Reactive Follicular Hyperplasia
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Benign, reversible process characterized by hyperplastic secondary lymphoid follicles
Clinical Issues
Enlarged lymph nodes, localized or widespread
± systemic symptoms: Fever, fatigue, weight loss
Age and duration are important clues for etiology
Lymph node size, location, and consistency can suggest likely etiologic agent
Microscopic Pathology
Numerous enlarged follicles, varying in size and shape, with occasional coalescence of follicles
Reactive follicles have central germinal centers and peripheral, sharply demarcated mantle zones
Ancillary Tests
Germinal center and mantle zone B cells express polytypic Igs and pan-B markers
Germinal center centrocytes and centroblasts are CD10(+), Bcl-6(+), and Bcl-2(-)
No monoclonal IgH gene rearrangements
No evidence of t(14;18)(q32;q21) or IgH-BCL2 fusion sequences
Top Differential Diagnoses
Follicular lymphoma
Atypical follicular hyperplasia
Progressive transformation of germinal centers
Nodular lymphocyte predominant Hodgkin lymphoma
Lymphocyte-rich classical HL, nodular variant
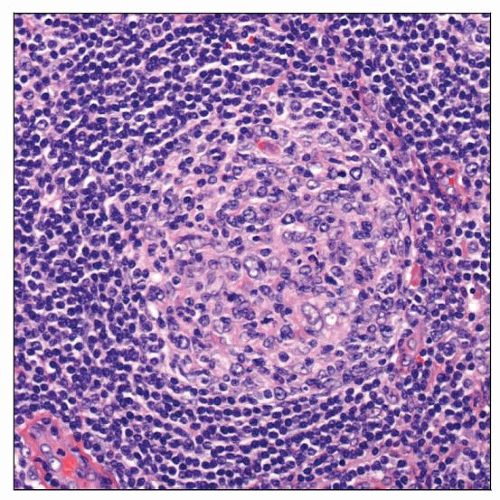 A hyperplastic lymphoid follicle is seen with a central, prominent germinal center and a peripheral, sharply demarcated mantle zone. |
TERMINOLOGY
Abbreviations
Reactive follicular hyperplasia (RFH)
Synonyms
Follicular hyperplasia
Definitions
Benign, reversible process characterized by marked proliferation of hyperplastic lymphoid follicles
Hyperplastic follicles have prominent germinal centers (so-called secondary follicles)
Characteristic of humoral immune reaction involving stimulation and proliferation of B cells
Usually involves lymph nodes but can affect extranodal organs
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Variety of drugs, chemicals, and environmental pollutants can cause RFH
Infectious Agents
Most common cause of RFH is bacterial infection
Fungi, parasites, and viruses also can cause RFH, either pure or as part of mixed reactive pattern
Others
In many cases, etiology of RFH cannot be identified
CLINICAL ISSUES
Presentation
Patients typically present with enlarged lymph nodes, either localized or widespread
Systemic symptoms, such as fever, fatigue, and weight loss, may be present
Laboratory abnormalities, such as leukocytosis, neutrophilia, or lymphocytosis, are common with infections and may be present
Lymph node size is important
Small, shotty lymph nodes in asymptomatic patients are within normal limits
Lymph nodes ≥ 1 cm in diameter are abnormal
Painful lymph nodes are more often related to inflammation or hemorrhage
Age and duration are important in identifying etiology
Location and consistency can suggest most likely etiologic agent
Location, as related to likely causes of lymphadenopathy
Cervical: Infectious mononucleosis
Posterior cervical: Toxoplasmosis
Parotid, submaxillary, epitrochlear: HIV infection
Cervical and axillary: Cat scratch disease
Inguinal: Sexually transmitted diseases
Supraclavicular: Often associated with malignant diseases, especially in older patients
Consistency, as related to likely causes of lymphadenopathy
Soft: Inflammatory
Fluctuant: Suppurative infection (often bacterial or fungal)
Matted: Tuberculosis, lymphogranuloma venereum, cancer
Firm to hard: Malignancy, including lymphoma or metastatic carcinoma
Treatment
Localized lymph node enlargement in absence of other symptoms requires follow-up for 3-4 weeks
If lymphadenopathy does not resolve, additional investigation is likely needed
Generalized lymphadenopathy usually requires immediate investigation for etiology
Prognosis
Benign, reversible process with no impact on patient survival
Can be associated with other diseases such as autoimmune disease or malignancy
MICROSCOPIC PATHOLOGY
Histologic Features
Numerous enlarged follicles, varying in size and shape, with occasional coalescence of follicles
In lymph nodes, reactive follicles usually prominent in cortex, with lesser involvement of other lymph node compartments
In spleen, reactive follicles are located in white pulp
Reactive follicles: Have central germinal centers and peripheral, sharply demarcated mantle zones
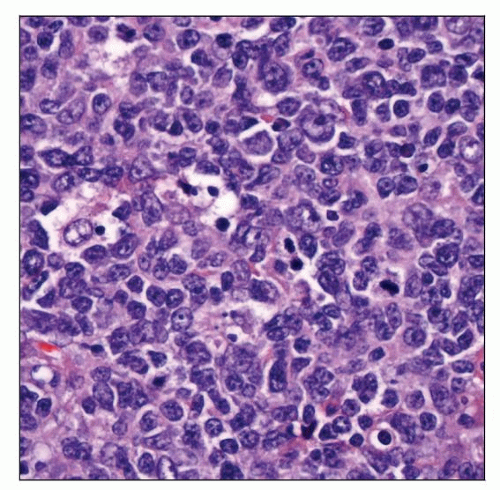
Germinal centers: Composed of centrocytes, centroblasts, follicular dendritic cells (FDC), T cells, and macrophages/histiocytes
Centroblasts: 3-4x size of small lymphocytes with large vesicular nuclei, 1-3 peripheral nucleoli, frequent mitoses, and rim of cytoplasm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree