloid sarcoma
Marginal zone B-cell lymphoma
Hodgkin lymphoma
T-cell/histiocyte-rich large B-cell lymphoma
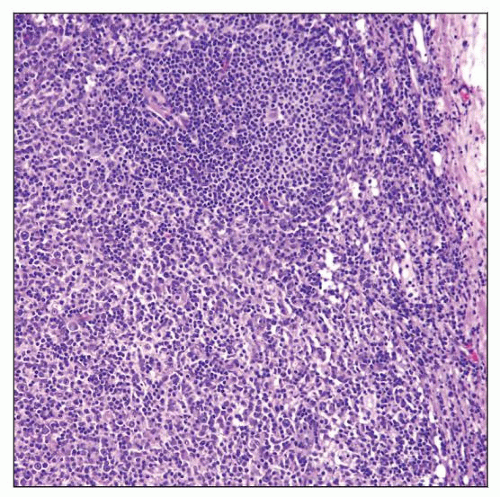 Lymph node with reactive parafollicular hyperplasia demonstrates that the paracortical (interfollicular) area is markedly expanded. A residual follicle is at the top of the field. |
TERMINOLOGY
Abbreviations
Reactive paracortical hyperplasia (RPH)
Synonyms
Diffuse paracortical lymphoid hyperplasia
Interfollicular hyperplasia, T-zone hyperplasia
Definitions
RPH is benign reaction, predominantly within paracortical regions of lymph node; manifestation of T-cell immunological response
Also occurs in extranodal lymphoid tissues
Often occurs as part of mixed reactive hyperplasia pattern
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Variety of environmental pollutants and chemicals can cause paracortical hyperplasia
Therapeutic agents (drugs) are an important cause
Phenytoin (Dilantin) and other antiseizure medications
Vaccine administration
Vaccinia
Measles (live, attenuated)
Usually arises 1-3 weeks after vaccination
Infectious Agents
Viral infection is common cause of RPH
Epstein-Barr virus (EBV)
Cytomegalovirus
Herpes simplex virus (type 1 or 2)
Necrosis is usually present in viral infection
CLINICAL ISSUES
Presentation
Patients present with enlarged lymph nodes, either localized or widespread
Systemic symptoms can be present
Fever, fatigue, and weight loss
Laboratory abnormalities may be present
Leukocytosis, lymphocytosis
Clues to etiology derived from
Patient age, duration of symptoms, and site
Size and consistency of lymph node(s)
Treatment
Localized lymph node enlargement in absence of other symptoms can be followed
If no resolution after 3-4 weeks, investigation is needed
Generalized lymphadenopathy is cause for concern
Immediate investigation for etiology is usually pursued
Prognosis
Self-limiting and reversible process with no impact on survival
Depends, in part, on underlying cause
Can be associated with other diseases (e.g., autoimmune diseases, malignancy)
IMAGE FINDINGS
Radiographic Findings
Lymphadenopathy, localized or generalized
MACROSCOPIC FEATURES
MICROSCOPIC PATHOLOGY
Histologic Features
Overall lymph node architecture is distorted but preserved
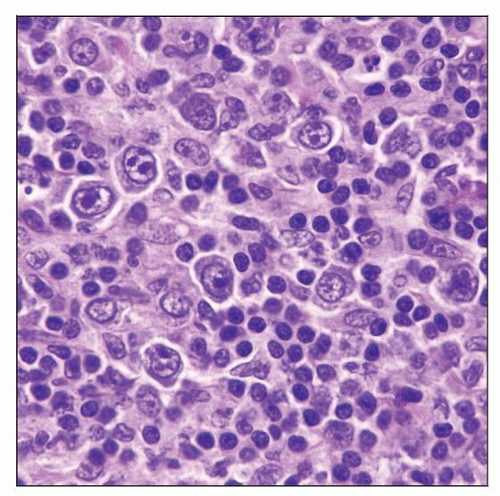
Paracortical areas are markedly expanded by heterogeneous cell population
Immunoblasts in sea of small lymphocytes (mostly T cells) and histiocytes
Imparts a mottled or “moth-eaten” pattern at scanning magnification
Immunoblasts are large with vesicular nuclei and central nucleoli
Nucleoli are basophilic, often with trapezoidal shape
Nucleoli often have thin attachments to nuclear membrane (“spider legs”)
Can resemble Hodgkin or Reed-Sternberg (HRS) cells
Can form sheets in some cases (raising differential diagnosis of large cell lymphoma)
Eosinophils can be prominent
Particularly in hypersensitivity causes (e.g., drug reactions)
High endothelial venules often present
Other lymph node components can be reactive (so-called mixed pattern)
Reactive follicles
Monocytoid B-cell hyperplasia in sinuses
Nodules of plasmacytoid dendritic cells
Predominant Pattern/Injury Type
Lymphoid, interfollicular
Predominant Cell/Compartment Type
Lymphadenopathy
ANCILLARY TESTS
Immunohistochemistry
Small lymphocytes are usually immunophenotypically normal T cells
Positive for pan-T-cell antigens (CD3, CD5, CD7, CD43); CD4(+) and CD8(+) subsets
Immunoblasts can be of either T-cell or B-cell lineage
CD30(+), CD45(+), CD15(-)
Evidence of virus in EBV-associated cases
Positive for EBV-LMP
Flow Cytometry
Numerous T cells with normal immunophenotype
Fewer polytypic B cells
In Situ Hybridization
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree