Pulmonary drug delivery
Kevin M.G. Taylor
Chapter contents
Inhalation aerosols and the importance of size distribution
Particle deposition in the airways
Formulating and delivering therapeutic inhalation aerosols
Pressurized metered-dose inhalers
Methods of aerosol size analysis
Cascade impactors and impingers
Key points
• Pulmonary delivery may be used for drugs having local or systemic activity.
• Nebulizers deliver relatively large doses of drugs, as either aqueous solutions or suspensions.
Inhaled drug delivery
Therapeutic agents for the treatment or prophylaxis of airways diseases, such as bronchial asthma, chronic obstructive pulmonary disease (COPD) and cystic fibrosis are usually delivered directly to the respiratory tract. The administration of a drug at its site of action can result in a rapid onset of activity, which may be highly desirable, for instance when delivering bronchodilating drugs for the treatment of asthma. Additionally, smaller doses can be administered locally compared to delivery by the oral or parenteral routes, thereby reducing the potential incidence of adverse systemic effects and reducing drug costs. The pulmonary route is also useful where a drug is poorly absorbed orally, e.g. sodium cromoglicate, or where it is rapidly metabolized orally, e.g. isoprenaline. The avoidance of first-pass metabolism in the liver may also be advantageous, although the lung itself has some metabolic capability.
The lung may also be used as a route for delivering drugs having systemic activity, because of its large surface area, the abundance of capillaries and the thinness of the air–blood barrier. This has been exploited in the treatment of migraine with ergotamine, and the potential for delivering biopharmaceuticals, such as insulin, vaccines and growth hormone via the airways is now well established.
Lung anatomy
The lung is the organ of external respiration, in which oxygen and carbon dioxide are exchanged between blood and inhaled air. The structure of the airways also efficiently prevents the entry, and promotes removal of airborne foreign particles, including microorganisms.
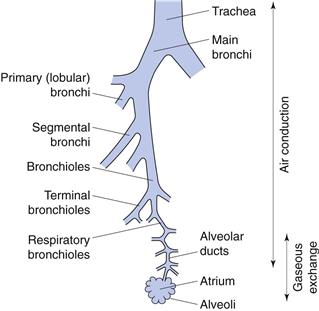
The respiratory tract can be considered as comprising conducting (central) regions (trachea, bronchi, bronchioles, terminal and respiratory bronchioles) and respiratory (peripheral) regions (respiratory bronchioles and alveolar regions), although there is no clear demarcation between them (Fig. 37.1). The upper respiratory tract comprises the nose, throat, pharynx and larynx; the lower tract comprises the trachea, bronchi, bronchioles and the alveolar regions. Simplistically, the airways can be described by a symmetrical model in which each airway divides into two equivalent branches or generations. In fact, the trachea (generation 0) branches into two main bronchi (generation 1), of which the right bronchus is wider and leaves the trachea at a smaller angle than the left, and hence is more likely to receive inhaled material. Further branching of the airways ultimately results in terminal bronchioles. These divide to produce respiratory bronchioles, which connect with alveolar ducts leading to the alveolar sacs (generation 23). These contain approximately 2–6 × 108 alveoli, producing a surface area of 100–140 m2 in an adult male.
The conducting airways are lined with ciliated epithelial cells. Insoluble particles deposited on the airways walls in this region are trapped by the mucus, swept upwards from the lungs by the beating cilia to the throat, and are swallowed.
Inhalation aerosols and the importance of size distribution
To deliver a drug into the airways, it must be presented as an aerosol (with the exception of medical gases). In pharmacy, an aerosol is defined as a two-phase system of solid particles or liquid droplets dispersed in air or other gaseous phase, having sufficiently small size to display considerable stability as a suspension.
The deposition of a drug/aerosol in the airways is dependent on four factors: the physicochemical properties of the drug, the formulation, the delivery/liberating device, and the patient (breathing patterns and clinical status).
The most fundamentally important physical property of an aerosol for inhalation is its size. The particle size of an aerosol is usually standardized by calculation of its aerodynamic diameter, da, which is the physical diameter of a unit density sphere which settles through air with a velocity equal to the particle in question. Therapeutic aerosols are heterodispersed (polydispersed) and the distribution of sizes is generally represented by the geometric standard deviation (GSD or σg), when the size is log-normally distributed.
For approximately spherical particles:
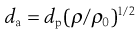 (37.1)
(37.1)
where dp is physical diameter, ρ is particle density and ρ0 is unit density, i.e. 1 g/cm3.
When dp is the mass median diameter (MMD), da is termed the mass median aerodynamic diameter (MMAD).
Large porous particles, with large physical diameters of the order of 20 µm are efficiently delivered to and deposited in the lungs. Their low density, due to the porous or hollow nature of their structure means such particles have a small aerodynamic diameter and are thus carried in the inspired air, deep into the lungs. Additionally, large particles are less prone to aggregation than smaller ones (see below) offering formulation advantages and the particles are too large to be cleared from the airways by alveolar macrophages.
Influence of environmental humidity on particle size
As a particle enters the respiratory tract, the change from ambient to high relative humidity (approximately 99%) results in condensation of water on to the particle surface, which continues until the vapour pressure of the water equals that of the surrounding atmosphere. For water-insoluble materials, this results in a negligibly thin film of water; however, with water-soluble materials a solution is formed on the particle surface. As the vapour pressure of the solution is lower than that of pure solvent at the same temperature, water will continue to condense until equilibrium between vapour pressures is reached, i.e. the particle will increase in size. The final equilibrium diameter is constrained by the Kelvin effect, i.e. the vapour pressure of a droplet solution is higher than that for a planar surface, and is a function of the particle’s original diameter. Hygroscopic growth will affect the deposition of particles, resulting in deposition higher in the respiratory tract than would have been predicted from measurements of their initial size.
Particle deposition in the airways
The efficacy of a therapeutic aerosol is dependent on its ability to penetrate the respiratory tract and be deposited. To penetrate to the peripheral (respiratory) regions, aerosols require a size less than about 5 or 6 µm, with less than 2 µm being preferable for alveolar deposition. Literature values for ‘respirable’ size vary and must be considered alongside the environmental changes in size described above and the heterodispersed nature of inhalation aerosol size distributions. Larger particles or droplets are deposited in the upper respiratory tract and are rapidly removed from the lung by the mucociliary clearance process. As a consequence, the drug becomes available for systemic absorption and may potentially cause adverse effects. Steroid aerosols of sufficiently large size may deposit in the mouth and throat, with the potential to cause adverse effects, including oral candidiasis. The size of aerosolized drug may be especially important in the treatment of certain conditions where penetration to the peripheral airways is particularly desirable, for instance the treatment and prophylaxis of the alveolar infection Pneumocystis carinii pneumonia.
There are three main mechanisms responsible for particulate deposition in the lung: gravitational sedimentation, impaction and diffusion.
Inertial impaction
The air stream changes direction in the throat, or where a bifurcation occurs in the respiratory tract. Particles within the air stream, having sufficiently high momentum, will impact on the airways’ walls rather than following the changing air stream. This deposition mechanism is particularly important for large particles having a diameter greater than 5 µm, and particularly greater than 10 µm, and is common in the upper airways, being the principal mechanism for deposition in the nose, mouth, pharynx and larynx and the large conducting airways. With the continuous branching of the conducting airways, the velocity of the air stream decreases and impaction becomes a less important mechanism for deposition.
The probability of impaction is proportional to:
 (37.2)
(37.2)
where θ is the change in airways direction, V is air stream velocity and r is the airway’s radius. Vt is the terminal settling velocity (see Eqn 37.3).
Gravitational sedimentation
From Stokes’ Law, particles settling under gravity will attain a constant terminal settling velocity, Vt:
 (37.3)
(37.3)
where ρ is particle density, g is the gravitational constant, d is particle diameter and η is air viscosity.
Thus, gravitational sedimentation of an inhaled particle is dependent on its size and density, in addition to its residence time in the airways. Sedimentation is an important deposition mechanism for particles in the size range 0.5–3 µm, in the small airways and alveoli, for particles that have escaped deposition by impaction.
Brownian diffusion
Collision and bombardment of small particles by molecules in the respiratory tract produce Brownian motion. The resultant movement of particles from high to low concentrations causes them to move from the aerosol cloud to the airways’ walls. Diffusion is inversely proportional to particle size. It is the predominant mechanism for particles smaller than 0.5 µm, with the rate of diffusion, given by the Stokes-Einstein equation:
 (37.4)
(37.4)
where D is the diffusion coefficient, kB is the Boltzmann’s constant, T is the absolute temperature, η is viscosity and d is particle diameter.
Other mechanisms of deposition
Although impaction, sedimentation and diffusion are the most important mechanisms for drug deposition in the respiratory tract, other mechanisms may occur. These include interception, whereby particles having extreme shapes, such as fibres, physically catch on to the airways’ walls as they pass through the respiratory tract, and electrostatic attraction, whereby an electrostatic charge on a particle induces an opposing charge on the walls of the respiratory tract, resulting in attraction between particle and walls.
Effect of particle size on deposition mechanism
Different deposition mechanisms are important for different sized particles. Those greater than 5 µm will deposit predominantly by inertial impaction in the upper airways. Particles sized between 1 and 5 µm deposit predominantly by gravitational sedimentation in the lower airways, especially during slow, deep breathing and particles less than 1 µm deposit by Brownian diffusion in the stagnant air of the lower airways. Particles of approximately 0.5 µm are inefficiently deposited, being too large for effective deposition by Brownian diffusion and too small for effective impaction or sedimentation, and they are often quickly exhaled. This size of minimum deposition should thus be considered during formulation, although for the reasons of environmental humidity discussed previously, the equilibrium diameter in the airways may be significantly larger than the original particle size in the formulation.
Breathing patterns
Patient-dependent factors, such as breathing patterns, lung physiology and the presence of pulmonary disease also affect particle deposition. For instance, the larger the inhaled volume, the greater the peripheral distribution of particles in the lung, whilst increasing inhalation flow rate enhances deposition in the larger airways by inertial impaction. Breath-holding after inhalation increases the deposition of particles by sedimentation and diffusion. Optimal aerosol deposition occurs with slow, deep inhalations to total lung capacity, followed by breath-holding prior to exhalation. It should be noted that changes in the airways resulting from disease states, for instance airways’ obstruction, may affect the deposition profile of an inhaled aerosol.
Clearance of inhaled particles and drug absorption
Particles deposited in the ciliated conducting airways are cleared by mucociliary clearance within 24 hours and are ultimately swallowed. The composition of mucus and the process of mucociliary clearance are discussed in Chapter 38. Insoluble particles penetrating to the alveolar regions, and which are not solubilized in situ, are removed more slowly. Alveolar macrophages engulf such particles and may then migrate to the bottom of the mucociliary escalator, or alternatively may be removed via the lymphatics. The clearance of particle-loaded macrophages occurs over a period of days or weeks.
Hydrophobic compounds are usually absorbed at a rate dependent on their oil/water partition coefficients, whereas hydrophilic materials are poorly absorbed through membrane pores at rates inversely proportional to molecular size. Thus, the airways’ membrane, like the gastrointestinal tract, is preferably permeable to the unionized form of a drug. Some drugs, such as sodium cromoglicate, are partly absorbed by a saturable active transport mechanism, whilst large macromolecules may be absorbed by transcytosis. The rate of drug absorption, and consequently drug action, can be influenced by the formulation. Rapid drug action can generally be achieved using solutions or powders of aqueous soluble salts, whereas slower or prolonged absorption may be achieved using suspension formulations, powders of less soluble salts or novel drug delivery systems such as liposomes and microspheres.
Formulating and delivering therapeutic inhalation aerosols
There are currently three main types of aerosol-generating device for use in inhaled drug therapy: pressurized metered-dose inhalers, dry powder inhalers and nebulizers.
Pressurized metered-dose inhalers
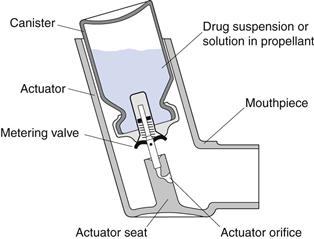
Pressurized metered-dose inhalers (pMDIs), also referred to as metered-dose inhalers (MDIs), were introduced in the mid-1950s and are the most commonly used inhalation drug delivery devices. In pMDIs, drug is either dissolved or suspended in liquid propellant(s) together with other excipients, including surfactants, and presented in a pressurized canister fitted with a metering valve (Fig. 37.2). A predetermined dose is released as a spray on actuation of the metering valve. When released from the canister, the formulation undergoes volume expansion in the passage within the valve and forms a mixture of gas and liquid before discharge from the orifice. The high-speed gas flow helps to break up the liquid into a fine spray of droplets.
Containers
Pharmaceutical aerosols may be packaged in tin-plated steel, plastic-coated glass or aluminium containers. In practice, pMDIs are generally presented in aluminium canisters, produced by extrusion to give seamless containers with a capacity of 10–30 mL. Aluminium is relatively inert and may be used uncoated where there is no chemical instability between container and contents. Alternatively, aluminium containers with an internal coating of a chemically resistant organic material, such as an epoxy resin or polytetrafluoroethylene (PTFE), can be used.
Propellants
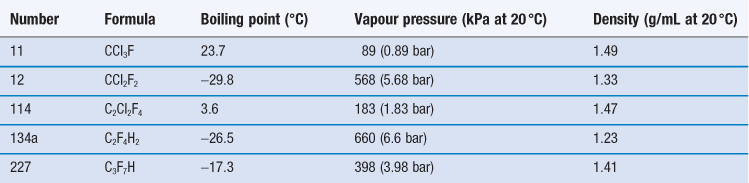
The propellants used in pMDI formulations are liquefied gases, traditionally chlorofluorocarbons (CFCs) which are now largely replaced by hydrofluoroalkanes (HFAs). At room temperature and pressure, these are gases but they are readily liquefied by decreasing temperature or increasing pressure. The head space of the aerosol canister is filled with propellant vapour, producing the saturation vapour pressure at that temperature. On spraying, medicament and propellant are expelled and the head volume increases. To reestablish the equilibrium, more propellant evaporates and so a constant pressure system with consistent spray characteristics is produced. The CFCs currently employed in pMDI formulations are trichlorofluoromethane (CFC-11), dichlorodifluoromethane (CFC-12) and dichlorotetrafluoroethane (CFC-114). Formulations generally comprise blends of CFC-11 and CFC-12 or CFC-11, CFC-12 and CFC-114 (Table 37.1), together with a surfactant such as a sorbitan ester, oleic acid or lecithin, which acts as a suspending agent and lubricates the valve.
CFCs and HFAs are numbered using a universal system. The first digit is the number of carbon atoms minus 1 (omitted if zero), the second is the number of hydrogen atoms plus 1, and the third is the number of fluorine atoms. Chlorine fills any remaining valencies, given the total number of atoms required to saturate the compound. If asymmetry is possible, this is designated by a letter. The symmetrical isomer is assigned the number described above; of the asymmetrical isomers, that designated the letter a is the most symmetrical, b the next most symmetrical, and so on. The CFCs are perfectly miscible with each other and suitable blends give a useful intermediate vapour pressure, usually about 450 kPa. The vapour pressure of the mixture of propellants is given by Raoult’s Law, i.e. the vapour pressure of a mixed system is equal to the sum of the mole fraction of each component multiplied by its vapour pressure:
 (37.5)
(37.5)
where P is the total vapour pressure of the system and pa and pb are the partial vapour pressures of the components, a and b:
 (37.6)
(37.6)
 (37.7)
(37.7)
where xa and xb are the mole fractions and  and
and  are the partial vapour pressures of components a and b, respectively.
are the partial vapour pressures of components a and b, respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree